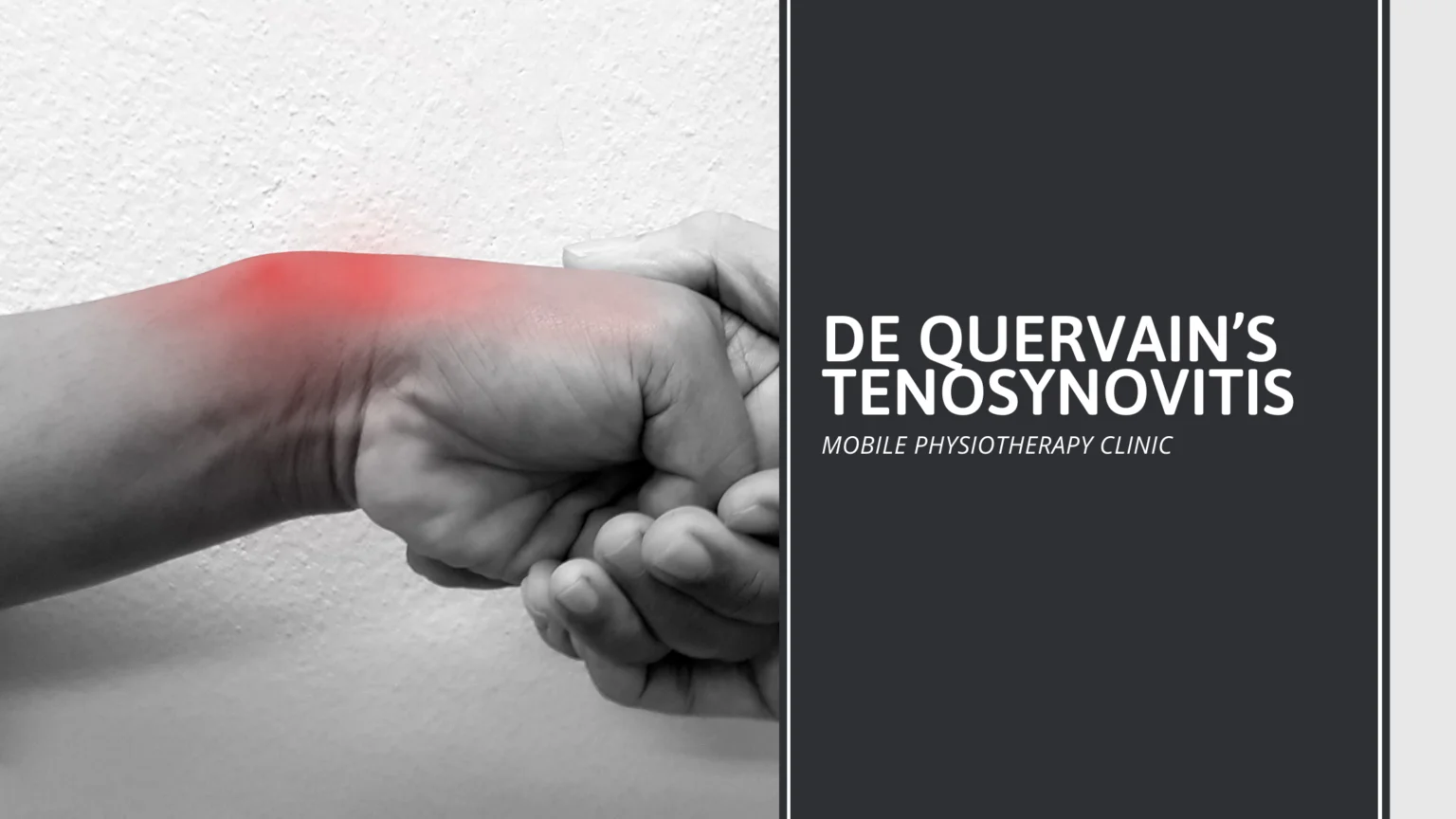
De Quervain’s Tenosynovitis
De Quervain’s tenosynovitis is also known as texting thumb, gamer’s thumb, washerwoman’s sprain, radial styloid tenosynovitis, de Quervain disease, de Quervain’s tenosynovitis, de Quervain’s stenosing, designer’s thumb, tenosynovitis, mother’s wrist, mommy thumb.
