Dystonic Cerebral Palsy and Physiotherapy Treatment:
Table of Contents
Introduction:-
Dystonic cerebral palsy, also termed to as dystonia, causes involuntary muscle contractions which results in to involuntary movements that affect either one part of the body or the whole body.
Dystonic CP is a kind of dyskinetic cerebral palsy. There is no permanent cure for it, but several treatment options are available, including sensory tricks that can be used to control the symptoms.
Dystonia:
Dystonia term refers to spasm in muscle tone which is characterized by involuntary muscle contractions that leads to slow twisting or repetitive movements, or abnormal sustained postures, that is triggered by attempts to movement.
Characteristics of dystonia include:
Repetitive and sustained (prolonged) movements
Abnormal postures
Movements that are rapid (fast) or slow and are often painful due to muscle stretch
Involuntary movements triggered while attempts at controlled movement
Involuntary movements occur more often when the person is tired, anxious, tense or in emotional state Pain can also result in an increase in these movements
What is Dystonic Cerebral Palsy?
According to the American Association of Cerebral Palsy and Developmental Medicine, dystonic cerebral palsy is a movement that causes increased muscle tone and motion is uncontrollable, involuntary posture and movement.
Dystonic cerebral palsy often disturbs with the child’s sleep due to uncomfortable pain caused by contractions. It can also be difficult for children with dystonia to sit or lie down for too long.Moreover, the involuntary movement contributes to the child expending a lot of energy,which can tire them easily and feel lethargic. Some children with dystonic cerebral faces problems while chewing and swallowing, which could lead to malnutrition.
Signs and symptoms:
Along with uncontrollable and repetitive movements, patients with dystonic cerebral palsy could also witnesses the following:
- Movement that differs between rapid and slow
- Pain while moving any limb
- Triggering in uncontrollable movements if the child is tired or anxious
- Affected speech patterns due to unruly movements in the jaw and mouth
- Drooling ( salivation by itself)
- challenges with walking
- One leg drags or drop foot
- Foot cramps and clonus
- Disorderly blinking
- Speaking and eating issues
- For young children with this type of cerebral palsy, symptoms generally first appear in a hand or foot. Over period, the symptoms can expand to other limbs of the body. By the time the patient reaches the teen years, the further progression of the symptoms tends to slow down.
Hallmark signs of Dystonia:
The movement pattern demonstrated by the children vary with change in position, for instance a child may have a scissoring posture in lower legs in standing and a splayed posture with legs turned outwards in sitting. This is characteristic of dystonia and differentiates it from hypertonia.
Dystonia is an unintentional and rapid movement and cannot be cognitively controlled
It is fluctuating in nature and presents with elevation or declination in tone influenced by trigger factors like beginning of a movement, making effort, emotions elicited during the task, external touch or general health conditions.
The muscles typically become stiff and spastic with purposeful movements of a distal body part
The postures are twisting in nature and can affect one or multiple body segments or the entire body.It comes with an All or nothing Phenomena where either the child is contracting every muscle in the body segment or switching off completely with a collapse in end in movement.
Types:
Dystonic cerebral palsy can be subdivided by the parts of the body it affects which are illustrated below:
Focal Dystonia :-Many child patients experience dystonia on one side of the body. This is known as focal dystonia, which can affect both lower limbs and one upper limb or the trunk of the body, along with one lower and one upper extremity.
Generalized Dystonia :-Other children have problems with their entire body, known as generalized dystonia. Patients with generalized dystonia usually have a difficulty with walking and balancing activity. Generalized dystonia can also occur in the upper limb and upper body, making movements tight and painful also causing fatigue.
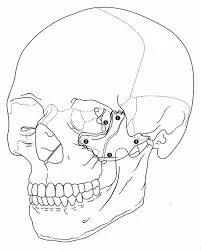
Cervical Dystonia:- Dystonia can also affect the head, neck, and shoulders, making for abnormal twists and turns while movement of neck, This is known as cervical dystonia.
Oro-mandibular Dystonia:- It occurs when the child’s mouth, jaw, and tongue are affected. Some children are prone to malnutrition and dietary issues because the patient does not take dietary supplements properly.
