Rheumatoid Arthritis : Cause, Symptoms, Diagnosis, Treatment, Exercise
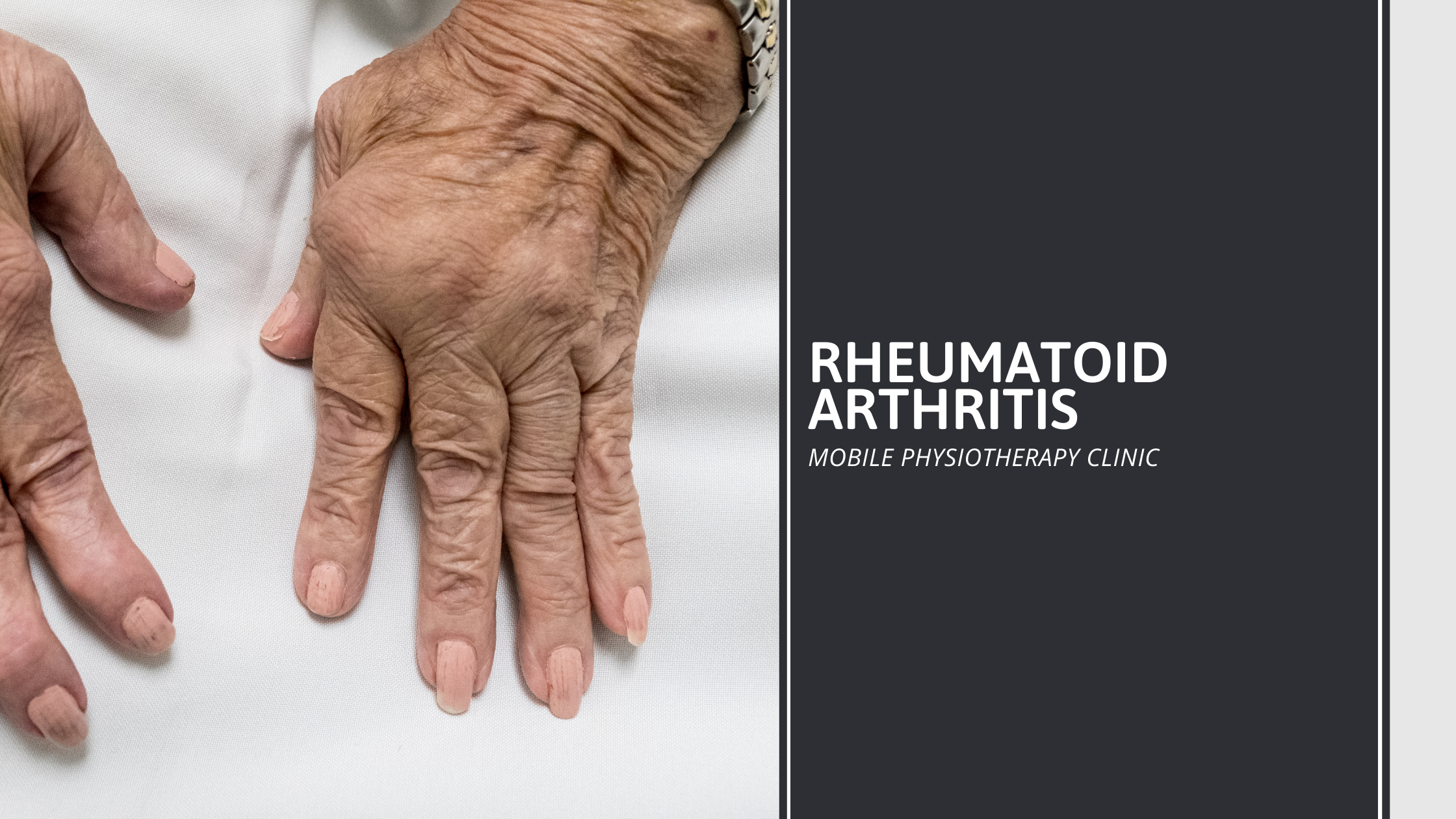
Rheumatoid Arthritis is a general term for inflammation (redness, warmth, swelling, and pain) in joints. Rheumatoid arthritis is a type of chronic (ongoing) arthritis that occurs in joints on both sides of the body (for instance, both hands, wrists, and/or knees), which helps distinguish it from other types of arthritis.
In addition to affecting the joints, rheumatoid arthritis may occasionally affect other parts of the body, including the skin, eyes, lungs, heart, blood, nerves, or kidneys.
