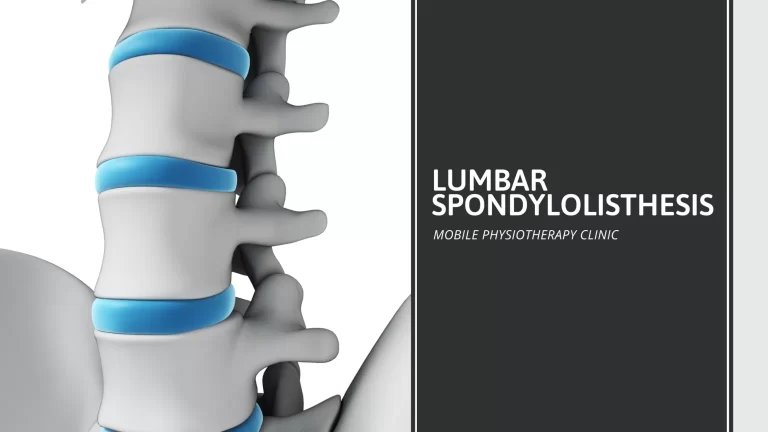
Lumbar Spondylosis
Even in healthy individuals, the cartilage (discs), joints, and bones in the lower back slowly deteriorate over the years due to normal wear and tear on the body. This age-related condition is called lumbar spondylosis. It’s also frequently called arthritis of the lower back and results in chronic lower back pain that worsens with age and increases with movement. When this condition occurs in the neck, it’s called cervical spondylosis.
Spondylosis is common and worsens with age. This condition is often used to describe degenerative arthritis (osteoarthritis) of the spine. Most people don’t have symptoms, but some may experience pain or muscle spasms.In many cases, no specific treatment is required. If symptoms occur, treatments include medication, corticosteroid injections, physiotherapy and sometimes surgery.
Table of Contents
Symptoms of Lumbar Spondylosis
In most cases, lumbar spondylosis only causes noticeable symptoms when the spinal cord or nerves around the spine become irritated or compressed. When symptoms do occur, they can differ greatly from person to person. For example, if there is pressure on the sciatic nerve, it can cause pain in the back, buttocks, legs, feet, and toes.
Common symptoms of lumbar spondylosis that may vary from case to case include:
- Intermittent back pain that may radiate to the extremities
- Joint or muscular stiffness upon awakening
- Muscle weakness and/or tingling in the back, buttocks, legs, and other affected areas
- Numbness or loss of sensation in the affected areas
- Tenderness in the area of nerve compression
- Loss of bowel or bladder control
- Limited range of motion in affected joints
Causes of Lumbar Spondylosis
The spine is made up of several motion segments stacked on top of one another to allow your spine to move smoothly. Each segment has three major points of contact including two facet joints and an intervertebral disc, similar to a three legged table. When facet joints and intervertebral discs degenerate or experience trauma, the protective cartilage wears away and new bone spurs form. The spurs can push on surrounding structures leading to symptoms. Some people develop spondylosis at an earlier age depending on certain risk factors including history of trauma, history of smoking, genetic predisposition, or occupations requiring hard labor. These changes may lead to malalignment, stiffness, pain, or abnormal changes to motion.
Risk Factors of Lumbar Spondylosis
Genetics is a risk factor for spondylosis. If many people in a family have spondylosis, the risk is likely to be a stronger genetic predisposition to spondylosis.
Spinal injury is also a risk factor for spondylosis. Injuries can cause intervertebral discs to herniate. Also, osteoarthritis is more likely to develop in injured joints, including joints in the spine. This can take years to develop.
Preventions of Lumbar Spondylosis
Prevention of Lumbar Spondylosis is very easy by just following some tips:
- Develop a regular fitness routine: Regular exercises and fitness routine keeps the body and spine flexible by giving you strong back and abdominal muscles
- Lose weight if necessary: Excess weight puts added stress on your lower back, so losing some extra kilos will surely help.