Hemi-dystonia:- It affects one upper limb and lower limb on the same side of the body.Symptoms of dystonic cerebral palsy may be present sometimes, but not while all activities. For example, a child may have problems while walking but not when swimming or other activity.It is notable that not all children exhibit the same symptoms.
Dystonic Cerebral Palsy and Sensory Tricks:
According to Current Clinical Neurology, a sensory trick movement occurs when a child touches a particular part of their body, such as their chin, which can neutralize involuntary head movements and stop muscular contractions.
Further, placing a finger near the dystonic part and raising a hand may release the dystonia affection. Others movements can be elicited find help by touching an eyelid.
According to the U.S. National Institutes of Health science, the sensory tricks are trial and error, and while one trick may work for one child, it may not work for another one, thus these tricks should be examined rather than copying.Sensory tricks vary from patient-to-patient and within the same individual.
Assessment:
Dystonia is a continuously overlooked element of the neurological presentation of CP. Therefore, it is recommended that a ‘dystonia’ assessment be routinely included in every neurological examination ,assessing for differing hypertonia, and using some tactile stimulation or voluntary movement to trigger dystonia. More information can be found in Section (can use a standardized scale such as the Barry Al bright Dystonia Scale. Assess the impact of the dystonia on functional ability, pain/comfort (including sleep), and care-giving and whether management is required.
If dystonia is present, assess whether the neurologic presentation is consistent with CP (risk factors, brain imaging, and associated family history) or if additional work is required. An important masquerader of CP related dystonia is Dopamine Responsive Dystonia. Consider the need for a experiment of levodopa and a referral to a neurologist or geneticist for additional diagnostic work.
Investigation:
Brain-imaging technologies can rule out areas of injured or abnormal development in the brain. These tests might include the following:
MRI;-
An MRI uses radio waves and a magnetic field to produce detailed 3D or cross-sectional images of the brain. An MRI can usually identify lesions or abnormalities in patient’s brain. This test is painless, but it’s too sound making and can take up to an hour to complete or more. Child will likely receive a sedative or light general anesthesia before the test.
Cranial ultrasound:
This can be performed during infancy. A cranial ultrasound uses high-frequency sound waves to produce images of the brain. An ultrasound does not produce a detailed image, but it may be used because it’s quick and it can provide a valuable preliminary assessment image of the brain.
Electroencephalogram (EEG):
If the child is suspected of having seizures or convulsions, an EEG can evaluate the condition further. Seizures can develop in a children with epilepsy. In an EEG test, a series of electrodes are attached to your patient’s scalp. The EEG records the electrical activity of patient’s brain. It’s common for there to be changes in normal brain wave patterns during or after epilepsy.
Laboratory tests:
Tests of the blood, urine or skin might be used to screen for genetic or metabolic problems.
Causes and risk factors of Dystonic cerebral palsy:
The National Institute of Neurogenic Disorders and Stroke reports that sometimes dystonia causes are idiopathic( unknown cause ). In other some cases, dystonia is a genetic condition.
Low birth weight, Damage to the placenta, and premature birth are associated with dystonia. Also, physical and psychological trauma during birth can result in dystonia. This occurs when a baby is deprived of oxygen ( hypoxia ) during childbirth or when a mother applies excessive force during delivery.
For example, a newborn with jaundice can typically have excess bilirubin in their blood. Untreated jaundice that is high can result in to basal ganglia damage in the brain, known as kernicterus. In kernicterus, the basal ganglia are stained ( marked ) with bilirubin. This type of brain damage can result in Dystonic cerebral palsy.For patient with dystonic cerebral palsy, damage usually occurs in the brain’s upper motor neurons.
As said earlier, the main cause of dystonic cerebral palsy is damages to parts of the basal ganglia, particularly the area of the brain that has control over movement. The basal ganglia are a group of sub cortical nuclei in the brain that control motor function, learning,perception and behavior.
Because cerebral palsy is caused by damage to the developing brain and therefore affects individuals early in life, poorly managed dystonia can significantly affect growth in adulthood, posture, overall mobility and daily life activity.
Other risks associated with poorly managed dystonic CP are:
- poor sleep quality
- high energy expenditure and fatigue, tiredness
- malnutrition
- chronic pain due to movement
- As within all types of cerebral palsy, the brain damage that caused dystonic CP is non- progressive, thus it can be revealed. Anyhow, symptoms can worsen if not properly managed.
