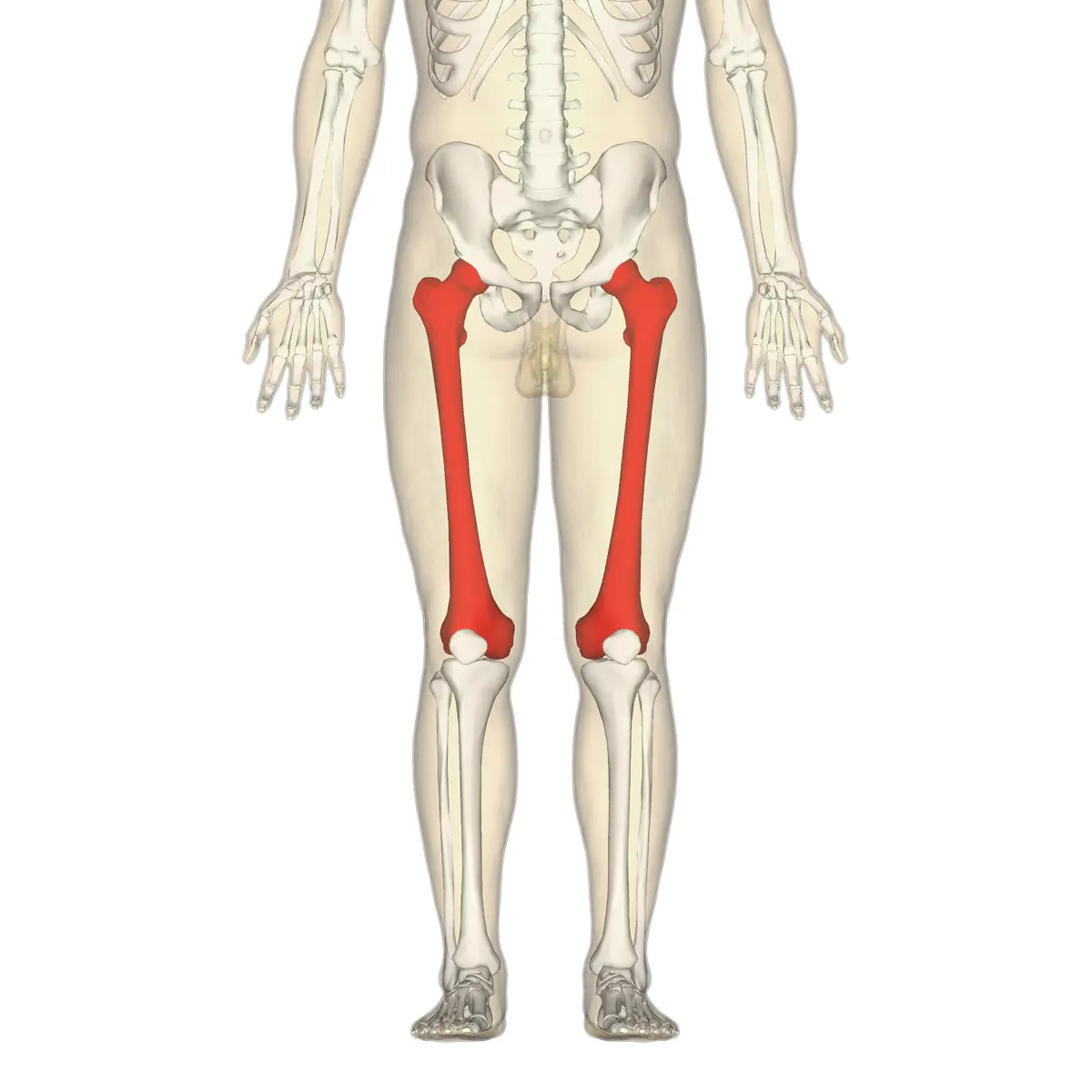
Femur Bone
Table of Contents
Introduction
introduction of the femur bone is as described follows ,
The longest and strongest bone in the human body is the femur, also referred to as the thigh bone. It plays a crucial role in providing structural support and bearing the majority of the body’s weight during activities such as standing, walking, and running.
Located in the thigh region, the femur connects the hip bone (pelvis) to the knee joint. Its distinctive structure includes a shaft and two rounded ends, known as the head and the condyles, which articulate with other bones to facilitate smooth movement.
The femur also houses the bone marrow, contributing to the production of blood cells. Due to its vital functions, the femur is essential for maintaining the body’s stability and enabling various forms of physical activity.
- In a normal adult, the inclination angle of the femur—also called the angle between the neck and shaft—measures approximately 128 degrees. But as people age, the inclination angle gets less. Other significant characteristics of the femur are the linea aspera and the adductor tubercle, which serve as the attachment points for the posterior part of the adductor magnus.