- Eat healthy, nutritious foods: Having healthy and nutritious diet will not make you obese or earn those extra kilos. It will even keep your bones well nourished and strong
- Take breaks throughout the day: Taking breaks will help you relax your joints, as being in one position creates stiffness
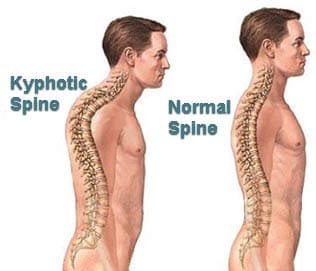
- Develop good posture: Keeping good posture help maintain healthy spine and lumbar
- Learn how to lift properly: When lifting heavy things, try to lift keeping your back straight to avoid sprain or bone twisting
- Get plenty of sleep: Sleeping relaxes both mind and body, so more sleep creates better and healthy spine
- Stop smoking: As rightly said, smoking slowly kills you from inside, not only it deteriorates your lungs but also your bones. This is usually not a visible sign but your doctor might say this.
- Avoid heavy use of alcohol: Heavy boozing makes you lose your senses, so a good posture might not be maintained.
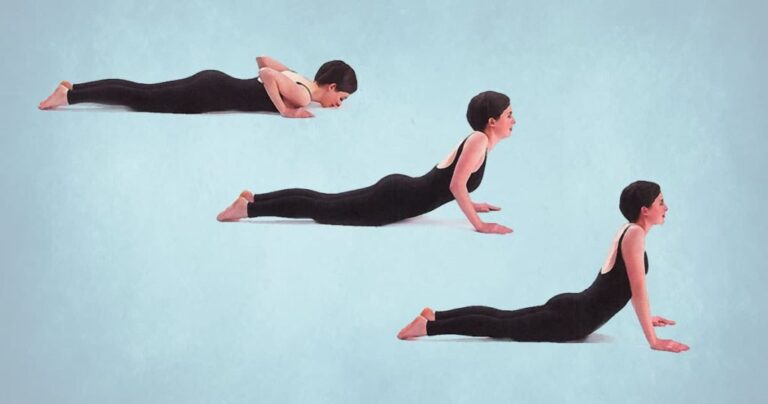
Exercises of Lumbar Spondylosis
Although some cases of lumbar spondylosis may need surgery, the American Academy of Orthopaedic Surgeons recommends trying noninvasive treatments first. Your doctor is likely to suggest some strengthening exercises or recommend physical therapy to give you guidance on similar exercises. There are plenty of easy moves you can try at home to build strength and improve flexibility.
Pelvic Tilt:
Pelvic tilt exercises engage some of your core muscles, which helps provide stability for your lower spine.
Step 1: Lie on your back with your knees bent and your feet flat on the floor.
Step 2: Pull your belly button in toward your spine using your abdominal muscles and flatten your lower back onto the floor.
Step 3: Keeping your core muscles engaged, hold the position for 15 seconds, and then relax.
Repeat the exercise 5 to 10 times.
Knee to Chest:
This exercise works the deep muscles of your core, again, helping stabilize your spine and relieve pain.
Step 1: Lie on your back with your knees bent and your feet flat on the ground. Keep your arms by your sides and your palms face down.
Step 2: Engage your core muscles by pulling your belly button inward toward your spine.
Step 3: Using your arms for extra stability, pull one of your knees up toward your chest. Hold the position for 5 seconds and relax back to the start position.
Step 4: Repeat the stretch with your other leg, pulling your knee to your chest and holding for a count of 5 before returning to the starting position.
Step 5: Finally, complete the same stretch by pulling both knees to your chest, counting to 5, and relaxing back to the starting position.
Repeat this sequence 2 to 3 times, ideally once in the morning and again at night.
Quadruped Arm and Leg Raise
Also called the bird dog exercise, the quadruped arm and leg raise target core muscles to build strength in your abdomen, hip flexors, glutes, and spine.
Step 1: Start on your hands and knees.
Step 2: Raise one arm and the opposite leg straight out while tightening your core.
Step 3: Hold the position for 5 seconds, and then lower your arm and leg back to the starting position.
Step 4: Repeat the move with the opposite arm and leg.
Perform the exercise 10 times for each side.
Multifidus Activation
The multifidus muscles are small muscles close to your spine that assist with twisting and bending motions. As many people with spondylolisthesis have weak multifidus muscles, this exercise helps strengthen them.
Step 1: Lying on your side, use your free hand to find the groove in your back next to your spine.
Step 2: Activate your core by imagining that you’re moving your chest (don’t actually move your leg). You should feel the multifidus muscles bulge under your fingers.
Step 3: Hold the pose for 3 seconds and relax.
Repeat the exercise 10 times. Then lie on your other side and repeat the exercise another 10 times.
Gluteal Stretch
Stretching your glute muscles can help to relieve tightness and tension. It can also lessen lower back pain, including pain caused by spondylolisthesis.