Treatment for Dystonic cerebral palsy:
Medication:
The use of medications for dystonic cerebral palsy can vary depending on the severity of sensory and motor impairments.
Orly baclofen and some anticholinergic drugs like trihexyphenidyl are often used to manage dystonic cerebral palsy which reduces ACH production. However, because oral forms of these medications cannot effectively pass through the blood-brain barrier thus, individuals often need higher doses, that can increase child’s risk of side effects.
Another medication that may be recommended is baclofen intrathically. Intrathecal baclofen therapy is basically surgical implantation of a baclofen pump that injects the drug directly to the cerebrospinal fluid in brain. It allows for a lower dose of muscle relaxant to enter the body and be effective by breaking blood-brain barrier, decreasing the risk of side effects.
This review found that many studies of intrathecal baclofen injection treatments have reported significant effective in dystonia and subjective improvements in mobility, speech and communication, chewing, swallowing, head control, sleep, pain and mood, comfort, and ease of care.”
Physiotherapy Treatment for Dystonic cerebral palsy:
It is imperative to note that much of this Dystonia Care Pathway is based on expert opinion, as the effective treatment for dystonia management in CP is currently limited.
Rehabilitation Strategies:
Rehabilitation strategies used by physiotherapist, occupational therapies and speech pathologists are usually considered cornerstones in dealing with dystonia in CP.General principles include:
1) ensuring therapy is goal-oriented,
2) avoiding asymmetry and aiming for symmetrical positioning to build motor control
3) optimizing seating and positioning with good stability and support
4) considering orthoses and splints to increase stability and coordination
5) considering the need for communication and psychological supports.

Generalized Dystonia Management:
With increasing severity of dystonic cp, additional interventions may be required beginning with oral medications. Oral baclofen is considered a first line medication for the management of any type CP. Common indications for this drug include pain or difficulty sleeping associated with dystonia in CP.
If the child does not respond well to oral baclofen, trihexyphenidyl can be used as a second line medication. Other oral medications should be considered for some specific indications. For example, the intermittent use of benzodiazepines is helpful for dystonic storms or disturbed sleep, and gabapentin for dystonia associated with pain. Clonidine can also be considered for the disturbed sleep associated with dystonia. The majority of the doctors group did not find levodopa effective in reducing dystonia in CP. Given this experience paired with the lack of evidence, it was not formally placed in the treatment arm of the treatment pathway.
In the presence of severe generalized dystonia including with significant impact on care and comfort, more aggressive management should be undertaken. This may include intrathecal baclofen (I TB) or sometimes deep brain stimulation (DBS). These strategies requires a specialist team.
Children with severe generalized hypertonia with a both dystonia and spasticity may trial intrathecal baclofen. Other considerations of whether to choose ITB or DBS can be based on the cerebral anatomy and whether placement of the simulator in the globes pallidus is possible. ITB should be used with precaution in the presence of nocturnal respiratory compromise. In the presence of dystonia with pain, other generic pain management strategies can be undertaken.
A main feature of dystonia in CP is a fluctuation in the severity of the dystonia. For this reason it is important to periodically re-examine the individual and adjust the interventions as required.
For some individuals with severe dystonia, a personalized plan for managing increasing dystonia can be developed and includes increasing the dosage of on going oral medications or introducing a second medication (e.g. clonidine or gabapentin). The use of the Dystonia Severity Action (DSAP) may be helpful for monitoring unstable dystonia . A rapid and severe increase in dystonia is termed ‘Periodic Status Dystonicus’.
It can be life-threatening and requires urgent treatment often with a combination of benzodiazepines and clonidine (enteral, intravenous, or trans-dermal). Another important issue is the triggering of dystonia from secondary health conditions including gastrointestinal disorders such as reflex or constipation. This can help minimize the symptoms and can derive to better therapy.The overall general health of the individual should be carefully monitored and secondary health issues should be actively addressed.
Focal Dystonia Management: For individuals with focal or sentimental dystonia associated with persisting posture attempts causing pain or impacting on function and care-giving, periodic injections of Botulinum toxin can be undertaken. Consider targeting both the agonist and antagonist muscles around the joints involved with the dystonic posture.