De Quervain’s tenosynovitis is a painful condition affecting the tendons on the thumb side of your wrist. If you have de Quervain’s tenosynovitis, it will probably hurt when you turn your wrist, grasp anything or make a fist.
Although the exact cause of de Quervain’s tenosynovitis isn’t known, any activity that relies on repetitive hand or wrist movement — such as working in the garden, playing golf or racket sports, or lifting your baby — can make it worse.
Table of Contents
Symptoms of De Quervain’s Tenosynovitis
Pain: Pain may be felt over the thumb side of the wrist. This is the main symptom. The pain may appear either gradually or suddenly. Pain is felt in the wrist and can travel up the forearm. The pain is usually worse when the hand and thumb are in use. This is especially true when forcefully grasping objects or twisting the wrist.
Swelling: Swelling may be seen over the thumb side of the wrist. This swelling may accompany a fluid-filled cyst in this region.
Sensation: A “catching” or “snapping” sensation may be felt when moving the thumb.
Difficult to move: Pain and swelling may make it difficult to move the thumb and wrist.
Causes of De Quervain’s Tenosynovitis
Doctors often don’t know why you get De Quervain’s Tenosynovitis. But it does result from:
- A direct blow to the thumb
- Gaming
- Hobbies like gardening or racket sports
- Inflammatory conditions like rheumatoid arthritis
- Overuse
- Repetitive workplace tasks
Who get De Quervain’s Tenosynovitis
Anyone can get De Quervain’s Tenosynovitis. But these things make it more likely:
- Age: Adults between 30 and 50 are most likely to get it.
- Gender: Women are 8 to 10 times more likely to get it than men.
- Motherhood: It often happens just after pregnancy. Lifting your little bundle of joy repeatedly might bring it on.
Motions: You can get the condition if you move your wrist over and over again, whether it’s for fun or for work.
Risk Factors of De Quervain’s Tenosynovitis
Although the majority of patients with de Quervain tenosynovitis are women between 30 and 50 years old, this condition can affect anyone at any age. There are several factors that can contribute to the swelling of the thumb tendons and increase the risk for developing de Quervain tenosynovitis:
- Repetitive activities with thumb and wrist, such as wringing out clothes, hammering, skiing, knitting
- Lifting heavy objects
- Chronic illnesses such as rheumatoid arthritis and diabetes
- Pregnancy
Preventions of De Quervain’s Tenosynovitis
The best way to prevent de Quervain’s tenosynovitis is by avoiding repetitive movements. Change your actions to reduce the stress on your wrists. Take frequent breaks to rest if you are using your wrists. Wear a brace or splint on your thumb and wrist, if necessary.
Follow the exercise routine suggested by your doctor or physical therapist. Be sure to tell him or her about any activities that cause pain, numbness, or swelling.
Exercises for De Quervain’s Tenosynovitis
People with De Quervain’s tenosynovitis are usually recommended to wear a splint for 2 to 3 weeks.
During this time, the splint can be removed to carry out the following exercises.
1) The individual places the affected hand palm down on a flat surface, such as a table. With the other hand, the affected thumb is gently moved away from the table then replaced slowly and smoothly. This movement should be repeated 5 to 10 times.
2) The person places the affected hand sideways, little finger first, on a flat surface. With the other hand, the affected thumb is moved away from the fingers, then brought back in line with them. The movement is repeated 5 to 10 times.
3) The affected hand is placed flat on the table, palm first. Keeping the hand still, the thumb is moved out to the side, as far as feels comfortable, then returned. The exercise is repeated 5 to 10 times.
4) Once exercise three has ceased to cause pain, it can be carried out with the wrist off the edge of the table.
