Prolapsed Intervertebral Disc Disease (PIVD)
A Prolapsed Intervertebral disc disease (PIVD) is commonly called a herniated disk. A herniated disk is an injury of the spine (backbone). You have a series of bones (vertebrae) in your spine, stretching from the base of your skull to your tailbone. Between your vertebrae are round cushions called disks. The disks act as buffers between your bones, allowing you to bend and move with ease. When one of these disks tears or leaks, it’s called a herniated disk.
Every year, up to 2% of people get a herniated disk. Herniated disks are a leading cause of neck and/or arm, and back and/or leg pain (sciatica). They can happen anywhere along the spine, but herniated disks most often occur in the lower back or the neck. It’s rare for a herniated disk to be in the mid-back.
Table of Contents
Symptoms of Prolapsed Intervertebral Disc Disease (PIVD)
Most herniated disks occur in the lower back, although they can also occur in the neck. Signs and symptoms depend on where the disk is situated and whether the disk is pressing on a nerve. They usually affect one side of the body.
- Arm or leg pain: If your herniated disk is in your lower back, you’ll typically feel the most pain in your buttocks, thigh and calf. You might have pain in part of the foot, as well. If your herniated disk is in your neck, you’ll typically feel the most pain in your shoulder and arm. This pain might shoot into your arm or leg when you cough, sneeze or move into certain positions. Pain is often described as sharp or burning
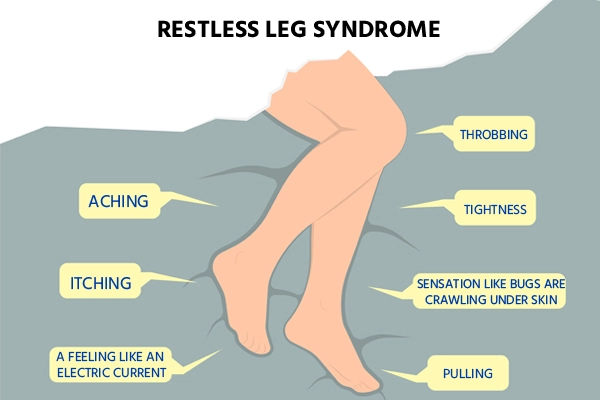
- Numbness or tingling: People who have a herniated disk often have radiating numbness or tingling in the body part served by the affected nerves
- Weakness: Muscles served by the affected nerves tend to weaken. This can cause you to stumble, or affect your ability to lift or hold items
You can have a herniated disk without symptoms. You might not know you have it unless it shows up on a spinal image.
Causes of Prolapsed Intervertebral Disc Disease (PIVD)
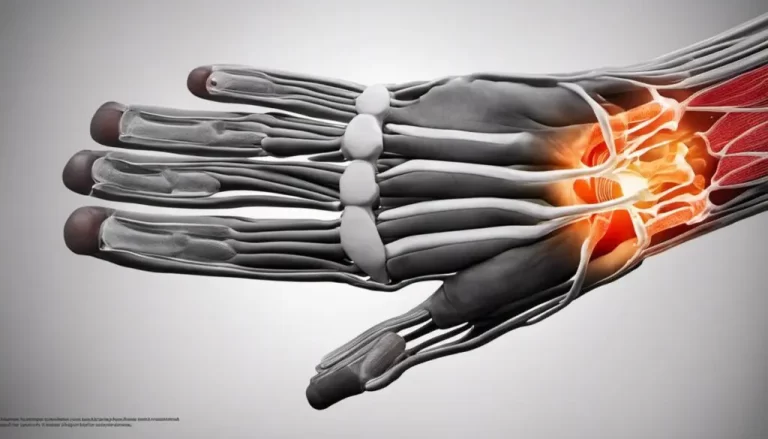
A slipped disk occurs when the soft internal section of an intervertebral disk protrudes through the outer layer.
The human backbone, or spine, consists of 26 bones called vertebrae. Between each vertebra lie rubbery, cushion-like pads called “disks.” These disks help keep the vertebrae in place and act as shock absorbers.
Spinal disks have a soft, jelly-like center and a tougher exterior.
A herniated disk occurs when some of the soft interior slips out through a crack in the wall of the disk. This most commonly occurs in the low back but can also occur in the vertebrae of the neck.
The escape of this “jelly” is thought to release chemicals that irritate nerves in the surrounding area and cause significant pain. The prolapsed disk may also put pressure on nerves and cause pain through compression.
The cause of a leaking disk is usually gradual wear and overuse as a result of repeated movement over time.
Spinal disks lose some of their water content as a person ages. This reduction in fluid makes the disks less supple and more prone to splitting.
It is not always possible to recall the exact point when a disk problem begins, but it often occurs when lifting objects without bending at the knee or after twisting while lifting a heavy item.
Risk Factors of Prolapsed Intervertebral Disc Disease (PIVD)
Herniated disks can occur at any age, but they are most common for men between the ages of 20 and 50 years.