Physiotherapy exercises:-
The dynamic muscular control approach based on changing movement patterns and configuration of the task rather than the hierarchical planning of the neurological motor development is used for the rehabilitation.
This approach allows observing the child from the functional range aspect in environments such as the home and preschool and assessing a realistic evaluation. The aim of Dystonic CP rehabilitation should be the progression of existing abilities of the child and to keep these abilities at an extreme level.
It is imperative to minimize the negative effects of functional limitations and disorders of child, and protect the child from the disability to prevent secondary disorders and maximize the motor functions to the extent permitted by the current deficit. Thus, this type of treatment where all the functions can be gained should be determined first.
The major goal of treatment has to be reaching maximum functional and bodily capacity. However, correction of abnormal posture and muscular patterns, prevention of the deformities that may develop in future, mobilization for good range, development of existing skills, and eliciting new skills are also among the targets of treatment.
The rehabilitation protocol of children with CP is decided according to the biological age and functional abilities of the child , somehow; the general treatment approach shows significant changes according to the age. Combining of different approaches should be used in distinguish age group.The environment where the therapy can be conducted can either be the home of the child or clinics and hospital departments, inpatient rehabilitation hospitals, rehabilitation centers or school-based therapeutic places.
The therapy protocol should be consistent with the patient’s age and skills as well and have a specific purpose for each limitation. Moreover, relevant measurable short-term targets should be made so that patient can achieve easily. These short-term goals allow the therapist, family and the child to be informed about therapy and throughout process.
Another main part of the treatment is family training. The exercise plan should be taught to the patient and family, the functional skills of the child in the home environment should be assessed, and the long-term expectations of the family should be taken into account and assure them about progression.
It is most important that the rehabilitation practice should be started as early as possible due to the plasticity characteristics ( ability to adapt changes) of the central nervous system.
The present function of the patient and prognosis for acquiring new skills should be taken into account when determining on the effectiveness of the physiotherapy. While the treatment protocol is made, the growth spurts of the patient and procedures such as surgery should be taken into account if necessary. Whatever the optimal functional level of the child, the family should also be indulged in the treatment through home programs.
Deciding on the vigorous of the treatment is important in the management of certain limitations. The usage of intensified therapy after orthopedic interventions and neurosurgery, during growth spurts that can make impact on the motion bio mechanics of the child, and when a specific aim is being focused on has critical importance. Physiotherapy in adolescents and adults with dystonic CP should be supported with recreational activities. Therefore, motivation can be provided for the acquisition of new skills.
Neuro-developmental therapy:
At present, the Bobath approach, initially, aims to observe the existing performance of the of in-dependency within the limitations of the patient’s potential assessment and result. Nero-developmental therapy (NDT) was developed by Bertha Bobath,who was physiotherapist, Karel
Bobath, who practiced as neuro-psychiatrist. This approach was given shape in order to involve scientific theories that were and empirical experiments which were developed and has a specific structure that is available to development and dynamic.
Thus, treatment has been developed until its first application and has undergone some particular changes. According to the Bobath’s, the motor control problem is one of the most imperative problems and delay or disorder of normal motor development or not being able to establish postural control and stability against gravity due to function problems in the central nervous system is the major significant factor that causes motor control problems.
The NDT method, which focuses all problems occurring in the patient as a result of the injury in the central nervous system has focused on working on short term and long term memory, ability for perception, sense, postural control and abnormal muscular patterns, reflexes and sensory motor components in the muscle tones.
It is also used to facilitate special gripping movement techniques, balancing activity and normalize muscle tone and also to decrease abnormal movement patterns, reflexes and spasticity. During the period when the NDT was first developed, the patient was more approached with passive movements; however, as it has received the name of “living concept” it is observed that the child is more active now with NDT.
The effect on the family is very important and the family must become like a part of the rehabilitation team within the scope of NDT. There have been debates on whether NDT principles affect motor development in terms of reflex and hierarchic model of motor control is focused on only neural explanation.
