Knee Pain at the Back of the Knee
Table of Contents
What is a Knee Pain at the Back of the Knee?
Knee pain at the back of the knee can be a challenging and discomforting issue that affects individuals of all ages and activity levels.
The largest joint in the human body and one of the most prone to damage is the knee. It is composed of tendons, ligaments, and cartilage that can tear or strain, as well as bones that can fracture or come out of joints.
One of the most common complaints from patients is Knee Pain in the Back of the Knee. Compared to the posterior portion of the knee, knee discomfort is more common in the anterior, medial, and lateral regions of the joint. A variety of pathologies affecting the bones, musculotendinous structures, ligaments, and/or bursas are possible differential diagnoses for Knee Pain at the Back of the Knee.
Vascular and neurologic damage are less frequent. Additionally, there are tumors like osteochondromas, which are bony tumors that typically develop close to the end of a long bone and contain both bone and cartilage.
A muscle or tendon injury may be indicated by tenderness while palpating the tendons or muscles in the back of the knee. A cyst or effusion may be indicated by pain or swelling in the popliteal region. To properly diagnose and treat posterior knee pain, one must have a thorough awareness of the anatomy of the knee, the physical examination, and differential diagnosis.
With rest and attention, certain knee injuries can eventually heal on their own. Others need to have surgery or other treatments. Pain can occasionally be an indicator of a chronic illness like arthritis, which steadily decreases the knee over time.
Back or knee pain not only makes it difficult to walk and perform daily tasks, but it can also have a significant impact on your sleep.
There could be severe pain at the back of the knee, swelling limiting leg movement, or a general soreness. The discomfort could be confined mostly to the back of the knee, or it could spread down and cause calf pain.
Generally speaking, one of the most sensitive musculoskeletal problems is pain in the knee. Multiple etiologies include tears in the muscles, tendons, nerves, and blood clots. However, early and accurate diagnosis is the key to managing it effectively, much like with most other problems.
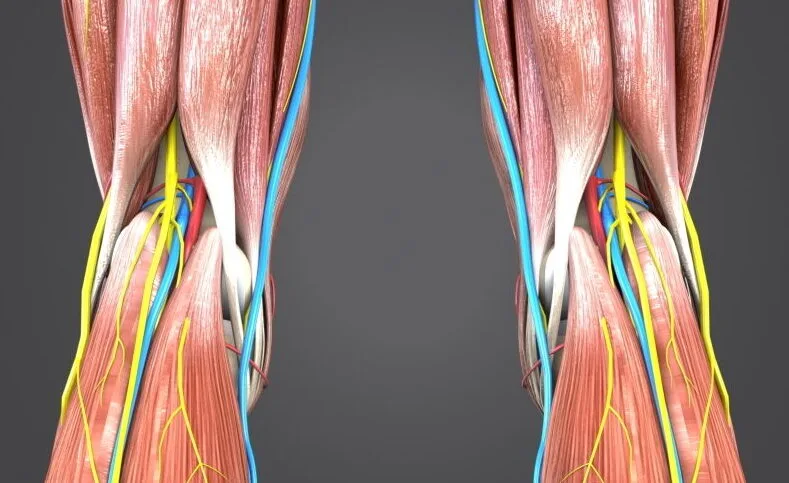
Anatomy
When diagnosing posterior knee discomfort, the anatomy of the knee is crucial. The intricate web of ligaments, muscles, and other soft tissues that surround the knee helps to support and form the joint. Both passive and active stabilizers are among them.
- Active stabilizers: The hamstrings, extensor mechanisms, and popliteus muscle are examples of active stabilizers.
- Passive stabilizers: The medial collateral ligament (MCL), lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL) are examples of passive stabilizers.
Two muscle groups that are significant to the anatomy of the posterior knee are the hamstring complex and the gastrocnemius. The semimembranosus and semitendinosus, which are situated medially, and the biceps femoris, which are positioned laterally, make up the hamstring muscle group.
When assessing posterior knee discomfort, the anatomy of the popliteal fossa must also be taken into consideration. Other components of the popliteal fossa include bursae, lymph nodes, fat, vascular structures (small saphenous vein, popliteal artery, and popliteal vein), and nerves (posterior femoral cutaneous, common peroneal, and tibial).