Factors that increase the likelihood include:
- Weight: Being overweight puts additional stress on the lower back
- Genetics: A person might inherit a predisposition to herniated disks
- Occupation: Individuals with physically demanding jobs or pastimes that involve pushing, pulling, or twisting are prone to herniated disks. Any repetitive activities that strain the spine can cause them
- Unsafe lifting technique: People should always apply force from the legs, not the back, when lifting heavy items. Incorrect technique can lead to a herniated disk
- Driving often: A combination of being seated for long periods and the vibrations and movements of the car can damage the disks and spinal structure
- Sedentary lifestyle: A lack of exercise can lead to a herniated disk
- Smoking: This might reduce oxygen supply to the disks and lead to a grinding-down of the tissue
Preventions of Prolapsed Intervertebral Disc Disease (PIVD)
It’s not always possible to prevent a herniated disk. But you can reduce your risk by:
- Using proper lifting techniques: Don’t bend at the waist. Bend your knees while keeping your back straight. Use your strong leg muscles to help support the load
- Maintaining a healthy weight: Excess weight puts pressure on the lower back
- Practicing good posture: Learn how to improve your posture when you walk, sit, stand and sleep. Good posture reduces strain on your spine
- Stretching: It’s especially important to take stretching breaks if you often sit for long periods
- Avoiding wearing high-heeled shoes: This type of shoe throws your spine out of alignment
- Exercising regularly: Focus on workouts that strengthen your back and abdomen muscles to support your spine
- Stopping smoking: Smoking can weaken disks, making them vulnerable to rupture. Consider quitting smoking
Diagnosis of Prolapsed Intervertebral Disc Disease (PIVD)
Diagnosis of prolapsed intervertebral disc disease is done for both Cervical and Lumbar Spine, by checking the history and physical examination.
Cervical Spine
History – In the cervical spine, the C6-7 is the most common herniation disc that causes symptoms, mostly radiculopathy. History in these patients should include the chief complaint, the onset of symptoms, where the pain starts and radiates. History should include if there are any past treatments.
Physical Examination – On physical examination, particular attention should be given to weaknesses and sensory disturbances, and their myotome and dermatome distribution.
Typical findings of solitary nerve lesion due to compression by herniated disc in cervical spine
- C5 Nerve: neck, shoulder, and scapula pain, lateral arm numbness, and weakness during shoulder abduction, external rotation, elbow flexion, and forearm supination. The reflexes affected are the biceps and brachioradialis
- C6 Nerve: neck, shoulder, scapula, and lateral arm, forearm, and hand pain, along with lateral forearm, thumb, and index finger numbness. Weakness during shoulder abduction, external rotation, elbow flexion, and forearm supination and pronation is common. The reflexes affected are the biceps and brachioradialis
- C7 Nerve: neck, shoulder, middle finger pain are common, along with the index, middle finger, and palm numbness. Weakness on the elbow and wrist are common, along with weakness during radial extension, forearm pronation, and wrist flexion may occur. The reflex affected is the triceps
- C8 Nerve: neck, shoulder, and medial forearm pain, with numbness on the medial forearm and medial hand. Weakness is common during finger extension, wrist (ulnar) extension, distal finger flexion, extension, abduction, and adduction, along with during distal thumb flexion. No reflexes are affected
- T1 Nerve: pain is common in the neck, medial arm, and forearm, whereas numbness is common on the anterior arm and medial forearm. Weakness can occur during thumb abduction, distal thumb flexion, and finger abduction and adduction. No reflexes are affected
Lumbar Spine
History – In the lumbar spine, herniated discs can present with symptoms including sensory and motor abnormalities limited to specific myotome. History in these patients should include chief complaints, the onset of symptoms, where the pain starts and radiates. History should include if there are any past treatments.
Physical Examination – A careful neurological examination can help in localizing the level of the compression. The sensory loss, weakness, pain location and reflex loss associated with the different levels are described below.