For instance, in the motor control model, the central nervous system is regarded as one of the systems that affect only motor control behavior. Motor control is also affected by cognitive and environmental sensitive factors. However, major physiological components and environmental contents are accepted as non-neural explanations in the individual’s progress .
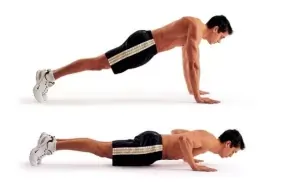
Principles
1 Mobilization of muscle and stiff joint
2 Muscular stretch
3 major practice of more normal movements
4 Less effortful functional tasks
5 Encouraging weight bearing
6 Integration of postural control and task performance
7 To focus sensory input and motor control
Strength training:
Disorders affecting muscular strength and motor control in children with dystonic CP are indicated among the main causes of the motor disorder . Muscle weakness and fatigue is a common disorder in children with CP and is associated with inefficient or reduced motor unit charge, inadequate co-activation of antagonist or agonist muscles, secondary type of myopathy and impaired muscle physiology.
Studies have shown the usefulness of strength training in children with CP and revealed the relationship of muscular strength with activity . Strength exercises increase muscle strength, flexibility, posture and balance in CP. They also increase the level of activity in daily life and develop functional activities such as walking, running and cycling.
Isotonic, isometric and isokinetic exercises should be used to increase muscle strength and motor function recovery. Strengthening methods commonly used in all age groups are functional and daily living activities, gravity and body weight . A efficient level of loading is necessary to increase the strength of the muscles when choosing among distinguish strengthening methods.
Strength training mainly requires effort against progressive resistance. Progressive resistance exercises that initiate development of muscle performance and motor skills by increasing the force production capacity are important for patients with dystonic CP.
Increase in muscle strength and joint range of motion are gained with resistance exercise training.Many researcher concluded that resistance exercises that involve the lower and upper limbs in children with dystonic diplegia increase the strength capacity. An increase in the spasticity was not present with resistance exercise training . Strength Training organized with manual resistance, fitness devices, free weights, Gym ball, thera-band, running band, static bike, leg press and isokinetic equipment are classic examples of resistance exercises.
Presence of weakness comparing to their peers in the affected extremities of children with dystonic CP even if they have a high functional level, and this weakness increases with neurological involvement . Moreover, patient with CP show lower strength-generating capacity in all lower extremity muscle groups, except for the hip extensors, compared to their healthy peers.
When the gross motor function classification system levels are taken into consideration, the muscle strengthening trainings are most commonly used in levels I-III.Patients at this level have good selective control and less co-activation of muscle spindle and are therefore considered to tolerate the specific progressive exercise training better. Muscle strengthening in children on level IV and V is difficult due to the problems with motor control. Hydrotherapy is the most popular muscle-strengthening method in patients at initial level.
Functional strength training, increase the endurance of the weak antagonist and responsible spastic agonist and to give functional benefits in patient with CP. Usually Functional exercises are a combination of aerobic and anaerobic capacity and strength training; which develop the physical fitness, intensity of activity and quality of life in ambulatory children.
Also treadmill can provide functional exercise and is a dynamic approach that should be used to stimulate the motor development of individuals with CP. The normal gait cycle and distance of individuals with CP elicits with treadmill exercises. Treadmills that support the body weight can be an option in individuals with CP who have no weight bearing ability.
Strength gaining is effective only when the goal is the development of a targeted motor skill or function. The functional gains of children without one’s voluntary muscle control capacity from a strength training protocol are thus restricted and not allowed to practice. Surgical interventions such as muscle-tendon lengthening, selective dorsal rhizotomy (SDR), botulinum toxin injection, and intrathecal baclofen pump implantation can increase the muscle length and improve muscle control in these children.
Therefore, strength training can be more effective and permanent effects can be ensured.Training the same muscle groups on alternative days is appropriate in children. Strength training can be modified in the presence of muscle pain or when muscle pain and tension develops with continuous exercise. The child should be trained to able to comprehend and consistently produce maximum and almost maximum effort for strength training.
Although strength training can be implemented for children aged 3 years or older no less than 3, it is therefore more appropriate for children aged 4-5 years . Despite the lack of an evidence regarding the harm of strength training, it should not be neglected that excessive physical effort may trigger seizures in children with a relevant past history.