Rheumatoid arthritis is an autoimmune disease, meaning that the patient’s immune system (the body’s infection-fighting system) is overreacting against itself. The result can cause some or all of the symptoms of rheumatoid arthritis.
Rheumatoid arthritis affects more than 1.3 million people in the United States. It is 2.5 times more common in women than in men. It usually occurs in people who are between the ages of 20 and 50; however, young children and the elderly can also develop rheumatoid arthritis.
Table of Contents
Symptoms of Rheumatoid Arthritis
Rheumatoid arthritis is a chronic disease marked by symptoms of inflammation and pain in the joints. These symptoms and signs increase during periods known as flares or exacerbations. Other times are known as periods of remission, this is when symptoms can disappear completely.
Rheumatoid arthritis symptoms commonly affect joints in the hands, wrists, and knee joint, but can also affect tissues and organs throughout the body including the lungs, heart, and eyes.
Symptoms can include:
- pain or aching in more than one joint
- stiffness in more than one joint
- tenderness and swelling in more than one joint
- the same joint symptoms on both sides of the body
- loss of joint function and deformities
- fatigue
- low-grade fever
- loss of appetite
- weakness
Symptoms can vary from mild to severe. It’s important not to ignore your symptoms, even if they come and go. Knowing the early signs of Rheumatoid arthritis will help you and your healthcare provider better treat and manage it.
Causes of Rheumatoid Arthritis
The exact cause of rheumatoid arthritis is unknown. However, it is believed to be caused by a combination the following factors:
- Genetics (heredity)
- Abnormal immunity
- The environment
- Hormones
Normally, the immune system protects the body from disease. In people who have rheumatoid arthritis, something possibly infections, cigarette smoking, and physical or emotional stress, among other causes—triggers the immune system to attack the joints (and sometimes other organs).
Gender, heredity, and genes largely determine a person’s risk of developing rheumatoid arthritis. For example, women are about three times more likely than men to develop rheumatoid arthritis.
Risk Factors of Rheumatoid Arthritis
- Age: The onset of rheumatoid arthritis is highest among adults in their 50s. Risk continues to increase with age for people assigned male at birth. Rheumatoid arthritis often occurs in people assigned female at birth during their child-bearing years
- Sex: People assigned female at birth are two to three times more likely to develop rheumatoid arthritis than people assigned male at birth
- Genetics: People born with certain genes, called HLA class II genotypes, are more likely to develop rheumatoid arthritis. The risk of rheumatoid arthritis may be highest when people with these genes have obesity or are exposed to environmental factors like smoking
- History of live births: People with ovaries who have never given birth may be at a greater risk of developing rheumatoid arthritis than those who have given birth
- Early life exposure: According to the Centers for Disease Control and Prevention, children whose mothers smoked have double the risk of developing rheumatoid arthritis as adults
- Smoking: Studies show that people who smoke cigarettes are at an increased risk of developing rheumatoid arthritis
- Obesity: Having obesity can increase the risk of developing rheumatoid arthritis
- Diet: High consumption of sodium, sugar (especially fructose), red meat, and iron is associated with an increased risk of developing rheumatoid arthritis
Complications
Rheumatoid arthritis increases your risk of developing:
- Osteoporosis: Rheumatoid arthritis itself, along with some medications used for treating rheumatoid arthritis, can increase your risk of osteoporosis which is a condition that weakens your bones and makes them more prone to fracture
- Rheumatoid nodules: These firm bumps of tissue most commonly form around pressure points, such as the elbows. However, these nodules can form anywhere in the body, including the heart and lungs
- Dry eyes and mouth: People who have rheumatoid arthritis are much more likely to develop Sjogren’s syndrome, a disorder that decreases the amount of moisture in the eyes and mouth
- Infections: Rheumatoid arthritis itself and many of the medications used to combat it can impair the immune system, leading to increased infections. Protect yourself with vaccinations to prevent diseases such as influenza, pneumonia, shingles and COVID-19
- Abnormal body composition: The proportion of fat to lean mass is often higher in people who have rheumatoid arthritis, even in those who have a normal body mass index (BMI)
- Carpal tunnel syndrome: If rheumatoid arthritis affects your wrists, the inflammation can compress the nerve that serves most of your hand and fingers
- Heart problems: Rheumatoid arthritis can increase your risk of hardened and blocked arteries, as well as inflammation of the sac that encloses your heart
- Lung disease: People with rheumatoid arthritis have an increased risk of inflammation and scarring of the lung tissues, which can lead to progressive shortness of breath
- Lymphoma: Rheumatoid arthritis increases the risk of lymphoma, a group of blood cancers that develop in the lymph system
Preventions
There’s no way to prevent Rheumatoid arthritis, but you can lower your chances if you:
- Quit smoking: It’s the one sure thing besides your genes that boosts your odds of getting Rheumatoid arthritis. Some studies show it also can make the disease get worse faster and lead to more joint damage, especially if you’re ages 55 or younger. If you’re overweight and a smoker, your chances of developing Rheumatoid arthritis go up
- Take care of your gums: New research shows a link between Rheumatoid arthritis and periodontal (gum) disease. Brush, floss, and see your dentist for regular checkups
Even though there’s nothing you can do to ensure you won’t get it, keep in mind that early treatment can make your symptoms less painful and save your joints from damage. Ideally, you should begin treatment within 3 to 6 months of your first symptoms.
