Stroke
Table of Contents
What is a Stroke?
A stroke is a medical condition in which blood flow to the brain reduces or stop which leads to brain cell death or loss of function of brain cell.
There are mainly 2 types of stroke:
- ischemic, due to lack of blood flow
- hemorrhagic, due to bleeding.
Both types lead parts of the brain cell to stop working properly.
- In a Stroke, there is an inability to move the body or loss of sense of one side of the body.
- Difficulty understanding or talking vertigo, or reduced vision to one side.
If symptoms last < 1 or 2 hours, the stroke is a transient ischemic attack (TIA), also called a mini-stroke.
- A hemorrhagic stroke may also be associated with a severe head pain
- The symptoms of a stroke may be temporary and /or permanent.
- Long-time complications may include pneumonia & loss of bladder control.
- The main risk factor for stroke is mainly High blood pressure.
- Other risk factors include
- High blood cholesterol
- tobacco smoking
- obesity
- diabetes mellitus
- A previous TIA
- End-stage renal disease
- atrial fibrillation.
- Ischemic stroke causes are Obstruction of a blood vessel, although there are also some common causes.
- Hemorrhagic stroke causes mainly – If bleeding directly into the brain and into the gap between the brain’s membranes. Bleeding can occur due to a ruptured cerebellum aneurysm.
- To diagnose stroke, A physical exam is supported by medical imaging such as a CT or MRI scan.
- A CT scan may rule out bleeding, but can not necessarily rule out ischemia, doesn’t see on a CT scan.
- Others like (ECG) and blood tests are done to determine risk factors and rule out other possible causes.
- Low blood sugar can leads to similar symptoms.
To prevent stroke:
- Decreasing risk factors, surgery to open arteries to the brain which is problematic carotid shallow, and warfarin in public with atrial fibrillation.
- Aspirin can be recommended by physicians for prevention.
- A stroke or TIA is often requires emergency treatment.
- An ischemic stroke, if detected within three to four 4 & a half hours and may be treatable with a medication that can break down the clot.
- Some hemorrhagic strokes benefit from surgery.
Treatment of stroke are:
Recovery of lost function is called stroke rehabilitation & ideally takes place in a stroke unit, so these are not available in the world.
In 2013, approximately
6.9 million public an ischemic stroke
3.4 million public hemorrhagic stroke
In 2015, About 42.4 million people had ago a stroke and were still here Between 1990 to 2010, stroke cases that occurred every year reduced to approximately 10% in the developed world and increased by 10% in the developing world.
In 2015, stroke had 2nd most cases of death after coronary artery disease, accounting for 6.3 million deaths in total 11% About,
- 3.0 million deaths due to ischemic stroke
- 3.3 million deaths due to hemorrhagic stroke
About half of people who have a stroke live < 1 year.
Overall, two-thirds of strokes could occur over 65 years old patients.
Classification of stroke :
2 types
- Ischemic stroke: Causes due by a blood clot in an artery & resulting in brain death to the affected area
2. Hemorrhagic stroke: due to leakage of blood or around the brain from a ruptured blood vessel & allowing blood to pool in the affected area so increasing the pressure on the brain.
Some part of the brain of the autopsy of a person who was an acute middle cerebral artery (MCA) stroke
Strokes MCA can be classified into 2 major categories:
1 ischemic and
2 hemorrhagic.
Ischemic strokes were due to an interruption of the blood supply to the brain, hemorrhagic strokes result from the disruption of a blood vessel or an abnormal vascular structure.
About,
- 87% of strokes are ischemic,
- 13% of strokes are hemorrhagic.
Bleeding can develop inner areas of ischemia, this condition is known as “hemorrhagic transformation.”
It is not known how many hemorrhagic strokes patients actually start as ischemic strokes.
Definition:
In the 1970s, the WHO described stroke as a “neurological deficit of cerebrovascular cause that persists beyond 24 hours or is interrupted by death within 24 hours”, although the word “stroke” is an old word.
This definition had supposed to reflect the reversibility of tissue damage and had been devised for the purpose, with the time frame of 24 hours being chosen at a time.
The 24-hour limit divides stroke from transient ischemic attack, which leads to a syndrome of stroke symptoms that solving completely within 24 hours.
Availability of treatments :
Reduce stroke severity when given early,
alternative terminology is a brain attack and acute ischemic cerebrovascular syndrome (modeled after a heart attack and acute coronary syndrome, respectively) and to reflect the urgency of stroke symptoms and the need to act as smoothly.