Typical findings of solitary nerve lesion due to compression by herniated disc in lumbar spine
- L1 Nerve: pain and sensory loss are common in the inguinal region. Hip flexion weakness is rare, and no stretch reflex is affected
- L2-L3-L4 Nerves: back pain radiating into the anterior thigh and medial lower leg; sensory loss to the anterior thigh and sometimes medial lower leg; hip flexion and adduction weakness, knee extension weakness; decreased patellar reflex
- L5 Nerve: back, radiating into buttock, lateral thigh, lateral calf and dorsum foot, great toe; sensory loss on the lateral calf, dorsum of the foot, web space between first and second toe; weakness on hip abduction, knee flexion, foot dorsiflexion, toe extension and flexion, foot inversion and eversion; decreased semitendinosus/semimembranosus reflex
- S1 Nerve: back, radiating into buttock, lateral or posterior thigh, posterior calf, lateral or plantar foot; sensory loss on posterior calf, lateral or plantar aspect of foot; weakness on hip extension, knee flexion, plantar flexion of the foot; Achilles tendon; Medial buttock, perineal, and perianal region; weakness may be minimal, with urinary and fecal incontinence as well as sexual dysfunction
- S2-S4 Nerves: sacral or buttock pain radiating into the posterior aspect of the leg or the perineum; sensory deficit on the medial buttock, perineal, and perianal region; absent bulbocavernosus, anal wink reflex
Treatment of Prolapsed Intervertebral Disc Disease (PIVD)
You may need more advanced treatments if your symptoms aren’t getting better. Your healthcare provider might recommend:
- Medication: Your provider may prescribe an anti-inflammatory pain reliever or muscle relaxant
- Physical therapy: A physical therapist teaches you an exercise program to help relieve pressure on your nerves. Exercise loosens tight muscles and improves circulation
- Spinal injections: Called an epidural or nerve block, a spinal injection is a shot of steroid medication directly into your spine. The medication reduces swelling and inflammation of the nerve from the disk herniation. This will allow your body to heal and return to activity faster
- Surgery: In rare cases, a large herniated disk might injure nerves to the bladder or bowel. That may require emergency surgery. For nonemergency cases, surgery is an option when other treatments fail. There are various ways to perform spinal decompression surgery, but the goal is to relieve pressure on the nerve
Herniated disks get better on their own over time or with nonsurgical treatment for 9 out of 10 people. If other treatments don’t relieve your symptoms, your healthcare provider may recommend surgery. There are multiple surgical techniques for relieving pressure on the spinal cord and nerves, including:
- Diskectomy to remove your herniated disk
- Laminectomy to remove part of the bone around a herniated disk and expand your spinal canal
- Artificial disk surgery to replace a damaged herniated disk with an artificial one
- Spinal fusion to directly join two or more vertebrae together to make your spine more stable
Exercises for Prolapsed Intervertebral Disc Disease (PIVD)
It can be frustrating to know which exercises work well, and which do not, for the varied symptoms of a lumbar herniated disc. These symptoms can include numbness and tingling in the legs, decreased strength, diminished sensations, and generalized back pain.
Here are 3 exercises to avoid, and some safe substitutes:
1. Avoid “Good mornings”
Nothing could be further from a good morning with this weight-lifting exercise. Even if the good morning is performed by someone without a disc herniation, it could lead to problems.
In a good morning, weight is placed on the shoulders, similar to when performing a traditional squat. The next step is to bend forward at the hips and allow your chest to drop toward the floor while maintaining a straight spine and legs. The exercise is a problem because it places a large working load on the lower back and buttocks.
Instead, try a “waiter’s bow”
A better alternative would be a “waiter’s bow.” It involves bending forward from your hips, gently placing your hands on a bed, and allowing your body to rock back slightly. Always maintain the natural curve in your lower back while doing this stretch—never let your lower back flatten or arch upward.
When returning to standing, squeeze your buttocks and drive your hips forward, rather than arching your back and lifting your torso.
This can be a valuable exercise to re-learn how to use the buttock muscles, rather than the low back, in order to stand. This version of a waiter’s bow exercise is also gentle as it supports your torso through placing your hands on the bed.
If you want to increase the difficulty, place an elastic band around your hips and anchor the opposite end on something (such as a door knob) behind you so your hips must work against resistance when driving them forward and standing up.
2. Avoid a standing hamstring stretch
Yes, it is important to stretch your hamstrings daily, but the common approach of “stand and reach for your toes” could cause serious issues when dealing with a herniation. The problem is that the stretch allows the back to compensate and bend forward, placing unnecessary stress on the front half of the disc.
Instead, stretch your hamstrings lying down
Instead, lie down on the floor near a doorway, straightening—as much as you can—the leg so you will not be stretching through the opening. Next, place the leg you will stretch leaning up along the doorframe. The closer you get to the wall, the more intense the stretch. A common issue with stretching is that people go too aggressively. Make the stretch mild, or you’ll waste your time.
Remember to stretch both legs, but only one at a time.
3. Avoid deadlifts
If you’re a CrossFitter, you probably just screamed and slammed the laptop closed in frustration, but hear me out. One of the most common movement problems is allowing your lower back to round out while bending forward or lifting an object. A deadlift requires perfect mechanics. Even when done well, it will cause a great amount of compression at the disc.
Instead, make a bridge
A substitute for a deadlift could be a bridge, where the core (abdominals and hips) are active. While lying on your back, knees bent up and feet flat on the floor, contract your abdominals and buttocks. Next, you raise your back and buttocks off the table in one solid unit, rather than rolling up vertebrae by vertebrae, by pushing through your feet. A variety of modifications can be made to increase the difficulty, such as marching, performing the bridge with one leg, and lifting your hands into the air.
Sometimes low back pain could be coming from other parts of the body, and sending the symptoms to the area of the lower back. Before trying any exercises or stretches it is always best to have thorough medical evaluation, rather than try to self-diagnose and treat.
The majority of treatment and rehabilitation recommendations will include some sort of exercises program; if you have a clinical diagnosis of a lumbar disc herniation, then knowing which versions of exercises to avoid and which are more effective are an important part of helping you better reduce and manage your symptoms.