Diagnosis
Diagnosing Rheumatoid arthritis can take time and may require multiple lab tests to confirm clinical examination findings. Your doctor will use several tools to diagnose Rheumatoid arthritis.
First, they’ll ask about your symptoms and medical history. They’ll also perform a physical exam of your joints. This will include:
- looking for swelling and redness
- examining joint function and range of motion
- touching the affected joints to check for warmth and tenderness
- examining for skin nodules
- testing your reflexes and muscle strength
If they suspect Rheumatoid arthritis, they’ll most likely refer you to a specialist called a rheumatologist.
Since no single test can confirm a diagnosis of Rheumatoid arthritis, your doctor or rheumatologist may use several different types of tests.
They may test your blood for certain substances like antibodies, or check the level of certain substances like acute phase reactants that are elevated during inflammatory conditions. These can be a sign of Rheumatoid arthritis and help support the diagnosis.
They may also request certain imaging tests, such as an ultrasound, X-ray, or MRI.
Tests not only show if joint damage has occurred but also how severe the damage is.
A complete evaluation and monitoring of other organ systems might be recommended for some people with Rheumatoid arthritis, too.
There are several types of blood tests that help your doctor or rheumatologist determine whether you have Rheumatoid arthritis. These tests include:
- Rheumatoid arthritis: The RF blood test checks for a protein called rheumatoid factor. High levels of rheumatoid factors are associated with autoimmune diseases, especially Rheumatoid arthritis
- Anti Citrullinated peptide antibody test (anti-CCP): This test looks for an antibody that’s associated with Rheumatoid arthritis. People who have this antibody usually have the disease. However, not everyone with Rheumatoid arthritis tests positive for this antibody. The anti-CCP test is more specific for Rheumatoid arthritis than the RF blood test, and often is positive before the RF test
- Antinuclear antibody test: The antinuclear antibody panel (ANA) tests your immune system to see if it’s producing antibodies to the nucleus of cells. Your body often makes ANA antibodies as a response to many different types of autoimmune conditions, including Rheumatoid arthritis
- Erythrocyte sedimentation rate: The ESR test helps determine the degree of inflammation in your body. The result tells your doctor whether inflammation is present. However, it doesn’t indicate the cause or site of the inflammation
- C-reactive protein test: A severe infection or significant inflammation anywhere in your body can trigger your liver to make C-reactive protein. High levels of this inflammatory marker are associated with Rheumatoid arthritis
Treatment of Rheumatoid Arthritis
The goals of rheumatoid arthritis treatment are to:
- Control a patient’s signs and symptoms
- Prevent joint damage
- Maintain the patient’s quality of life and ability to function
Joint damage generally occurs within the first two years of diagnosis, so it is important to diagnose and treat rheumatoid arthritis in the “window of opportunity” to prevent long-term consequences.
Treatments for rheumatoid arthritis include medications, rest, exercise, physical therapy/occupational therapy, and surgery to correct damage to the joint.
The type of treatment will depend on several factors, including the person’s age, overall health, medical history, and the severity of the arthritis.
Non-pharmacologic therapies
It is the first step in treatment for all people who have rheumatoid arthritis. Non-pharmacologic therapies include the following:
Rest: When joints are inflamed, the risk of injury to the joint and to nearby soft tissue structures (such as tendons and ligaments) is high. This is why inflamed joints should be rested. However, physical fitness should be maintained as much as possible. Maintaining a good range of motion in your joints and good fitness overall are important in coping with the overall features of the disease.
Exercise: Pain and stiffness often prompt people with rheumatoid arthritis to become inactive. However, inactivity can lead to a loss of joint motion, contractions, and a loss of muscle strength. These, in turn, decrease joint stability and increase fatigue.