Step 1: Start by laying on your back with your knees bent.
Step 2: Rest one ankle over the other leg, just above the knee.
Step 3: Grab the thigh of the bottom leg and pull it toward your chest until you feel the stretch in your buttocks. It should not be painful.
Step 4: Hold your leg for 15 to 30 seconds and release it.
Repeat the exercise 3 times for each leg.
Diagnosis of Lumbar Spondylosis
To diagnose spinal osteoarthritis, a doctor will need to conduct a physical and neurological examination – and look closely at a patient’s spine and range of motion when bending forward, backward, and side-to-side. The doctor will note the shape of the spine, including any abnormal curvatures, and will palpate or feel the spine to detect any tender spots, muscle tightness, spasms, bumps, or areas of inflammation.
Your doctor will evaluate your pain level, along with other symptoms such as weakness or paresthesias, and take X-rays to detect bone spurs or loss of disc height, which can be a sign of degenerative disc disease. Your doctor may also order a CT (computerized tomography) or MRI (magnetic resonance imaging) to view degenerative changes and abnormalities in the spine’s soft tissues. Depending on your symptoms, you may undergo other diagnostic tests.
These are tests that produce various kinds of pictures of your body. Such tests include:
- X-rays: They can help measure the extent of arthritis or injuries to the bones
- MRI: This test checks your spinal nerves and looks for disc problems
- CT scan: This test checks your spinal canal, bones, and joints
Treatment of Lumbar Spondylosis
Treatment depends on the grade of the slippage, your symptoms, age and overall health. Your doctor will discuss treatment options with you. You may need medication, physical therapy or surgery.
Nonsurgical treatments include:
- Rest: Take a break from strenuous activities and sports
- Medication: An over-the-counter nonsteroidal anti-inflammatory drug (NSAID), such as ibuprofen or naproxen can bring relief. If those don’t work, your doctor may prescribe other medications
- Injections: You receive an injection of steroid medications directly into the affected area
- Physical therapy: A physical therapist can teach you targeted exercises to strengthen your abdomen (belly) and back. Daily exercises often relieve pain after a few weeks
- Bracing: A brace can help stabilize your spine. The brace limits movement so that fractures can heal. Braces are not used in adults
You may need surgery if you have high-grade spondylosis, the pain is severe or you’ve tried nonsurgical treatments without success. The goals of spondylosis surgery are to:
- Relieve pain from the irritated nerve
- Stabilize the spine where the vertebra has slipped
- Restore your function
Surgery for back pain due to spondylosis typically involves spinal decompression, with or without fusion. Decompression alone is almost never done in isthmic spondylosis. Studies show fusion with decompression may give better outcomes than decompression alone. During a decompression surgery, your surgeon removes bone and disk from the spine. This procedure gives the nerves space inside the spinal canal, relieving pain.
For a fusion surgery, your surgeon fuses (connects) the two affected vertebrae. As they heal, they form into one bone, eliminating movement between the two vertebrae. You may experience some limited spinal flexibility as a result of the surgery.
Most of the time, pain is gone after you recover from spondylolisthesis surgery. You can gradually begin to resume your activities until you are back to full function and movement.
How to brace your Lumbar Spondylosis?
Depending on how spondylosis affects the parts of your spine, it may cause spinal instability. That means that the parts of your spine aren’t working properly to control your movements. With an unstable spine, you’re more at risk for neurological injury (injury to the nerves). To address this instability, your doctor may recommend you wear a brace for a while.
Bracing is a temporary treatment option for spondylosis, one more often used for spondylosis in the neck (cervical spine). Braces can, however, also be used for spondylosis in other regions of the spine, such as the low back (lumbar spine). A brace will help control your pain by limiting motion. Braces also help support your spine, taking some of the pressure off your vertebrae. Additionally, braces can help the muscles relax, and that relaxation alone can provide a level of pain relief.
Long-term bracing isn’t usually recommended because it can cause the spinal muscles to weaken. It’s better for you to go to physical therapy to learn how to strengthen your muscles so that they better support your spine.
Your doctor will decide if bracing is a good option for you, what kind of brace you should wear, and how long you’ll need to wear it. With a brace, it’s absolutely critical that you follow the doctor’s order exactly for how and when you’re supposed to wear it. If you don’t, the brace won’t be as effective at relieving your pain and providing support.