- The acetabulum of the pelvis encloses the femoral head, forming the ball-in-socket joint that is the hip. The head of the femur is oriented somewhat anteriorly, superiorly, and medially. The fovea capitals femoris, a pit on the head, is connected to the acetabulum via the ligamentous teres.
- The anterior arch of the shaft of the femur is moderate. The shaft of the medial and lateral condyles spreads out in a cone shape at the distal femur, landing on a cuboidal base. The knee joint is formed by the femur and tibia joining at the medial and lateral condyles.
- The synovial joints of the hip and knee are covered in cartilage to minimize friction and maximize range of motion. The bony characteristics provide reference points when determining the axis along the bone known as the femur.
- The average adult femur is about eighteen inches long. The strongest bone in your body is also the femur. It is capable of bearing up to thirty times your body weight.
Structure and function of the femur bone
Structure and function of the femur bone is as described follows
- The femur’s primary roles include stability of gait and weight bearing. The thick sheath known as the capsular ligament encircles the proximal femur and acetabulum periosteum. The femoral head is held in place within the pelvic acetabulum by this ligament. External rotation is permitted but internal rotation is restricted by the capsular ligament.
- The proximal tibia and distal femur form the hinge joint that makes up the knee. The tibia femoral articulation is stabilized and cushioned by the medial and lateral meniscus. Valgus and varus deformities are prevented by the medial and lateral ligaments. The anterior and posterior cruciate ligaments in the knee joint limit the tibia’s anterior or posterior displacement while permitting some rotational mobility of the knee. When extending the knee, the patellofemoral joint is utilized.
The proximal region of the femur bone
The proximal region of the femur bone of the femur bone is as described follows ,
- The hip joint is formed by the proximal portion of the femur articulating with the pelvic acetabulum.
- It is made up of the larger and lesser trochanters, two bony processes, and a head and neck. The intertrochanteric line anteriorly and the trochanteric crest posteriorly are the two bony ridges that link the two trochanters.
- The head and pelvic acetabulum articulate to produce the hip joint. Its smooth surface is coated in articular cartilage, except the fovea, a tiny indentation where the ligamentous teres are attached.
- The neck of the femur bone joins the femur’s head and shaft. It is cylinder-shaped and protrudes medially and superiorly. It is positioned concerning the shaft at a about 135-degree angle. There is more range of motion at the hip joint at this angle of projection.
- The most lateral palpable bone projection that arises from the anterior portion, directly lateral to the neck, is called the greater trochanter.
- Numerous muscles in the gluteal area, including the gluteus medius, gluteus minimus, and piriformis, attach to it. This is the site of origin of the vastus lateralis.
- A strong contraction of the gluteus medius may result in an avulsion fracture of the greater trochanter.
- Smaller than the greater trochanter is the lesser trochanter. It protrudes from the femur’s posteromedial side, immediately below the neck-shaft junction.
- It is where the iliopsoas attaches, and a hard contraction of it can result in an avulsion fracture of the lesser trochanter. The intertrochanteric line is a ridge of bone that connects the two trochanters on the anterior aspect of the femur and runs infer medially. It is referred to as the pectineal line once it crosses the lesser trochanter on the posterior surface.
- The strongest ligament in the hip joint, the iliofemoral ligament, attaches to it. It also functions as the hip joint capsule’s anterior connection. Similar to the intertrochanteric line, the intertrochanteric crest is a bone ridge that joins the two trochanters. It is situated on the femur’s posterior surface. The tubercle, which is spherical and on its superior half, is where the quadratus femoris attaches.
Shaft of the femur bone
The shaft of the femur bone of the femur bone is as described follows ,
- The femur shaft descends somewhat to the medial side. This increases stability by bringing the knees closer to the center of gravity of the body. The midsection of the shaft has a circular cross-section, but the proximal and distal portions are posteriorly flattened.
- The term “linea aspera” refers to the roughened bone ridges on the posterior surface of the femoral shaft (rough line in Latin). The medial and lateral supracondylar lines are formed by the distal splitting of this. It is between them that the popliteal surface is flat.
- The pectineal line is formed proximally by the medial boundary of the linea aspera. The gluteal tuberosity, where the gluteus maximus is attached, develops from the lateral border. The medial and lateral popliteal fossa floors are formed by the distal widening of the linea aspera.
The distal end of the femur
The distal end of the femur bone of the femur bone is as described follows ,
- The medial and lateral condyles, which articulate with the tibia and patella to form the knee joint, are characteristics of the distal end of the femur.
