Spasticity and Physiotherapy Treatment:-
Table of Contents
What is a Spasticity?
Spasticity is a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes with exaggerated tendon reflexes, resulting from hyper excitability of the stretch , as one factor of the upper motor neuron syndrome.
Spasticity is loss in muscle movement patterns so that muscles contract all at once. Muscle movements are usually controlled by a complex neuron muscular system that allows some muscles to contract (tighten) while others to relax.
Injury to nerves in the central nervous system can disrupt the pattern. As a result, many muscles may start contracting all at once. Spasticity can be found in cerebral palsy patients, traumatic brain injury subjects, stroke, spinal cord injury, multiple sclerosis, and other conditions that affect the brain or spinal cord. Spasticity mostly affects in the lower limbs but can occur in the upper limbs too.
Spasticity is expected to be a positive feature of upper motor neuron syndrome that indicates injury . This is because there is due to a loss of inhibition of the lower motor neuron tracts, rather than a disruption of connection to the lower motor neuron . This comes from disordered sensorimotor control of motion a lesion of the upper motor neuron which regulate muscle control. Therefore, there is an imbalance of the signals between the central nervous system (CNS) and muscles, presenting as intermittent or sustained involuntary activation of muscles spindle.
All muscles have some tone to maintain functional movements, for example, activation of anti gravity muscles to maintain particular postures like sitting or standing . In patient with spasticity, there is a velocity-dependent increase in muscle tone to passive movement or stretch. This creates an inability to stretch muscles or coordinate movements efficiently.
Causes of Spasticity
- Cerebral Palsy
- Multiple Sclerosis
- Motor neuron disease
- Stroke
- Hypoxic Brain Injury
- Traumatic Brain Injury
- Parkinson’s Disease
- Spinal cord injury
- Spinal cord compression
- Metastasis / tumor
This inhibition can result from central nervous system pathology, such as Lesions to the central nervous system (brain or spinal cord) can lead to both positive and negative upper motor neuron syndrome features:
| Positive Component | Negative Component |
| Exaggerated Reflexes | Spastic muscle Contractions |
| Released Reflexes | Motor Weakness |
| Babinski Sign positive | Slowed voluntary motion |
| Increased passive Tone | Loss in Dexterity |
| Clonus | Loss of Selective Motor Control |
Spasticity can have an affection on an individual’s function, affecting upper and lower limbs, as well as trunk. If this can not be managed effectively, it can lead to fixed deformity contractures(changes to soft tissue), which affect skin care, comfort and hygiene care, as well as complications for daily tasks.
The management of spasticity needs to be carefully considered as some patients rely on aspects of spasticity to allow them to maintain enough tone for functions such as standing or walking. Physiotherapy management may include facilitating individuals to utilize this to maintain weight bearing and ambulation to decrease their risk of developing osteoporosis, strengthen muscles, help improve circulation and promote overall mental health.
Classification of Spasticity:
Intrinsic Tonic Spasticity: Exaggeration(excessive) of the tonic component of the stretch reflex (manifesting as increased tone).
Intrinsic Phasic Spasticity: Exaggeration (excessive) of the phasic aspect of the stretch reflex ,manifesting as tendon hyper-reflexia and clonus.
Extrinsic Spasticity: Exaggeration(excessive) of extrinsic flexion or extension spinal movements and reflexes .
Spasticity usually have an impact on an patient’s function, affecting upper extremity and lower extremity, as well as the torso. If this is not treated time effectively , it can result in to fixed deformity contractures(hardening of soft tissue), which affect skin and causes blemishes, comfort and hygiene, moreover complications for daily tasks.
Prevalence:
35% of patients are with stroke,more than 90% subjects with CP,about 50% of TBI patients40% of SCI patients between 37%and 78% of MS patients.Anatomy and Etiology UMN injury results in to loss of inhibition downstream and hypersensitivity of the reflex arc inside the spinal cord. Primary affections from an upper motor neuron lesion (UMNL) are usually due to the disruption of supra spinal control of descending pathways that has control on excitatory and inhibitory reflex on proprioceptive, cutaneous and nociceptive spinal reflexes.