Ischemic stroke :
The main points are Cerebral infarction and Brain ischemia
In an ischemic stroke :
blood supply to part of the brain is reduced, leading to dysfunction of the brain tissue in that parts. There are 4 reasons why this can happen.
- Thrombosis: It is an obstruction of a blood vessel by a blood clot forming generally.
2. Embolism: It is an obstruction due to an embolus from anywhere in the body.
3. Systemic hypoperfusion: It is a general decrease in blood supply,
Example: Shock Cerebral venous sinus thrombosis.
A stroke without an obvious explanation is termed cryptogenic (of unknown origin); this constitutes 30 to 40% of all ischemic stroke patients.
There are different classification systems for acute ischemic stroke.
The Oxford Community Stroke Project can be classified as OCSP which is also known as the Bamford or Oxford classification &relies primarily on the initial symptoms;
based on the extent of the symptoms,
The stroke episode is classified as 4 infarct
- total anterior circulation infarct (TACI)
- partial anterior circulation infarct (PACI)
- lacunar infarct (LACI)
- posterior circulation infarct (POCI).
These four entities predict the extent of the stroke, the area of the brain that is damaged, the underlying cause, and the prognosis.
The TOAST (Trial of Org 10172 in Acute Stroke Treatment) is classified based on clinical symptoms as well as results of further investigations; on this basis, a stroke is classified as being leads to
- thrombosis or embolism due to atherosclerosis of a long artery
- an embolism produced in the heart,
- complete blockage of a mini blood vessel,
- other determined cause,
- undetermined reason (2 possible causes, no cause identified, or incomplete investigation)
Users of stimulants like as cocaine and methamphetamine are at high risk for ischemic strokes.
Hemorrhagic stroke :
Main points :
- Intracerebral hemorrhage and Subarachnoid hemorrhage
- CT scan of an intraparenchymal bleed with surrounding edema
Intracerebral hemorrhage:
It is basically bleeding within the brain itself (when an artery in the brain bursts, flooding the surrounding tissue with blood), leads to either intraparenchymal hemorrhage (bleeding within the brain tissue)or intraventricular hemorrhage (bleeding in the brain’s ventricular system).
Subarachnoid hemorrhage :
- It is basically bleeding that occurs outside of the brain tissue but still within the skull, and precisely between the arachnoid mater and pia mater which includes the dedicated innermost layer of the 3 layers of the meninges that surround the brain.
- The above 2 main types of hemorrhagic stroke are also 2 different forms of intracranial hemorrhage, which is the accumulation of blood anywhere within the cranial vault;
- but the other forms of intracranial hemorrhage, such as epidural hematoma leads to bleeding between the skull and the dura mater,
- It is the thick outermost layer of the meninges around the brain
- and subdural hematoma (bleeding in the subdural space), has not been considered as”hemorrhagic strokes”.
- Hemorrhagic strokes can occur on the background of alterations to the blood vessels in the brain, such as cerebral amyloid angiopathy, cerebral arteriovenous malformation, and an intracranial aneurysm, it can cause intraparenchymal or subarachnoid hemorrhage.
- In addition to the neurological part, hemorrhagic strokes are usually done due to specific symptoms (for instance, subarachnoid hemorrhage classically causes a severe headache known as a thunderclap headache) or reveal evidence of a previous head injury.
Symptoms of stroke:
The symptoms of a stroke often appear without danger. Some of the major symptoms include:
- Confusion, including problems in speaking and understanding speech
- A head pain, possibly with altered consciousness or vertigo
- numbness or an in able to move parts of the face, arm, or leg, particularly on one side of the body vision problems in 1 or both eyes
- difficulty walking, including dizziness and a reduced coordination
- Stroke may lead to long-term health problems. related to the speed of the diagnosis and treatment, a person may experience temporary or permanent disabilities after a stroke.
Some people can also experience:
- bladder or bowel control problems
- depression
- paralysis or weakness on 1 or both sides of the body
- problem controlling or expressing their emotions
Symptoms vary and can range in severity.