- The rounded regions near the end of the femur are called medial and lateral condyles. While the front surface articulates with the patella, the posterior and inferior surfaces articulate with the tibia and menisci of the knee. A more pronounced lateral condyle aids in impeding the patella’s natural lateral mobility, whereas a flatter condyle increases the risk of patellar dislocation. Bony elevations on the non-articular portions of the condyles are known as medial and lateral epicondyles. The bigger epicondyle is the medial one.
- The origin of the knee’s medial and lateral collateral ligaments is found in their respective epicondyles.
- The deep intercondylar fossa is a deep groove between the two condyles on the femur’s rear surface. The anterior cruciate ligament (ACL) attaches to the medial aspect of the lateral condyle, and the posterior cruciate ligament (PCL) attaches to the lateral aspect of the medial condyle. It has two facets where intracapsular knee ligaments can be attached.
Articulation of the femur bone
Articulation of the femur bone is as described follows ,
- With the acetabulum acting as the socket and the femoral head acting as the ball, the proximal femur articulates with the acetabulum of the pelvis. enables three planes of movement at the hip: internal and external rotation in the horizontal plane, flexion and extension in the sagittal plane, and abduction and adduction in the frontal plane.
- The tibiofemoral joint is the result of the convex femoral condyles of the femur articulating with the condyles of the tibia distally. There are two planes of movement at the tibiofemoral joint: the horizontal plane’s internal and external rotation and the sagittal plane’s knee flexion and extension.
- The articulation of the patella with the femur’s intercondylar/trochlear groove forms the patellofemoral joint.
Embryology
Embryology of the femur bone is as described follows ,
- The cells of the lateral plate mesoderm are the first to develop into limb buds in the femur and lower limb. In the fourth week, these cells become active and create the limb bud. Soon after the upper limb bud, the lower limb begins to form.
- Limb development is induced by the limb bud’s apical ectodermal ridge. The femur originates from the lateral plate somatic mesoderm of the lower limb bud. Endochondral ossification is the process by which bone replaces models of hyaline cartilage. There is no cartilage model for the process of intramembranous ossification, which produces articular cartilages and epiphyseal plates.
- The perimysium, epimysium, and tendons are also produced by the lateral plate somatic mesoderm. The femur muscles are produced by the myotonic component of the somite. The periosteum, which envelops the femur, provides nutrition by way of the nearby blood supply. Strength is provided by the femur’s compact bone, which is strongest in the middle third of the bone where stresses are greatest.
Lymphatics and Blood Supply of the femur bone
Lymphatics and Blood Supply of the femur bone is as described follows ,
- The major blood vessel supplying the lower limbs is the femoral artery. After cross the Ilioinguinal ligament, this artery is the main branch of the external iliac artery. The femoral artery gives rise to the medial and lateral circumflex arteries. Significant anastomotic connections are made between these veins and the obturator artery, which is a branch of the internal iliac artery and supplies the femoral head. The ligamentous teres femoris is crossed by the fovea artery, a branch of the obturator artery that supplies the femoral head with blood.
- The femoral artery splits into the deep and superficial femoral arteries at the level of the lesser trochanter. The shaft and the distal part of the deep femoral artery are supplied by its perforating branches.
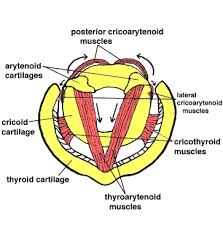
Nerve supply of the femur bone
Nerve supply of the femur bone is as described follows ,
- The longest bones, the big flat bones, and the vertebrae have the highest level of Osseous sensory innervation. The surrounding nerves provide the periosteum with a dense innervation for sensory function. Sensory nerves in bone marrow follow blood arteries. They can be found in the perivascular areas around Harversian canals.
- The proximally located femoral and obturator nerves supply the hip joint, which in turn innervate the periosteum of the femur. The nerves that innervate the knee (common fibular, femoral, obturator, and tibial nerves) supply the distal periosteum. Nerves that innervate muscles also supply the periosteum of the femur. On the posterior part of the femur, medial to the linea aspera, there is a noticeable nutritional foramen. Nerves Here, nutritive blood vessels and sciatic nerves from the tibial division enter to supply the inside of the femur.