Different Lesions and Their Presentations:-
The signs and symptoms between Cortical UMN Lesions and Spinal Cord UMN Lesions vary with the location of where the damage has taken place.
Corticospinal Tract Lesion
Whereas the Corticospinal Tract has an inhibitory effect on stretch and flexor reflex, the lead inhibitory system produced by the Dorsal Reticulospinal Tract remains intact and thus the balance of excitatory and inhibitory influences are maintained equally.
Internal Capsule Lesion
This type of lesion leads to interruption of both the Corticospinal Tract and Corticoreticular Tract pathways which are supposed for the inhibitory reflexes and some loss of inhibition to stretch and flexor stretches. The excitatory systems from both the Medial Reticulospinal tract and Vestibulospinal Tract are usually more dominant which leads to the facilitation of extensor muscles and stretch reflexes although it causes inhibition of flexors stretch.
Incomplete Spinal Cord Lesion
Signs and symptoms will vary depending on site of injury and extent of damage. If the inhibitory system is influenced then there might be an unopposed excitatory drive to stretch and extensor reflexes with partial inhibition of flexor reflexes.
Complete Spinal Cord Lesion
Spinal reflexes are unopposed due to the complete loss of supra spinal dominance. Both flexor and extensor reflexes are diminished and therefore people may experience both flexor and extensor spasms.
Clinical presentation of Spasticity:
Increased muscle tone in agonist muscle groups such as the shoulder adductors, flexors of elbow, wrist, and finger and forearm pronators. In the lower extremity, the increased tone is specifically prominent in the hip adductors, knee flexors and extensors, and plantar flexors and invertors muscle group of the ankle. Muscles those move Anti gravity are predominantly affected.Individuals may report difficulty with footwear if their spasticity involves constant.
Permanent loss of joint range of motion has been known to happen 3-6 weeks after stroke or brain injury and therefore it is imperative that spasticity is diagnosed early on in the assessment in order for it to be monitored and managed as per requirement. In a person with hemiplegia the lower extremity pattern is plantar flexion and inversion of the ankle with hamstring tightness reduced knee range of motion as well as adductor spasticity. Upper limb presentation is usually shoulder girdle movement as adduction, internal rotation, elbow flexion, forearm pronation with wrist and elbow flexion.
Ashworth scale of Spasticity
The Ashworth scale is the most broadly used assessment tool to measure resistance to limb movement in a clinic and hospital setting, although it is unable to distinguish between the neural and non-neural components of elevated tone.
The scale is as follows:
| Grade | Description |
| 0 | Not increase in muscle tone or length |
| 1 | Slight increase in tone giving a hold when the limb is mobiled |
| 2 | More noticable increase in tone but limb easily moves |
| 3 | Considerable increase in tone – passive movement difficult |
| 4 | Limb is rigid in flexion or extension unable to move |
Modified Ashworth scale of Spasticity
| Grade | Description |
| 0 | No increase in muscular tone |
| 1 | Slight increase in muscular tone, manifested by either catch and release or by minimal resistance at the last range of motion when the affected limb is moved in flexion or extension |
| 1+ | Minimal increase in muscular tone, manifested by a catch afterwards followed by minimal resistance throughout the remainder (less than half) of the ROM |
| 2 | More marked increase in muscle tone through most of the ROM, but affected part(s) easily moved |
| 3 | Considerable increase in muscle tone, passive movement difficult |
| 4 | Affected limb rigid in flexion or extension |
Treatment of Spasticity
Medication of Spasticity
Baclofen:
The most usual systemic agent. Baclofen effects on the receptors of excitatory nerve terminals, in particular the ‘GABA B G-Protein receptor. If the drug has attached to this G-Protein on the pre-synaptic terminal, potassium channels open while calcium channels close, hyperpolarising the cellular activity. The inabiulity for the calcium to enter the cell membrane means the release of glutamate, an excitatory neurotransmitter, is prohibited.