5) With the palm down on the table, the individual should lift the thumb, as far away from the surface as possible, then bring it back down. This is repeated 10 times, increasing repetitions, as the movement becomes more comfortable.
6) An elastic band is placed around the fingers and thumb, and the thumb is moved against the resistance of the band 10 times.
7) Resting the affected hand on the table palm up, the person touches the top of the thumb to the little finger. The stretch is held for 6 seconds and done 10 times.
8) Holding the affected arm out in front, the person uses the other hand to press down the back of the hand, stretching the wrist. The position is held for 15 to 30 seconds and repeated three times.
9) As above, but the other hand is used to push the hand upwards, stretching the wrist in the other direction. The stretch is held for 15 to 30 seconds and repeated three times.
10) Holding a can in the affected hand, with the palm facing up, the individual can lower the weight then return to the starting position. Two sets of 15 are recommended.
11) The person holds a can and places the wrist in a sideways position with the thumb at the top. They then gently bend their wrist up, with the thumb reaching towards the ceiling, then gently lower to the starting position, all without moving the forearm. Two sets of 15 are advised.
12) A person can strengthen their grip by squeezing a soft rubber ball and holding the stretch for 5 seconds. Two sets of 15 are recommended.
These exercises should be used for rehabilitation and only done once the initial pain has eased.
The first step to tackling De Quervain’s Tenosynovitis is resting from the activity or activities that have caused the pain. Wearing a splint and regularly applying heat or cold packs will also help.
Diagnosis of De Quervain’s Tenosynovitis
1. Clinical examination diagnosis
- The Finkelstein test is named after Harry Finkelstein (1865-1939), an American surgeon who first described it in 1930. It is a clinical test used to assess the presence of De Quervain’s Tenosynovitis in people with wrist pain. It is performed by grasping the patient’s thumb and deviating the hand in the ulnar direction. If a sharp pain occurs along the distal radius, this is considered to make De Quervain’s Tenosynovitis likely.
- Eichhoff’s test is often wrongly named as Finkelstein’s test. Eichhoff’s test consists of grasping the thumb in the palm of the hand while the wrist is ulnar deviated, and the test is positive in the presence of pain over the radial styloid process during lunar deviation of the wrist.
- The wrist hyperflexion and abduction of the thumb (WHAT) test revealed greater sensitivity (0.99) and an improved specificity (0.29) together with a slightly better positive predictive value (0.95) and an improved negative predictive value (0.67) compared with Eichhoff’s test in one study. Moreover, the study showed that the wrist hyperflexion and abduction of the thumb test was very valuable in diagnosing dynamic instability after successful decompression of the first extensor compartment.
2. Radiological Diagnosis
2.1 Plain Radiograph – Plain radiographs are non-diagnostic of the condition but may show non-specific signs and can help exclude other causes of pain such as fracture, carpometacarpal arthritis and osteomyelitis, and the signs include soft-tissue selling over the radial styloid and focal abnormalities of the radial styloid including cortical erosion, sclerosis, or periosteal reaction.
2.2 Ultrasound – Ultrasound is very often diagnostic. Findings include:
- Edematous tendon thickening of APL and EPB at the level of the radial styloid (compare with the contralateral side)
- Increased fluid within the first extensor tendon compartment tendon sheath
- Thickening of overlying retinaculum and the synovial sheath
- Peritendinous subcutaneous edema resulting in a hypoechoic halo sign
- Peritendinous subcutaneous hyperaemia on Doppler imaging
It is important to assess for an intertendinous septum which can usually be identified if present. Ultrasound is often used to guide corticosteroid injections into the tendon compartment to treat the condition.
- Using B-mode ultrasound as standard , shear wave elastography (SWE) as diagnosis of De Quervain’s Tenosynovitis has 95% specificity and 85% sensitivity in diagnosing De Quervain’s Tenosynovitis.
- In addition, ultrasonic characteristics including the cutoff value of the extensor retinaculum for diagnosing De Quervain’s Tenosynovitis was 0.45 mm (sensitivity 96.3%, specificity 93.3%). Bony crests on the radial styloid were found in all cases of the presence of intracompartmental septum.