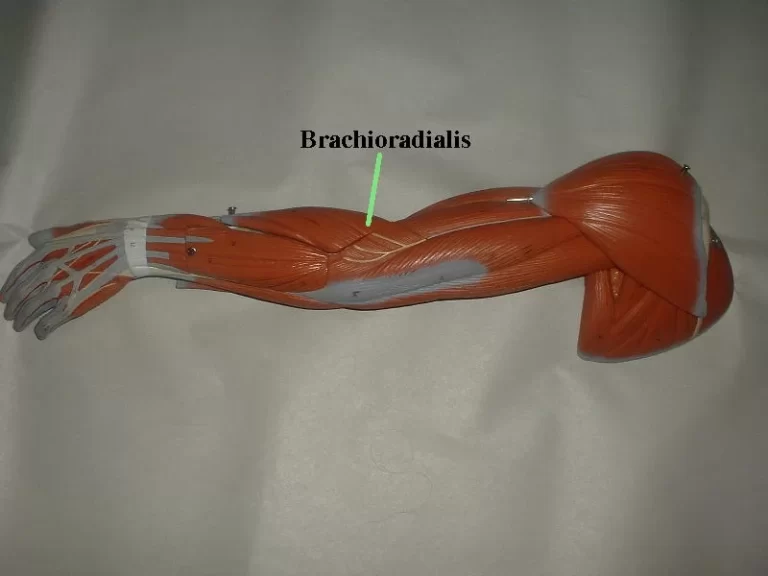
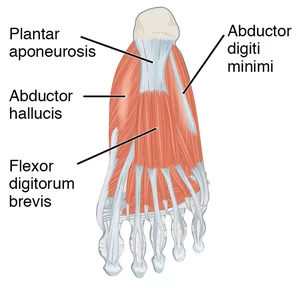
Muscle Attachment of the femur bone
Muscle attachments of the femur bone is as described follows ,
The anterior, medial, posterior, and gluteal compartments comprise the thigh muscles. The anterior compartment contains the femur.
Muscle of the anterior compartment in the femur bone
Muscle of the anterior compartment bone of the femur bone is as described follows ,
- The muscles that make up the anterior compartment are mostly involved in knee extension and hip flexion. The Sartorius, iliopsoas, and pectineus muscles are examples of hip flexors. All hip flexors except for the iliopsoas are innervated by the femoral nerve. The psoas major and iliacus muscles combine to form the iliopsoas muscle, which is the strongest hip flexor.
- The iliacus inserts on the lesser trochanter after emerging from the iliac fossa, iliac crest, and ala of the sacrum. The femoral nerve (L2-L3) innervates the iliacus. The psoas muscle inserts with the iliacus on the lesser trochanter of the femur after emerging from the lateral portion of the T12-L5 vertebrae. The ventral rami of L1–L3 innervate the iliacus. When combined, the iliopsoas is the strongest flexor at the hip.
- The pectineus inserts on the femur’s pectineal line after emerging from the superior pubic ramus. The pectineus, which receives innervation from the femoral nerve, aids in medial thigh rotation and acts as a flexor at the hip. As part of the pes anserine, or “goose’s foot,” the Sartorius inserts on the medial surface of the tibia after emerging from the anterior superior iliac spine of the iliac bone.
- The psoas muscle inserts with the iliacus on the lesser trochanter of the femur after emerging from the lateral portion of the T12-L5 vertebrae. The ventral rami of L1–L3 innervate the iliacus. When combined, the iliopsoas is the strongest thigh flexor at the hip. The pectineus inserts on the femur’s pectineal line after emerging from the superior pubic ramus. The pectineus, which receives innervation from the femoral nerve, aids in medial thigh rotation and acts as a flexor at the hip. As part of the pes anserine, or “goose’s foot,” the Sartorius inserts on the medial surface of the tibia after emerging from the anterior superior spine of the iliac bone. tendon (made up of the semitendinosus, gracilis, and sartorius tendons). The femoral nerve (L2-L3) innervates the Sartorius, which flexes, abducts, externally rotates the thigh, and flexes the leg at the knee. The word “satori” is Latin for “tailor,” which makes sense given that they frequently cuff trousers or hem skirts while seated cross-legged on the ground.
- The FABER muscle is a good way to remember the sartorius. This represents External Rotation, Abduction, and Flexion. Keep in mind that the sartorius only works as a thigh flexor when the leg is stretched to the knee. In the absence of such, the muscle flexes the leg at the knee.
- The rectus femoris, vastus medialis, and vastus lateralis make up the quadriceps femoris muscle. The patella is the result of the attachment of four muscles, and the patellar tendon connects it to the tibial tuberosity. The femoral nerve innervates all of them (L2, L3, L4). (Note that the femoral nerve (L2, L3) innervates the more proximal muscles in this compartment, while the femoral nerve (L2, L3, L4) innervates the quadriceps femoris. The medial lip of the linea aspera is the origin of the vastus medialis muscle. The lateral lip and greater trochanter of the linea aspera give rise to the vastus lateralis. The anterolateral femur is the origin of the vastus intermedius.