Regular exercise, especially in a controlled fashion with the help of physical therapists and occupational therapists, can help prevent and reverse these effects. Beneficial workouts include: range-of-motion exercises to preserve and restore joint motion; exercises to increase strength, and; exercises to increase endurance (walking, swimming, and cycling).
Physical and occupational therapy: Physical and occupational therapy can relieve pain, reduce inflammation, and help preserve joint structure and function for patients with rheumatoid arthritis.
Specific types of therapy are used to address specific problems of rheumatoid arthritis:
- The application of heat or cold can relieve pain or stiffness
- Ultrasound can help reduce inflammation of the sheaths surrounding tendons (tenosynovitis)
- Exercises can improve and maintain range of motion of the joints
- Rest and splinting can help reduce joint pain and improve joint function
- Finger-splinting and other assistive devices can prevent deformities and improve hand function
- Relaxation techniques can relieve secondary muscle spasm
Occupational therapists also focus on helping people with rheumatoid arthritis continue to actively participate in work and recreational activity, with special attention to maintaining good function of the hands and arms.
Nutrition and dietary therapy: Weight loss may be recommended for overweight and obese people to reduce stress on inflamed joints.
People with rheumatoid arthritis have a higher risk of developing coronary artery disease. High blood cholesterol (a risk factor for coronary artery disease) can respond to changes in diet. A nutritionist can recommend specific foods to eat or avoid in order to reach a desirable cholesterol level.
Changes in diet have been investigated as treatments for rheumatoid arthritis, but no diet has been proven to cure it. No herbal or nutritional supplements, such as cartilage or collagen, can cure rheumatoid arthritis. These treatments can be dangerous and are not usually recommended.
Medications
There are many medications to decrease joint pain, swelling, and inflammation, and prevent or slow down the disease. The type of drugs that your doctor recommends will depend on how severe your arthritis is and how well you respond to the medications.
These medications include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, or naproxen
- Corticosteroids (oral and injectable forms)
- COX-2 inhibitor (celecoxib [Celebrex])
- Disease-modifying anti-rheumatic drugs (DMARDs) such as hydroxychloroquine (Plaquenil), methotrexate (Rheumatrex, Trexall), sulfasalazine (Azulfidine), and leflunomide (Arava)
It may take four to six weeks of treatment with methotrexate, one to two months with sulfasalazine, and two to three months with hydroxychloroquine to see an improvement in symptoms.
- Biologic agents, such as infliximab (Remicade), etanercept (Enbrel), adalimumab (Humira), certolizumab (Cimzia), golimumab (Simponi), tocilizumab (Actemra), rituximab (Rituxan), abatacept (Orencia), anakinra (Kineret), tofacitinib (Xeljanz)
Biologics tend to work rapidly, within two weeks for some medications and within four to six weeks for others. Biologics should be alone or in combination with other DMARDs. They are reserved for patients who do not adequately respond to DMARDs, or if the prognosis (outlook) for the patient is problematic.
Other precautions to note with these drugs:
- DMARDs and biologic agents interfere with the immune system’s ability to fight infection and should not be use by people who have serious infections
- Anti-TNF agents such as infliximab, etanercept, adalimumab, certolizumab and golimumab are not recommend for people who have lymphoma or who have been treat for lymphoma. People with rheumatoid arthritis especially those with severe disease have an increase risk of lymphoma, regardless of what treatment is use. Anti-TNF agents have been associate with a further increase in the risk of lymphoma in some studies but not others. More research is in need to define this risk
- Testing for tuberculosis (TB) is need before starting anti-TNF therapy. People who have evidence of earlier TB infection should be treat for TB, because there is an increased risk of developing active TB while receiving anti-TNF therapy
Some of these medications are traditionally use to treat other conditions, such as cancer, inflammatory bowel disease and malaria. When these drugs are use to treat rheumatoid arthritis, the doses are much lower and the risks of side effects tend to be considerably less. However, the risk of side effects from treatment must be weigh against the benefits on an individual basis.
When you are prescribe any medication, it is important to meet with your physician regularly so he or she can watch for any side effects.
Surgery
When bone damage from the arthritis has become severe or pain is not controlled with medications, surgery is an option to restore function to a damaged joint.
Exercises for Rheumatoid Arthritis
The following types of exercise may help relieve the pain, joint stiffness, and other symptoms that rheumatoid arthritis can cause:
1. Stretching
It can help improve flexibility, reduce stiffness, and increase range of motion. Stretching daily is important for relieving rheumatoid arthritis symptoms.
The ideal stretching routine will be different for each person and depend on which joints are affected and what symptoms occur. However, stretches often involve slowly and gently moving the joints of the knees, hands, and elbows.