The knee’s bursae are sacs lined with synovium that reduce friction in moving parts. The bursa’s pain and swelling are brought on by inflammation, outside pressure, or overuse.
Causes of posterior Knee Pain
The following list of conditions can result in pain behind your knee, along with what to expect if you have any of them:
- Leg cramps:
While the calves are the most common muscles to cramp, other leg muscles, like those at the back of the thigh near the knee, can also be affected.
Leg cramps are more likely to happen after strenuous activity or during pregnancy. Additional potential reasons include the following:
- Nerve issues in your lower limbs
- Liver disease
- Dehydration
- Infections, such as tetanus
- Poisons, such as lead or mercury, in the blood
Muscles will suddenly contract, or spasm, when you have a cramp. The average duration of the suffering is between ten minutes and a few seconds. After the spasm, the muscle can hurt for a few hours. Here’s how to get rid of the pain and common leg cramps from happening again.
- Jumper’s knee
The tendon, which attaches your kneecap (patella) to your shinbone, is injured in the jumper’s knee. Another name for it is patellar tendonitis. When you jump or change direction, like when playing basketball or volleyball, it can happen.
Tiny tears in the tendon may result from these motions. The tendon eventually swells up and becomes weaker.
The jumper’s knee causes pain under the kneecap. With time, the condition becomes worse. Additional signs and symptoms consist of the following:
- Weakness
- Stiffness
- Difficulty in bending or straightening the knee
- Biceps femoris tendonitis (hamstring injury)
Three muscles pass down the back of your thigh and make up the hamstring:
- Semitendinosus muscle
- Semimembranosus muscle
- Biceps femoris muscle
You can bend your knee with the help of these muscles.
An injury to one of these muscles is referred to as a pulled hamstring or hamstring strain. A hamstring strain is the result of overstretching the muscle. It’s possible for the muscle to rip completely, and recovery could take months.
When your hamstring muscle is injured, you will feel excruciating pain. Biceps femoris tendinopathy, a muscle injury, is the cause of discomfort in the back of the knee.
- Bruises
- Edema
- Weakness in the rear leg
Sportsmen who run quickly, such as those involved in soccer, basketball, tennis, or track. Stretching the muscles before playing can help prevent this injury.
- Baker’s cyst
A Baker’s cyst is a fluid-filled sac that appears behind the knee. Synovial fluid is the term for the fluid found inside the cyst. This fluid normally lubricates your knee joint. Nevertheless, if you have arthritis or a knee injury, your knee may produce too much synovial fluid. The extra fluid could build up and become a cyst.
Among the symptoms are:
- Discomfort behind and inside your knee
- Edema behind the knee
- Stiffness and difficulty bending the knee
- Being active can aggravate these problems. If the cyst breaks, your knee will hurt sharply.
Sometimes, Baker’s cysts disappear by themselves. For the treatment of a large or painful cyst, you could need physical therapy, steroid injections, or cyst extraction. It’s essential to determine whether an underlying condition, such as arthritis, is the source of the cyst. If so, treating this issue first might cause the Baker’s cyst to disappear.
- Calf strain, or gastrocnemius tendonitis
Your calf, or back of the lower leg, is made up of the gastrocnemius and soleus muscles. These muscles assist you in pointing your toes and bending your knees.
Tennis and squash are two games where quick changes from a standing to a running stance can result in tension or rips in the gastrocnemius muscle. The acute discomfort in the back of the leg that this muscle produces will indicate whether you’ve strained it.
Additional signs and symptoms consist of the following:
- Discomfort and oedema in the calf
- Soreness in the calf
- Difficulty walking on tiptoe
Depending on the size of the rip, the pain should go away. It will recover more quickly if you rest, elevate the damaged leg, and apply ice to the area.
- Tear in the meniscus
A wedge-shaped piece of cartilage that stabilizes and cushions your knee joint is called a meniscus. There are two menisci in each knee, one on each side of the knee.
An athlete runs the risk of tearing the meniscus when they squat and twist their knee. As you age, your meniscus weakens and degenerates, making it more likely to tear from any twisting motion.
Torn meniscus membranes can make a “popping” sound. Initially, the damage might not hurt. However, after a few days of walking on it, the knee can suffer even worse.