Tizanidine repeats the same mechanism as Baclofen, but attaches to the a2 adrenoreceptor on the pre-synaptic cell membrane.
Botulinum Toxin (Botox) Injected locally into muscle belly. Prevents the excytotic release of acetylcholine neuron transmitter at the level of the neuromuscular junction which further prevents release of calcium from the sarcoplasmic reticulum which leads to excitation-contraction coupling.
Diazepam (Valium) Less common used. Prioritizes the effect of GABA, an inhibitory neurotransmitter, that is released from inhibitory inter neurons which reduces the excitability in the post-synaptic nerve terminal.
Dantrolene Given orally. Blocks the release of calcium from the sarcoplasmic reticulum within the muscle which prevents excitation-contraction coupling.
Advantages include:-
- Oral medications is used to relax a huge number of muscles.
- The dosage of oral medications is easily adjusted and changed.
- Oral medications may be discontinued at any time.
Disadvantages include:–
- The effect of oral medications may be indigestible and cause gastric problem.
- Drowsiness is a significant side effect. Dizziness and weakness may take place.
- Some medications can lead to liver inflammation.
Physiotherapy treatment of Spasticity:
Spasticity is one of the commonest components of the UMN syndrome although should not be considered in isolation when it comes to management protocols. It is essential that management targets particular impairments to treat and patient is always focused rather than aimed at reducing the degree of spasticity Planned interventions should consider a balance between movement and positioning.
Standing
Tilt table or standing frame -The compensatory effects of standing on whole feet, using either a tilt table or a standing frame are said to be secondary to the activating the anti-gravity muscle activity in the trunk and lower extremities, maintenance or improvement in soft tissue and joint flexibility, modulation of the neural component of spasticity with through out prolonged stretch and altered sensory input, reduction of lower limb spasms, and positive psychological counseling.
Progressive resistance exercise (PRE)
There is proved evidence that strength training can improve arm’s strength and function without increasing tone or pain in individuals with stroke, and also elevate motor relearning in a paralytic limb . The effect of strength training usually relies on the duration after stroke, usually the mechanism underlying loosing strength changes over the time.
Immediately following a stroke, reduced force production is due to a loss of descending input to the spinal neuron motor tract, declining the activation of motor units, sometimes six months after stroke, reduction in force production is also because of decrease in the cross sectional area of muscle spindle and a reduction of motor units due to improper use.
Aerobic exercise
Aerobic exercise is physical activity which aims to improve the oxygen supply system by increasing muscle strength and endurance as well as straining the heart and lung. It has also been noticed to improve active range of motion available after stroke, possibly by increasing motor relearning .
Bobath therapy approach
Neuro-developmental treatment Bobath approach explains motor dysfunction in hemiplegia through a neuron physiological perspective, stating that the individual must be actively participating while the therapist assists the patient to mobilize using key points of control and reflex inhibiting techniques .Suggested that different mechanisms are involved in creating the non-linear pattern of neurological management after stroke.
These mechanisms include:
- preservation of penumbral cells surrounding the infarcted part
- elevation of cerebral shock and
- the urgency of the brain to adapt by neuroplasticity.
Neuromuscular electrical stimulation (NMES)
Neuromuscular electrical stimulation (NMES) refers to the stimulate the intact lower motor neuron to activate paralytic muscle or group of muscles. Functional electrical stimulation (FES) is a commonly used neuromuscular electrical stimulation. As FES produces functional movement, it has been hypothesized that the FES-induced afferent–efferent stimulation that results in limb movements in addition to cutaneous and proprioceptive inputs during the acute stage could play a major role in ‘reminding’ patients how to perform movements properly.