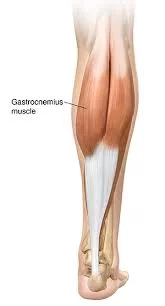
Muscle of the posterior compartment in the femur bone
Muscle of the posterior compartment of the femur bone is as described follows ,
- Hip extensors and knee flexors make up the majority of the posterior compartment muscles. These comprise the semitendinosus, semimembranosus, and biceps femoris muscles. Except for the biceps femoris, the majority of the posterior thigh muscles are innervated by the tibial division of the sciatic nerve (L5, S1, S2). There are two heads to the biceps femoris: the long and short heads. The sciatic nerve’s tibial branch innervates the long head (L5, S1, S2). The sciatic nerve’s common peroneal (fibular) division innervates the short head (L5, S1, S2).
- The gluteal region is organized by the layers of muscles that are superficial and deep. The gluteus maximus, medius, and minimus make up the superficial layer.
- The posterior side of the ilium, sacrum, coccyx, and sacrotuberous ligament give rise to the gluteus Maximus. Strong thigh extensors like the gluteus Maximus come in handy when getting out of a chair or going upstairs. The gluteus Maximus elevates the body to the next level through its action in power extension, whereas the iliopsoas bends the thigh at the hip to reach the next stair.
- The gluteus medius inserts on the lateral aspect of the greater trochanter after emerging from the posterior portion of the ilium between the anterior and posterior gluteal lines. The superior gluteal nerve innervates the gluteus medius (L5, S1). Similar origins can be found for the gluteus minimus on the posterior portion of the ilium. The superior gluteal nerve innervates the muscle, which inserts on the lateral surface of the femur.
- At the hip, both muscles twist the thigh laterally and abduct it. Additionally, they keep the pelvis from lowering when the opposing leg is raised off the ground. The tensor fasciae lata (TFL), which originates from the anterior superior iliac spine and inserts on the greater tubercle on the tibia, also aids in these movements. The superior gluteal nerve (L5, S1) innervates the TFL as well. The quadratus femoris, the superior and inferior gemellus muscles, the piriformis, and the obturator internus make up the deep layer. The anterior sacrum and sacrotuberous ligament give rise to the piriformis muscle, which inserts on the superior edge of the greater trochanter of the femur. S1, S2 ventral rami innervate the piriformis. The bones that encircle the obturator foramen give rise to the obturator internus. The nerve that innervates the obturator internus is located in the L5, S1 region. The greater trochanter’s medial surface is where the obturator internus inserts. When the thigh is extended, all of the deep muscles spin it laterally. They all stabilize the femur head in the acetabulum and abduct the flexed thigh at the hip. The nerve that innervates the obturator internus (L5, S1) innervates the superior gemellus. The femur’s greater trochanter is where the inferior gemellus inserts after emerging from the ischial tuberosity. The quadratus femoris nerve innervates the inferior gemellus (L5, S1). The ischial tuberosity gives origin to the quadratus femoris.
- The nerve that supplies innervation to the quadratus femoris (L5, S1) is responsible for this function. The quadratus femoris stabilizes the femur head in the acetabulum and laterally rotates the thigh at the hip. The external rotation of the hip is aided by these deeper and shorter gluteal muscles.
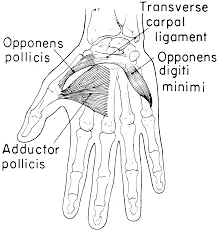
Muscle of the medial compartment in the femur bone
Muscle of the medial compartment of the femur bone is as described follows ,
- The main purpose of the muscles in the medial compartment of the thigh is adduction of the thigh at the hip. The adductor longus, adductor brevis, adductor magnus, gracilis, and obturator externus muscles are the muscles of this compartment. The medial compartment is mostly innervated by the obturator nerve.
- The middle portion of the linea aspera is where the adductor longus penetrates after emerging from the pubis. Innervating the adductor longus is the obturator nerve. The pectineal line and linea aspera are where the adductor brevis inserts after emerging from the pubis. The obturator nerve (L2, L3, L4) innervates the adductor brevis.
- The muscle known as the adductor magnus is hybrid and has two innervations. The anterior half inserts onto the linea aspera after emerging from the ischiopubic ramus. The obturator nerve innervates this muscle, which is an adductor of the thigh at the hip. The posterior portion, which is a hamstring, originates from the ischial tuberosity, inserts onto the femur’s adductor tubercle, and is innervated by the sciatic nerve’s tibial aspect (L4).
- The inferior ramus and body of the pubis give origin to the gracilis, which inserts on the medial aspect of the pes anserine, or goose foot, tendon, extending from the tibia. The obturator nerve (L2, L3) innervates the gracilis, which rotates the thigh laterally and stabilizes the femur head in the acetabulum.