Additional signs of a meniscus tear include:
- Knee stiffness
- Edema
- Weakness,
- Locking or buckling of the knee
- Knee movement decrease
The afflicted knee can mend more quickly and get symptom relief with rest, ice, and elevation. It could need to be surgically repaired if the rip does not mend itself.
- Anterior cruciate ligament injury
The anterior cruciate ligament (ACL) is a band of tissue that goes through the front of your knee joint. It joins the thighbone to the shinbone, which helps support and move your knee.
Most ACL injuries happen when a runner stops, slows down, or changes direction suddenly. Additionally, you could sprain or tear this ligament if you land a jump poorly or are struck in a contact sport like football.
The wound may “pop” at that point. After that, your knee will hurt and swell. Walking may hurt, and you could find it difficult to extend your knee to its maximum length.
An ACL strain can be managed with physical treatment and rest. Surgery is frequently required if the ligament is injured to fix it. This is what to expect when your ACL is reconstructed.
- Posterior cruciate ligament injury
Note that, compared to the ACL, the PCL is less prone to injury.
The PCL may be injured if there is a strong blow to the front of the knee, such as in a car accident. Sometimes walking might cause injuries due to knee twisting or neglecting to take a step.
Overstretching a ligament results in a strain. If the pressure is applied enough, the ligament could split in two.
Apart from discomfort, a PCL injury causes:
- Stiffness
- Edema in the knees
- Difficulty walking
- Knee weakness
An injury to the PCL can heal more quickly with rest, ice, and elevation. If you have damage to more than one ligament in your knee, experience instability, or have damaged cartilage, you may require surgery.
9. Chondromalacia:
When a joint’s cartilage degenerates, a condition known as chondromalacia results. The stretchy substance called cartilage keeps your bones from rubbing against one another when you move.
Chondromalacia can result from a knee injury or the knee gradually wearing down due to ageing, arthritis, or abuse. The most common site of cartilage degradation is the patella, or region under the kneecap. The knee bones rub against one another and hurt when the cartilage is gone.
The primary complaint is a dull discomfort located behind the kneecap. If you climb stairs or sit for a long period of time, the pain can get worse.
Additional signs and symptoms consist of the following:
- Difficulty extending your knee past a certain point,
- Buckling or weakening in the knee
- A grinding or cracking sensation when bending and straightening the knee
Physical therapy, ice packs, and over-the-counter painkillers can all help with discomfort. Chondromalacia is a permanent condition once cartilage is damaged. The damage to the cartilage can only be fixed surgically.
- Arthritis
The cartilage that supports and cushions the knee joint eventually deteriorates as a result of the degenerative disease known as arthritis. The following types of arthritis can affect the knees:
- Of these, osteoarthritis is the most prevalent. Your cartilage increasingly deteriorates with age.
- An autoimmune condition called rheumatoid arthritis occurs when the body’s defenses wrongly target the joints.
- Another autoimmune condition that inflames the knees and other joints is lupus.
- Psoriatic arthritis is characterized by painful joints and rough patches of skin on the skin.
- Physical activity, medications, and injections can all be used to manage arthritis symptoms.
- Disease-modifying medications, which reduce inflammation in the body and attenuate immune system responses, are used to treat rheumatoid arthritis and other inflammatory types of illness in the body.
- Deep vein thrombosis:
Deep vein thrombosis (DVT) is the term for a blood clot that forms in a deep vein inside the leg. It’s likely that you’ll experience leg pain, especially when standing. This is the method used to identify a blood clot.
Additional signs and symptoms consist of the following:
- Warmth and swelling in the leg
- Red skin
When a clot becomes caught in a lung artery, it causes a pulmonary embolism (PE). PE raises the possibility of being dangerous.
DVT is treated with thinners. These drugs prevent the clot from getting bigger and from forming new clots. Your doctor may prescribe thrombolytics to break up large, potentially hazardous clots more quickly.
Differential Diagnosis:
Posterior knee pain can be caused by some conditions:
- Semimembranosus tendinopathy
- Biceps femoris tendinopathy
- Hamstrings strain
- Calf strain
- M. popliteus strain
- M. popliteus tendinitis
- Posterior cruciate ligament injury
- PLC: Posterolateral corner/posterior complex
- Knee Bursitis
- Common peroneal nerve injury
- Baker Bursitis
- popliteal artery entrapment syndrome, aneurysms
- Deep venous thrombosis (DVT)
Referred pain from conditions like sacral radiculopathy, lumbar facet arthropathy, sacroiliac joint dysfunction, and intra-articular hip pathology can also cause posterior knee pain. Alternatively, it may result from entrapment of nerves in the popliteal fossa and peripheral neurological damage.