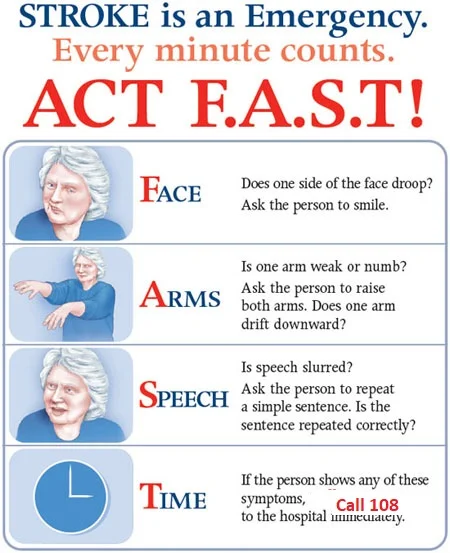
Learning the acronym “FAST” is a better way to remember the symptoms of a stroke. This may help a person seek prompt treatment. FAST stands for:
- Face drooping: If the person is trying to smile, does 1 side of their face droop?
- Arm weakness: If the person is trying to raise both arms, does one arm drift downside?
- Speech difficulty: If the person is trying to repeat a simple phrase, is their speech slurred or unusual?
- Time to act: If any of these symptoms have occurred contact the emergency services at a time.
The outcome leads to how quickly someone receives treatment. Prompt care also means that they could be less likely to experience permanent brain damage or death.
Stroke symptoms typically start suddenly, over seconds and minutes, and in most cases have not progressed further. The symptoms rely on the area of the brain affected. The more extensive the area of the cerebellum affected the more functions that are likely to be lost. Some forms of stroke may cause advanced symptoms. For e.g, in intracranial hemorrhage, the affected area can compress other structures. Most forms of stroke have not been associated with head pain, apart from subarachnoid hemorrhage and cerebral venous thrombosis, and occasionally intracerebral hemorrhage.
What are the Causes of Stroke?
Ischemic strokes and hemorrhagic strokes may happen for many reasons. Ischemic strokes also happen because of blood clots. These may happen for various reasons, such as:
- Atherosclerosis.
- Clotting diseases.
- Atrial fibrillation (especially when it can happen due to sleep apnea).
- Heart defects (atrial septal defect or ventricular septal defect).
- Microvascular ischemic disease (which can block smaller blood vessels in your brain).
- Hemorrhagic strokes may happen for several reasons also, including:
- High blood pressure, especially when you are in for a long time when it’s very high, or both.
- Brain aneurysms may sometimes lead to hemorrhagic strokes.
- Brain tumors (lead to cancer).
- Diseases that weaken or cause unusual changing in blood vessels in your brain, like moyamoya disease.
How to Diagnose stroke?
The stroke starts rapidly. For the best outcome, a person can receive treatment at a hospital within 3 hours of their symptoms first appearing.
There have several different diagnostic tests a doctor can use to determine the type of stroke. These include:
Physical examination:
A doctor can ask about the person’s symptoms and medical history. They will have to check muscle strength, reflexes, sensation, vision, and coordination. They will also check blood pressure, listen to the carotid arteries in the neck, and examine the blood vessels at the back of the eyes.
Blood tests: A doctor can perform blood tests to determine if there have a high risk of bleeding or blood clots, measure levels of particular substances in the blood, including clotting factors, and check whether or not an infection is present.
CT scan:
A series of X-rays may show hemorrhages, strokes, tumors, and other conditions within the brain.
MRI scan:
These are using radio waves and magnets to create an image of the brain, which a doctor may use to detect damaged brain tissue.
Carotid ultrasound:
A doctor can carry out an ultrasound scan to check blood flow in the carotid arteries and to see if there have any narrowing or plaque present.
Cerebral angiogram:
A doctor can inject a dye into the brain’s blood vessels to make them visible under X-ray or MRI. This is providing a detailed view of the blood vessels in the brain and neck.
Echocardiogram:
his is creating a detailed image of the heart, which doctors may use to check for any sources of clots that could have traveled to the brain.
It has only possible to confirm the type of stroke using a brain scan in a hospital environment.
Risk factors
The most important modifiable risk factors for stroke have high blood pressure and atrial fibrillation although the size of the effect has small; 833 people are to be treated for one year to prevent one stroke.
Other modifiable risk factors can include:
- high blood cholesterol levels,
- diabetes mellitus
- end-stage kidney disease
- cigarette smoking (active and passive),
- hard alcohol use
- drug use
- lack of physical activity
- obesity
- processed red meat consumption, and not a proper diet.
Smoking just 1 cigarette per day can increase the risk by>30%. Alcohol can use predispose to ischemic stroke, as well as intra-cerebral and sub-aranchoid hemorrhage via multiple mechanisms (e.g., via hypertension, atrial fibrillation, rebound thrombo- cytosis, and platelet aggregation and clotting disturbances).