- The obturator externus inserts on the femur’s trochanteric fossa after emerging from the obturator foramen. The obturator externus, which rotates the thigh laterally and stabilizes the femur head in the acetabulum, is innervated by the obturator nerve (L3, L4).
Variation in the femur bone in different animals
variation of the femur bone in different animals is as described follows ,
- The greater and lesser trochanters, as well as a ridge known as the adductor crest that runs down the ventral surface of the femoral shaft, are the primary sites of muscle attachment along the femur in primitive tetrapods. In the most basic versions, the femur’s neck is usually small or non-existent, indicating a straightforward attachment to the acetabulum. Greater trochanters are linked to the loss of the rudimentary sprawling gait and were present in both extinct archosaurs and contemporary birds and mammals. Mammals are the only animals that have developed the lesser trochanter; they do not have greater trochanters. Mammals also frequently lack the adductor crest or have it reduced to a series of wrinkles running the length of the bone. Similar structures to the third trochanter can be found in certain primates and other mammals.
- Vestigial femurs are present in several species of whales, snakes, and other non-walking animals. Certain snakes use the projecting end of a pelvic spur, a vestige of a pelvis, and a femur that is not joined to the rest of the skeleton, for mating purposes. The Basilosauridae, an extinct family of whales with clearly defined femurs, lower legs, and feet, are thought to have played this role in mating. Atavism is the condition in which a modern whale has tiny legs due to a mutation in the genes that code for extended extremities.
- The Eusthenopteron is a lobe-finned fish that lived in the Late Devonian period and is one of the oldest known vertebrates to have a femur.
Metagenomics of viruses
According to a recent study, bone contains far more persistent DNA viruses than previously thought. In addition to hepatitis B and parvovirus 19, 10 other viruses were found, including various polyomavirus and herpesvirus members, human papillomavirus 31, and torque teno virus.
Vertebrates
The term “femur” comes from the study of arthropods in invertebrate zoology. The name “femur” has been adopted by analogy and, when appropriate, refers to the most proximal of the two longest-jointed segments of the arthropod’s legs. However, its usage is not analogous to that of vertebrate anatomy. The coxa and trochanter are the two basal parts that come before the femur. This convention is applicable in technology but not in carcinology.
Clinical Significance
Clinical Significance of the femur bone in different animals is as described follows ,
Hip Disorder in Adolescents
Male teenagers who are overweight are more likely to develop slipped capital femoral epiphysis (SCFE), a hip condition affecting the femoral head. A superior and anterior displacement of the metaphysis concerning the epiphysis is known as SCFE or slipped capital femoral epiphysis. Although idiopathic causes predominate, SCFE (slipped capital femoral epiphysis) has also been linked to radiation therapy, renal insufficiency, and endocrine dysfunction. One common consequence of SCFE (slipped capital femoral epiphysis) is femoroacetabular impingement. Although early treatment with a single screw through the growth plate has been demonstrated to prevent increasing slippage, preventative treatment for SCFE (slipped capital femoral epiphysis) remains contentious.
The modified Dunn method has been investigated recently for severe SCFE. In the modified Dunn method, the deformity is corrected by removing a wedge of the femoral neck, and the femoral head is then immobilized by screw fixation. enduring hip With the modified Dunn treatment, post-operative problems such as discomfort and avascular necrosis were prevalent.
Vascular related disorders
A rare childhood condition known as Legg-Calve-Perthes disease (LCP) results from a disruption in the blood supply to the femoral head. Limping and hip pain are among the symptoms. Boys are five times more likely to have LCP (Legg-Calve-Perthes disease), which often manifests around age 4 to 8. According to twin research, environmental factors including poor social status increase the likelihood of LCP (Legg-Calve-Perthes disease). Congenital deformities such as Down syndrome, inguinal hernias, and genitourinary disorders are also linked to LCP (Legg-Calve-Perthes disease). The age and stage of the disease determine the course of treatment. Treatment options for LCP( Legg-Calve-Perthes disease) include exercise, acupuncture, braces, bisphosphonates, and hip arthroscopy.
Environment related disorders
The incapacity of rickets to mineralize bone causes a differ malformation of the long bones. The growth plate calcifies and encourages the formation of long bones mostly by endochondral ossification. But with rickets, this mechanism is either diminished or non-existent. The most frequent cause of rickets is a lack of vitamin D. Reduced sun exposure, an irregular phosphate metabolism, and inadequate calcium or phosphate intake are some additional factors.
Fractures of the femur
The medical word for shattering a bone is a bone fracture. Femurs are the strongest bones that are generally fractured by severe traumas, falls, or auto accidents.
- Stress on the part
- Growing bone
- Sensitivity of bone
- unable to move your leg as freely as you normally can do with the femur of the lower extremities of the body.
- Any discoloration or bruises. Or something abnormal is occurring in the femur.