A typical stretching routine may consist of:
- warming up by walking in place or pumping the arms while sitting or standing for 3–5 minutes
- holding each stretch for 20–30 seconds before releasing it
- repeating each stretch 2–3 times. Using a yoga strap may help people maintain proper form while stretching. If someone does not have a yoga strap, they could use an alternative such as a dog leash
Some people may find it beneficial to work with a physical therapist who understands rheumatoid arthritis to learn the correct way to perform the stretches that meet their personal needs.
2. Walking
Walking is a low-impact form of exercise that can help with aerobic conditioning, heart and joint health, and mood.
It is essential to wear proper shoes and stay hydrated, even if the walking is not strenuous. It is often sensible to walk slowly initially and then increase the pace when possible.
A person may want to start a walking routine on flat, even surfaces before progressing to uphill, downhill, or uneven surfaces.
3. Flowing movements, such as tai chi and yoga
Both tai chi and yoga combine deep breathing, flowing movements, gentle poses, and meditation. They increase flexibility, balance, and range of motion while also reducing stress.
A 2013 study of participants with rheumatoid arthritis who had done group tai chi suggested that tai chi could reduce anxiety and depression while increasing self-motivation and self-esteem.
The participants did tai chi twice a week for 12 weeks.
A 2013 study of women with rheumatoid arthritis who did Iyengar yoga suggests that this exercise had mood, fatigue, and pain disability benefits. The participants did yoga twice a week for six weeks.
It is possible to find free online videos or apps like Gaia for tai chi or yoga workouts, including some yoga workouts specifically for people with rheumatoid arthritis. A person should always talk to their doctor before starting a yoga or tai chi practice.
4. Pilates
Pilates is a low-impact activity that can increase flexibility for enhanced joint health.
It can be helpful to do Pilates poses that activate the core muscles and emphasize movements that help with stability. Pilates can be good for overall movement patterns, similar to tai chi and yoga.
People new to Pilates should begin slowly and seek guidance from a certified trainer if possible.
5. Water exercises
Water helps support body weight by minimizing gravity, which means that water exercises do not impact heavily on the joints.
Swimming, water aerobics, and other gentle water exercises can increase flexibility, range of motion, strength, and aerobic conditioning. They can also reduce joint stress and stiffness.
More studies on the benefits of water exercises on rheumatoid arthritis are needed.
6. Cycling
As rheumatoid arthritis increases the risk of cardiovascular disease, it is vital to keep the heart as healthy as possible. Cycling can help improve cardiovascular function.
Riding a stationary bike can be a safe way to get the joints moving and improve cardiovascular fitness. A benefit of a stationary bike is that a person can be supervised while riding. A person can also ride their bike outdoors to get fresh air.
In addition to improving aerobic conditioning, cycling can reduce stiffness, increase range of motion and leg strength, and build endurance.
7. Strength training
Strengthening the muscles around the affected joints can help increase strength while reducing pain and other rheumatoid arthritis symptoms.
Using a resistance band is a way to challenge the body and build muscle over time. A physical therapist who works with people with rheumatoid arthritis should be able to offer guidance on suitable exercises.
8. Hand exercises
Rheumatoid arthritis can sometimes lead to limited use of the hands. A person with rheumatoid arthritis may lose their grip strength or find that they are dropping things.
Bending the wrists up and down, slowly curling the fingers, spreading the fingers wide on a table, and squeezing a stress ball can all help increase strength and flexibility in the hands.
9. Gardening
Light gardening can be a beneficial exercise for a person with rheumatoid arthritis.
People should be gentle with their body, work slowly, and avoid overstraining the muscles and joints.
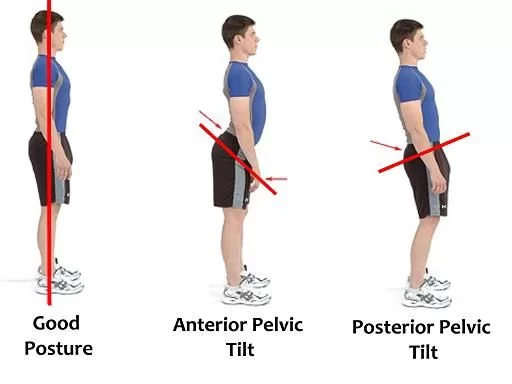
A person can avoid overstraining by avoiding bending and twisting in ways that can aggravate the lower back. A gardener should make sure to properly hinge at the hips when working in the garden.






12 Comments