2.3 MRI – MRI is very sensitive and specific and useful for detecting mild disease where ultrasound may be equivocal. The presence or absence of intertendinous septum can be assessed. Findings include:
Tenosynovitis
- Increased fluid within tendon sheath (high T2, low-intermediate T1)
- Debris within sheath (intermediate T1 signal)
- Thickened edimatous retinaculum
- Peritendinous subcutaneous edema
- Peritendinous subcutaneous contrast enhancement
Tendinosis
- Tendon enlargement maximal at radial styloid and often greater at the medial aspect of the tendon
- Slightly increased intratendinous T1 and T2 signal compared to other tendons
- Striated appearance of tendons due to multiple enlarged slips
Longitudinal tendon tear
- Linear high T2 signal due to fluid within the split
- More common in APL
2.4 Ultrasound guided injections and prognosis in De Quervain’s Tenosynovitis
When comparing ultrasound and clinical characteristics of the operated and non-operated wrists, it was found that patients with high baseline visual analogue scale, with all positive clinical tests and with a persistent intracompartmental septum, had a significantly higher risk of failure following conservative treatment.
Treatment of De Quervain’s Tenosynovitis
Once the issue is diagnosed, nonsurgical treatments often succeed in resolving it.
By the treatment of the issue the inflammation of the tendons and synovial sheaths is typically reduced, so that the tendons can move freely through the synovium again.
Most cases of De Quervain’s tenosynovitis can be treated without surgery. Typically, symptoms should start to improve after 4 to 6 weeks of treatment.
Nonsurgical treatment options for De Quervain’s tenosynovitis include:
- Rest: Patients should minimize wrist and thumb movement in the affected hand. This may include pinching and gripping or any repetitive hand activities. Resting the hand on a pillow or elevated surface can also help.
- Activity modification: Avoiding the activity that may have triggered the condition, such as from a sport, hobby, or employment, will give inflammation a chance to subside.
- Splint/brace: Physicians may recommend that patients wear a splint called a thumb spica splint, which immobilizes the thumb. Patients are typically instructed to wear it 24 hours a day for 4 to 6 weeks.
- Ice: Ice therapy can reduce inflammation and numb pain signals, so it’s useful for treating De Quervain’s tenosynovitis. The affected area can be iced for 10 to 15 minutes several times a day. Ice shouldn’t be applied directly to the skin, as this can cause burns.
- NSAIDs: Pain medications that also alleviate inflammation, such as ibuprofen (Advil) and naproxen (Alieve), can help ease De Quervain’s tenosynovitis symptoms. Other non-NSAID pain medications such as aspirin may also be appropriate.
- Physical therapy: A physical or occupational therapist can assist patients by teaching them exercises for the hand and thumb and ways to complete day-to-day tasks while putting minimal strain on the inflamed tendons.
- Steroid (cortisone) injections: If the above measures fail to bring relief, physicians may recommend a cortisone injection into the tendon sheath. Most patients recover from the condition after receiving injections. One study of 80 patients with De Quervain’s tenosynovitis found that 95% were symptom-free after two or three injections over the course of 6 weeks.
However, these injections have a drawback as they carry a risk of causing reactions and side effects. In the study, 25% of the patients had temporary adverse reactions to the injections, such as a cortisone flare.
If nonsurgical treatment options fail to offer relief, there is a surgical treatment option that’s simple and effective for relieving pain and resolving the condition.
Surgical release of the tendon will reduce the pressure in your wrist. The doctor makes an incision in your wrist near the base of your thumb. Then the surgeon opens the tissue or sheaths over the swollen tendons to relieve the tendon and the compressed nerves. Loosening them up reduces the pain.
During rehabilitation, you’ll possibly feel numb or tingling near the surgical site. You’ll go through physical or occupational therapy. At the same time, you’ll have to wear a splint on your hand for a month after surgery.