Diagnosis
Multiple tests and imaging results are used to make the diagnosis. A thorough medical history is often taken by the physician, who then performs a clinical examination.
Active and fit people often have inflammation and tears in their soft tissues, such as the meniscus, cartilage, and tendon. An increasing number of older people report having pain in their posterior knee due to cysts or arthritis.
Your physician will inquire about:
- your level of physical activity and the symptoms you’re feeling
- Any pain-relieving medication you’ve tried when the symptoms arise
- Your physician will perform a physical examination of your knee, feel for any painful areas, and bend and extend your leg to measure your knee’s range of motion.
In order to assess whether there is any damage to the tendon or bone, your doctor may also prescribe imaging tests to examine your kneecap and tendon. Additionally, by ruling out other potential reasons of your discomfort, such a fracture, these tests can help.
Ultrasonography, MRIs, and X-rays are used to find underlying damage.
- X-ray to examine the bone and see whether you have a fractured or misplaced kneecap.
- MRI to examine the tendon and reveal any soft tissue damage
- Ultrasound to examine the tendon and detect any injury to the soft tissues
Treatment of Knee Pain at the Back of the Knee
Although it may not provide defense against all traumatic origins of knee pain, this may enhance the way the muscles respond to physical activity.
Doctors usually recommend the RICE approach to help reduce pain and swelling when an injury initially occurs.
RICE is an acronym for:
- Resting: Give rest to the affected leg.
- Icing: Apply ice to the affected knee.
- Compressing: Wrap the elastic band around the knee to reduce swelling.
- Elevating: Elevate the injured leg
The RICE method can frequently aid in reducing oedema and pain. But since he first used the phrase in 1978, Dr. Gabe Mirkin has said that applying ice to injuries can postpone their healing. When deciding what course of action is best for them, people should speak with a physician or physical therapist.
While the knee heals, taking nonsteroidal anti-inflammatory medicines (NSAIDs) can also help reduce discomfort and swelling. Some NSAIDs can be bought online, including ibuprofen.
In rare circumstances, a physician could advise steroid injections to lessen symptoms.
In cases of more severe injuries, medical professionals could perform a CT or MRI scan to get a full picture of the affected area. Afterwards, based on the condition, they may recommend physical therapy or surgery as therapies.
Medical treatment:
SMT (semimembranosus tendinopathy): It may be possible to effectively relieve the symptoms with one or more injections at the insertion site of 3 mL of 2% lidocaine and 10 mg triamcinolone.
Surgical rerouting and tendon reattachment is a rare yet potentially beneficial procedure.
Physical therapy treatment:
- SMT(semimembranosus tendinopathy)
Without additional treatment, this illness will resolve in over 90% of cases.
- The first line of conservative treatment consists of ice packs, relative rest, pain-relieving modalities, a brief course of NSAIDs, and physical therapy activities that target the hamstrings.
- In patients with genu valgum, SMT may benefit from appropriate shoe fitting to avoid overpronation or a medial heel lift. Stable running shoes and shoes with motion control technology are examples of shoes that fit properly because they offer additional support and stop your ankle from rolling inward suddenly. It is even more crucial to wear these shoes if you are overweight. The medial post, the heel’s engineering, and the plastic shank beneath the arch are the three primary components of stability. E.g., Nike Zoom Structure Triax 15
2. Hamstring strain:
ICE (rest, ice, compression, and elevation) is a technique for treating hamstring strains that accelerate healing. Heat treatments, such as hot packs, whirlpools, or preheating before stretching exercises, might be employed after the acute phases. To reduce pain and inflammation, ice treatment should be applied after every activity.
- First phase: The athlete starts pain-free submaximal isometric strengthening at various angles.