Drugs, most commonly amphetamines and cocaine, may induce stroke through damage to the blood vessels in the brain and acute hypertension. Migraine with aura doubles a person’s difficulty for ischemic stroke.
Nontreated, celiac disease regardless of the presence of symptoms can be an underlying cause of stroke, both in children and adults.
High levels of physical activity can reduce the risk of stroke by about 26%. There has a lack of high-quality studies looking at promotional efforts to improve lifestyle factors. Nonetheless, can be given the long body of circumstantial evidence, the best medical management for stroke includes advice on diet, exercise, smoking, and alcohol use.
Medication has the most common method of stroke prevention; carotid endarterectomy may be a useful surgical method of preventing stroke.
Blood pressure
High blood pressure accounts for 35–50% of stroke risk. Blood pressure is a reduction of 10 mm Hg systolic or 5 mm Hg diastolic may reduce the risk of stroke by ~40%.
Lowering blood pressure can be conclusively shown to prevent both ischemic and hemorrhagic strokes. It has equally important in secondary prevention. Those people older than 80 years and who are isolated with systolic hypertension benefit from anti-hypertensive therapy.
The available evidence has not to show large differences in stroke prevention between antihypertensive drugs—therefore, other factors like protection against other forms of cardiovascular disease and cost could be considered. The routine can use B-blockers following a stroke or TIA is not been shown to result in benefits.
Blood lipids
High cholesterol levels have inconsistently associated with (ischemic) stroke. Statins can be shown to reduce the risk of stroke by about 15%. Since earlier meta-analyses of other lipid-lowering drugs were not showing a decreased risk, statins could exert their effect by mechanisms other than their lipid-lowering effects.
Diabetes mellitus
Diabetes mellitus can increase the risk of stroke by 2 to 3 times. While intensive blood sugar control can be shown to reduce small blood vessel complications such as kidney damage and damage to the retina of the eye it can’t be shown to reduce large blood vessel complications such as stroke.
Anticoagulation drugs
Oral anticoagulants such as warfarin are the mainstay of stroke prevention for over 50 years. However, several studies can be shown that aspirin and other antiplatelets are highly effective in secondary prevention after a stroke or transient ischemic attack. Low doses of aspirin (for example 75–150 mg) have as effective as high doses but are fewer side effects; the lowest effective dose remains unknown.
Thienopyridines (clopidogrel, ticlopidine) could be slightly more effective than aspirin and have a decreased risk of gastrointestinal bleeding but have more expensive.
Both aspirin and clopidogrel can be useful in the 1st few weeks after a minor stroke or high-risk TIA. Clopidogrel is fewer side effects than ticlopidine. Dipyridamole may be added to aspirin therapy to provide a small additional benefit, even though headache has a common side effect. Low-dose aspirin can also be effective for stroke prevention after having a myocardial infarction.
For those with atrial fibrillation is a 5% year risk of stroke, and this risk can higher in those with valvular atrial fibrillation. Depending on the stroke risk, anticoagulation with medications like warfarin or aspirin is useful for prevention. Except in people with atrial fibrillation, oral anticoagulants should not be advised for stroke prevention—any benefit can be offset by bleeding risk.
In primary prevention, however, antiplatelet drugs had not reduced the risk of ischemic stroke but increased the risk of major bleeding. Further studies have been needed to investigate a possible protective effect of aspirin against ischemic stroke in women.
Surgery
Carotid endarterectomy or carotid angioplasty may be used to remove atherosclerotic narrowing of the carotid artery. There has evidence supporting this procedure in selected cases.
Endarterectomy for significant stenosis is shown to be useful in preventing further strokes in those who is already had one. Carotid artery stenting can not be shown to be equally useful.
People have been selected for surgery based on age, gender, degree of stenosis, time since symptoms, and the person’s preferences. Surgery may most efficient when not delayed too long—the risk of recurrent stroke in a person who is 50% or greater stenosis is up to 20% after 5 years, but endarterectomy decreased this risk to around 5%.
The number of procedures needed to cure 1 person was 5 for early surgery (within 2 weeks after the initial stroke), but 125 if could delay longer than 12 weeks.
Screening for carotid artery narrowing can not be shown to be a useful test for the general public. Studies of surgical intervention for carotid artery stenosis without symptoms can be shown only a small decrease in the risk of stroke.