An increase in synaptic efficacy in existing neural circuits, or the formation of upcoming synapses, may be involved in the earlier stages of motor learning program. In addition, rapidly repeated movements of the affected extremity in stroke patients, produced by FES, might reinforce network connection patterns between synapse and muscle. Thus FES facilitates motor cortical rearrangements towards skill possession.
Mechanical gait trainer (treadmill training)
The mechanical gait trainer, uses an overhead suspension and harness belt to support a percentage of the individual’s body weight as the they walk on a treadmill. This device stimulates the phases of gait, supports the patients according to their motor power, and controls the center of gravity (COG) in the vertical and horizontal directions. It has been observed to reduce spasticity by allowing early training of posture and stepping reflex in cp patients. It promotes motor relearning of gait cycles.
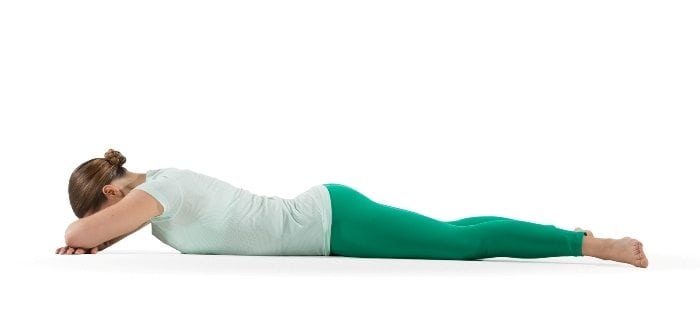
Passive movement and stretching
Passive movement and passive stretching of the joints aim of stretch interventions is to maintain and increase joint mobility by influencing the extensibility of the soft tissues surround the joints . Stretch interventions is usually applied by therapist but also can be self stretched. All techniques involve the therapeutically elongation of soft tissues for varying duration of time.
Some techniques are only applied for short periods of time. Other passive techniques, such as positioning, provide a way of administering stretches for sustained long periods of time. Splints and serial casts are used to give stretch for even longer periods of time and are sometimes used to provide uninterrupted prolonged stretch for many days or even weeks with the help of weight.
Static positioning
Usually Muscle length positioning refers to the changes of a muscles’ length and reduce in tone on stretch reflex activity. Although spasticity is said to be length-dependent, the position of patients during test is likely to influence the outcomes of the spasticity assessment, particularly when bi-articular muscles are indulged.
This is possibly due to changes in intrinsic muscle characteristics, some prolonged state shows more stretch reflex activity compared with a muscle in a tightened state.This factor is taken into account when assessing and managing spasticity with different interventions.
Continuous passive motion robotics
The use of robotics to give continuous passive motion and stretch to joints has been successful in reducing spasticity in the upper limb by influencing mechanical factors in the soft tissues and by sending elevation of afferent nerve stimulation to the motor cortex leading to motor re-learning.
Reflex inhibitory thermoplastic splinting and orthotics
Wrist splints are used to prevent as well as to reduce contracture also the aim of splinting is to influence muscle extensibility, according to the mode of stretch given by the splint. Both static and dynamic passive movements and stretching of joints affected by spasticity have been observed to have an effect on decreasing motor neuron excitability, gaining flexibility, and compromising tensile stress on the soft tissues.
Therefore a combination of reflexive and mechanical factors shows result in decreased spasticity. It can be stated that the motion and stretch in a weight bearing or non-weight bearing position are more beneficial towards declination of spasticity .
Surgical treatments:
Intrathecal baclofen therapy (ITB): ITB therapy is used to cure severe spasticity. Baclofen is injected directly to the spinal cord by a programmable pump and with use of catheter. Because the drug is placed directly at the site of action in the spinal column, much less amount of baclofen is needed, and there are less side effects than if the drug were taken orally. Individuals must undergo an ITB screening test prior to having a shunt placed.






One Comment