Exercise: The injured limb is placed on top of the contralateral limb, and the strained hamstring is contracted to complete a set of isometric contractions at 30°, 60°, and 90° of knee flexion by the athlete. At this point, it is best to preserve the available hip and knee range of motion rather than stretching the hamstring into a painful range. Additionally, motion helps to align the fibres and strengthen their lateral adhesion, which keeps the damaged fibres from separating from the stump. The objectives of this stage are normalizing gait and achieving knee flexion strength at more than 50% of undamaged length following manual muscle testing at 90 degrees of knee flexion.
When sitting, perform an isometric knee flexion. Keep in mind that this would perform at multiple angles.
- The second phase: To prepare for movements particular to their sport, the athlete gradually regains strength across the range of motion and enhances neuromuscular control of the hips and pelvis. If end-range lengthening is uncomfortable at this point, avoid doing so.
Exercises: To obtain eccentric training, execute movements like the Nordic hamstring exercise, single-leg windmills, and straight-leg deadlifts with an isokinetic dynamometer if one is available.
(Eccentric) Single-leg windmills: Maintaining lumbar lordosis and the stance leg straight, the patient places the uninjured leg on a chair or fixed surface and reaches down in a diagonal plane.
As demonstrated, it can be done without (beginning) weights and advanced with kettlebells or hand-held weights.
Nordic hamstring exercise: The Nordic hamstring exercise is performed with the patient in tall kneeling with the clinician holding their feet. When the patient can no longer control their descent, they slowly fall forward while keeping their hips neutral and then use their upper extremities to propel themselves back into the starting position.
You can use elastic assistance that is fastened to the wall to perform the Nordic hamstring exercise in place of a helper or therapist.
After this phase, the athlete should have full strength upon manual muscle testing (5/5) or be within 20% of the uninjured leg in the zero to 90° range when measured with a hand-held or isokinetic dynamometer to progress to the next phase. At this time, the athlete should also be able to jog at a moderate pace both forward and backward without experiencing any pain.
- Third phase: The focus is on functional movements and eccentric strengthening in the lengthened state. Plyometric and sports-specific training may be initiated, as well as advanced balance exercises. Without the use of a dynamometer, alternative lengthened-state eccentric training can be accomplished by having the affected leg rest on the subject’s chest and using an elastic resistance device, such as a theraband, cable column, or manual resistance, to resist an external force.
Lengthened eccentric state training with the Biodex: Using a setup, the Biodex can be adjusted so that the patient passively stretches and flexes their knee to its maximum range of motion while their hips are in flexion. As the knee is stretched, the patient resists the passive action.
Lengthened state eccentric training on cable columns: The patient can perform this exercise while lying supine and linked up to an elastic resistance or cable column, bringing their knee firmly into their chest. The patient then flexes the knee with the help of his or her arms, and as the cable or elastic band pulls the knee into extension, the patient gradually resists it eccentrically. After reaching this point, the athlete ought to be fully strong throughout their range of motion and capable of carrying out any activity linked to their sport without any difficulties.
Summary
Pain behind the knee might occasionally indicate a major problem. A doctor should be contacted by anyone who is suffering from severe symptoms or symptoms that last for a longer period of time.
Observing a physician’s recommended course of action can help ensure that the injury heals properly and doesn’t worsen.
FAQs:
You might need to elevate your leg and knee as you sleep if you have knee pain. If so, the ideal position to sleep is on your back. To raise one’s knee above the level of the heart, place a pillow beneath both legs. The elevation can aid in reducing knee oedema if it exists.
Usually, the knee pain may intensify and create discomfort behind the knee and surrounding area after walking for a while (around 30 minutes). After you stop walking, the pain should normally go away in a few hours if osteoarthritis is the cause of your knee pain.
Your knee locks, clicks, and buckles. There is a deformation or abnormality in your knee. You can’t flex your knee and find it difficult to fully extend. There is a significant amount of warmth, redness, or swelling around the knee.
Once more, if you have sprained, dislocated, or, worst-case, cracked your kneecap, you should apply RICE (rest, ice, compress, elevate) to the affected area for at least 48 hours. But eventually, for those with long-term (chronic) arthritis, walking may be helpful.
Ankle injuries, rheumatoid arthritis, osteoarthritis, cysts, misuse, ageing-related wear and tear, and, in extremely rare instances, malignancy are among the several possible reasons for posterior knee pain. When your leg muscles tense up, leg cramps happen.