To get adv the complication rate of the surgery could be kept below 4%. Even then, for 100 surgeries, 5 people may benefit by avoiding stroke, 3 can develop stroke despite surgery, 3 may develop stroke or die due to the surgery itself, and 89 will remain stroke-free but would also are done so without intervention.
Diet
Nutrition, specifically the Mediterranean-style diet, is the potential for decreasing the risk of having a stroke by more than half. It has not seen that lowering levels of homocysteine with folic acid affects the risk of stroke.
A Centers for Disease Control and Prevention public service announcement about a woman having a stroke after pregnancy.
Women
A number of specific recommendations can be made for women including taking aspirin after the 11th week of pregnancy if there has a history of previous chronic high blood pressure and taking blood pressure medications during pregnancy if the blood pressure can > 150 mm Hg systolic or greater than 100 mm Hg diastolic. In those who can previously have preeclampsia other risk factors should be treated more aggressively.
Previous stroke or TIA
Keeping blood pressure below 140/90 mmHg has recommended. Anticoagulation may prevent recurrent ischemic strokes. Among people with nonvalvular atrial fibrillation, anticoagulation may reduce stroke by 60% while antiplatelet agents will reduce stroke by 20%. However, a recent meta-analysis is suggesting harm from anticoagulation started early after an embolic stroke. Stroke prevention treatment for atrial fibrillation has been determined according to the CHA2DS2–Vasc score. The most widely can be used anticoagulant to prevent thromboembolic stroke in people with nonvalvular atrial fibrillation is the oral agent warfarin while a number of newer agents including dabigatran are alternatives that can not require prothrombin time monitoring.
Anticoagulants, when used following a stroke, could not be stopped for dental procedures.
If studies show carotid artery stenosis, and the person can a degree of residual function on the affected side, carotid endarterectomy (surgical removal of the stenosis) can decrease the risk of recurrence if performed rapidly after stroke.
Treatment of Stroke:
Medical:
Treating ischaemic strokes
If you have an ischaemic stroke, a combination of medicines to treat the condition and prevent it from happening again can usually recommend.
Some of these medicines need only Thrombolysis – “clot buster” medicine, it can be started once the stroke has been treated and may need to be taken long-term.
This use of “clot-busting” medicine can be known as thrombolysis.
Alteplase has most effective if started as soon as possible after the stroke occurs – and certainly within four and half hours.
It’s not generally recommended if more than 4.5 hours have passed, as it has not clear how beneficial it is when used after this time.
Before alteplase can be used, it’s very important that a brain scan is done to confirm a diagnosis of an ischaemic stroke.
This is because the medicine may make the bleeding that occurs in hemorrhagic strokes worse.
Thrombectomy
A small number of severe ischaemic strokes may be treated by an emergency procedure called a thrombectomy.
This removes blood clots and helps restore blood flow to the brain.
Thrombectomy is only effective at treating ischaemic strokes caused by a blood clot in a large artery in the brain.
The procedure involves inserting a catheter into an artery, often in the groin. A small device is passed through the catheter into the artery in the brain.
The blood clot may then be removed using the device or through suction. The procedure can be done under local anesthetic or general anesthetic.
Aspirin and other antiplatelets
Most people will be given aspirin straight after having an ischaemic stroke. As well as being a painkiller, aspirin is antiplatelet, which reduces the chances of another clot forming.
Other antiplatelet medicines may be used later, such as
- clopidogrel and dipyridamole.
- Anticoagulants
- Warfarin, apixaban, dabigatran, edoxaban and rivaroxaban are examples of anticoagulants for long-term use.
There are also a number of anticoagulants called heparins, which can only be given by injection and are used short-term.
Anticoagulants may be offered :
If you can a type of irregular heartbeat called atrial fibrillation, which can cause blood clots could a history of blood clots can develop a blood clot in your leg veins (deep vein thrombosis (DVT)) because a stroke has left you unable to move one of your legs
Blood pressure medicines
If your blood pressure is too high, you may be offered medicines to lower it.
Medicines that have commonly used include:
- thiazide diuretics
- angiotensin-converting enzyme (ACE) inhibitors
- calcium channel blockers
- beta-blockers
- alpha-blockers
Statins reduce the level of cholesterol in your blood by blocking a chemical (enzyme) in the liver that produces cholesterol.
You may be offered a statin even if your cholesterol level is not particularly high, as it may help reduce your risk of stroke whatever your cholesterol level is.