- a lump or malformation that is unusual for your body.
- Visit the hospital’s emergency department as soon as you think you could have a fracture or have experienced trauma.
- Unpleasant abnormal feeling at the end of the femur.
Usually, there aren’t any overt signs.
Individuals who are born with a female gender assignment, women, and adults over 50 are more likely to develop osteoporosis. Make an appointment for a bone density test with your doctor; this can help detect osteoporosis early on and avoid fractures.
Patellofemoral pain Syndrome (PFPS)
Pain beneath and surrounding your kneecap (patella) is known as patellofemoral pain syndrome (PFPS). PFPS (patellofemoral pain syndrome) can result from anything, including wearing new shoes or overusing your knees. PFPS (patellofemoral pain syndrome) symptoms include:
- discomfort felt when bending your knee, such as when crouching or climbing stairs.
- soreness during a period of bent knee sitting.
- When you stand up or walk stairs, your knee may make crackling or popping sounds.
- discomfort that gets worse as you alter the sports equipment, playing surface, or level of exercise.
- Consult your provider if having severe pain.
Bursitis
Any joint in the body, including the hip and knee, can develop bursitis. It happens when the bursa, a little fluid-filled sac that facilitates joint movement, becomes inflamed. An injury, an illness, or overuse may cause this.
Femoral ante version
A disorder called the femoral ante version first manifests in childhood. It occurs when the femur bones twist inward, causing the knees and toes to be positioned inside.
Legg calve Perthes disease (LCP)
Legg calve Perthes disease is an uncommon hip joint disorder that affects children. Blood flow to the femur’s head is impacted. Osteonecrosis is the term for the condition where bone tissue dies due to a shortage of blood.
Diagnosis of the femur bone
Diagnosis of the femur bone is as described follows ,
A bone density test is the most popular test used to evaluate the condition of your femur. It is sometimes referred to as a DXA or DEXA scan. A bone density test uses low doses of X-rays to gauge how strong your bones are. It serves as a gauge for bone loss with aging.
Your surgeon or healthcare practitioner may recommend imaging studies if you have had a femur fracture. These tests may include:
- radiography which is known as x-rays.
- Imaging with magnetic resonance (MRI).
- CT scan.
Surgical consideration of the femur bone
Operative treatment of the femur bone is as described follows ,
- Osteoporosis is more common in older female patients, increasing their risk of fractures from falls that occur from a low height. Young individuals frequently suffer femoral fractures from high-energy trauma, such as car crashes or falls from a considerable height, because of the femur’s strength. To enable patients to walk sooner and enjoy a higher quality of life, all femur fractures are treated surgically unless they present with serious comorbidities or significant surgical risk.
- Aseptic non-union, per prosthetic fracture, and avascular necrosis are the primary problems that result in surgical revision. Depending on the fracture form and features, internal fixation or arthroplasty may be the better course of action for a proximal femur fracture.
- The blood flow from the deep branch of the medial femoral circumflex artery is more likely to be disrupted by an intracapsular fracture involving the femoral neck than by an extra scapular fracture. Therefore, if treated with intramedullary (IM) nails and screws, The modified Dunn method has been investigated recently for severe SCFE. In the modified Dunn method, the deformity is corrected by removing a wedge of the femoral neck, and the femoral head is then immobilized by screw fixation. enduring hip With the modified Dunn treatment, post-operative problems such as discomfort and avascular necrosis were prevalent.arthroplasty involving replacement of the femoral head is more suited to avoid the risk of avascular necrosis. There are many options for consideration of the surgical operation of the femur bone to get back the function of the femur along with weight bearing.
- Femoral neck fractures can be categorized using the Garden classification system and are assessed using plain film X-rays.
- Garden I is a less displaced or valgus-decided incomplete femoral fracture of a neck fracture.
- Garden II has very little displacement and is a complete fracture.
- Garden III is a total collapse with minimal shift in position.
- Garden IV is a fully fractured area that has seen over 50% displacement. Femoral neck fractures, however, are primarily categorized as displaced (Garden I and II) or not displaced (Garden III and IV) due to the difficulty in classifying the fractures on an x-ray.
- Sliding hip screws or cancellous lag screws are used to treat no displaced fractures. About the same results and issues arise from both procedures. Less blood loss and a faster recovery period are linked to cancellous lag screws. However, because the lag screw head prominently irritates soft tissue when the femoral neck naturally shortens after surgery, cancellous lag screws have a greater revision rate than sliding hip screws.
- Since more than half of distal femur fractures are intra-articular and the type of surgical therapy relies on whether there is joint space involvement, distal femur fractures are difficult injuries that should be diagnosed by CT scan. Intramedullary (IM) plates, screws, blades, or anterograde or retrograde nails are used to repair extra-articular fractures. When compared to open reduction internal fixation with a plate, blade, or screws, retrograde internal fixation yields better results and fewer rates of revision and infection. Results from anterograde IM nails are similar to those from retrograde IM nails. Retrograde intra-articular nails can be used to repair certain stable and no displaced intra-articular fractures; nonetheless, total knee arthroplasty (TKA) is the recommended treatment for the majority of intra-articular fractures. However, the morbidity and mortality rate for older TKA patients is significant, therefore selection plays a major role.
How to keep the femur bone healthy?
You can keep your bone (and general) health in check by maintaining a healthy diet and exercise routine as well as by visiting your doctor for routine examinations. Speak with your healthcare practitioner about getting a bone density scan if you are over 50 or if osteoporosis runs in your family.
Use these general safety recommendations to reduce your risk of injury:
- Always fasten your seatbelt.
- When engaging in any sport or activity, wear the proper safety gear.
- Check your home or place of business to be sure nothing could hurt you or anybody else.
- Always use the proper tools or equipment while reaching for anything at home.
- Take a good diet and always ask to nutrionist or dietitian for help to guide a diet for you to make your bones healthy and strong.
- Follow a nutritional and activity plan that will strengthen your bones.
- Use a walker or cane if you have difficulty walking or are prone to falls.
Summary
- The thigh bone is called the femur. It’s essential to your capacity to move and stand. Numerous vital muscles, tendons, ligaments, and sections of your circulatory system are also supported by the femur.
- Your femur typically breaks after a significant trauma, such as a fall or auto accident, Should you suffer a fracture, you probably require both physical therapy to help you restore your strength and mobility and surgery to fix your broken bone. Osteoporosis can affect your femur just like it might affect other bones.
FAQs
The pyramid-shaped neck at the proximal end is connected to the spherical head at the apex and the cylindrical shaft at the base. Two prominent bone protrusions that link to the muscles that move the hip and knee are called the greater and lesser trochanters.
In healthy individuals, the anatomic tibiofemoral angle is valgus with an offset of 4-6°. Anatomic mechanical femoral angle in patients with osteoarthritis of the knee ranges from 1.5° to 7°.
The pectineus, iliacus, sartorius, psoas minor, iliopsoas, and quadriceps are the muscles of the anterior femur.
Femur bone is the strongest bone of lower extremities of the human body.
yes, it is included in the category of long bone.
The profunda femoris, which is the deep penetrating branch of the upper thigh, is a branch of the femoral artery, and the medial and lateral circumflex branches of this branch provide the greatest portion of blood supply to the head of the femur.
One of the most widely used measurements to evaluate hip morphology is the femoral neck-shaft angle (NSA), also known as the caput-collum-diaphyseal (CCD) angle. This angle specifically measures the relationship between the femoral shaft and the femoral head-neck axis.
Similar to biparietal diameter (BPD), femur length (FL) is a foetal biometric parameter that measures the longitudinal growth of the longest bone in the foetus. It starts to rise at around 1.5 cm.
References
- Professional, C. C. M. (n.d.-k). Femur. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22503-femur
- BSc, L. C. M. (2023, September 11). Femur. Kenhub. https://www.kenhub.com/en/library /anatomy/femur
- Femur. (n.d.). Physiopedia. https://www.physio-pedia.com/Femur
- Wikipedia contributors. (2023a, October 15). Femur. Wikipedia. https://en.m.wikipedia.org/wiki/Femur
- Chang, A. (2023, November 17). Anatomy, bony pelvis and lower limb: femur. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov /books/ NBK532982 /#:~:text= The%20femur%20is%20the%20longest,move%20the%20hip%20and%20knee.
- Femur shaft fractures (Broken thighbone) – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/ diseases–conditions/femur-shaft-fractures-broken-thighbone/
- TeachMeAnatomy. (2020b, November 13). The femur – proximal-distal – shaft – TeachMeAnatomy. https://teachmeanatomy.info/lower-limb/bones/femur/
- Hip anatomy. (n.d.). Physiopedia. https://www.physio-pedia.com/Hip_Anatomy
- Emt-P, R. B. (2022, October 28). The anatomy of the femur. Verywell Health. https://www.verywellhealth.com/femur-anatomy-4587598
- Admin. (2022b, August 26). Femur structure and function. BYJUS. https://byjus.com /neet/ femur-structure-and-function/
- Vedantu. (n.d.). Femur. VEDANTU. https://www.vedantu.com/biology/femur
- Zomorodi, C. (2022, December 13). What to know about the femur Bone. WebMD. https://www.webmd.com/a-to-z-guides/femur- what-to-know more about it