Carotid endarterectomy
Some ischaemic strokes can cause by the narrowing of an artery in the neck called the carotid artery, which can carry blood to the brain.
Botulinum Toxin
Muscle Relaxant drugs can be fitted into hyperactive discontinuous muscles to locally block spasticity.
Botulinum Toxin A in addition to recreation remedy may be used to reduce upper branch spasticity but is doubtful to ameliorate functional exertion or motor function.
Botulinum Toxin A in addition to recuperation remedy may be useful for perfecting muscle tone in cases with lower branch spasticity but is doubtful to ameliorate motor function or walking.
Physiotherapy Treatment:
Positioning
The ability to change position and posture has been affected in many individuals post-stroke as a result of varying degrees of physical impairments. Showing Stroke: Positioning
- Practice Statement
- Consensus-based Recommended
- Initial specialist assessment for positioning could cause an acute stroke as soon as possible and where
- possible within four hours of arrival at the hospital.
- Arm Support devices like a Lap Tray may be used to assist with arm positioning for those at risk.
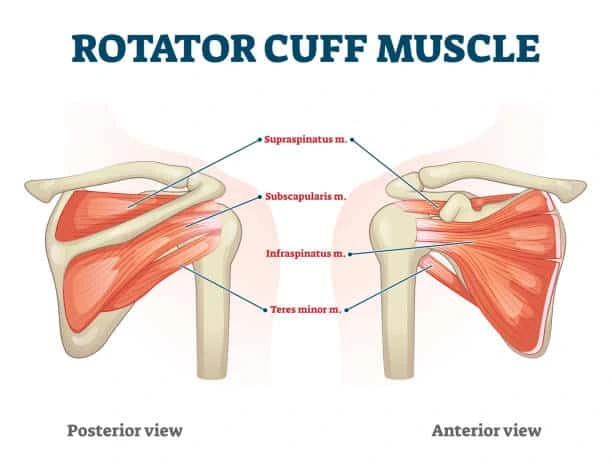
shoulder subluxation
Education and training around correct manual handling and positioning could be provided to the
individual with stroke, those family/carers,s and health professionals, particularly nursing and other allied health staff.
Elevation of the limb when resting could be considered for individuals who are immobile to prevent swelling in the hand and foot.
Early Mobilisation
Immobility is associated with a number of post-stroke complications like deep vein thrombosis etc.
Implementing an Early able-to-move Program for Critically Ill Patients.
Patients with difficulty moving after stroke could be assessed as soon as possible within the first 24 hours and trained healthcare professionals to detain the most appropriate and safe methods of transfer and mobilization.
Commence mobilization (out-of-bed activity) within 24 to 48 hrs of stroke onset until receiving palliative care.
Starting intensive out-of-bed activities within 24 hours of stroke onset has not recommended. Mobilization within 24 hours of onset might only be for patients who require little or no assistance to mobilize.
Balance training
Balance difficulties are common for many individuals after a stroke usually cause to a combination of less body and trunk motor control, altered sensation, and partially centrally determined alteration in body representation such as the patient misperceiving their posture in relation to the upright.
Impaired balance causes to loss of confidence, and fear of falling, and increases the risk of falls. Current evidence suggests that trunk exercise training will improve trunk performance and dynamic sitting balance, while task-specific training improves dynamic balance in both sitting and standing.
Sitting
Practicing to reach beyond arm’s length while sitting with supervision/assistance might be under observation for individuals who have difficulty with sitting.
Standing
Strategies could include:
The practice of standing balance could be provided for individuals who have difficulty with standing.
- Walking training that added challenge to standing balance (e.g. overground walking, obstacle courses)
- Provides visual or auditory feedback
- Receive progressive balance repeatedly training
- Received lower limb strengthening exercises
- advise for an ankle-foot orthosis
Gait & Mobility
- The high priority for many people with limited ability to move after a stroke has to walk independently. If walking
- performance has not good after the stroke, community activity shall be limited and the patient may become
- housebound and isolated from society. See Gait Training in Stroke
- Strong Recommendation
- Tailored repetitive practice of walking (or components of walking) could be practiced as much as possible
- for individuals with difficulty walking. The following modalities may be used to achieve this:
- Circuit Class Therapy (focusing on overground walking practice) Treadmill Training with or without body weight support
- Virtual Reality Training
Other interventions can be used in addition to those above:
Electromechanically Assisted Gait Training
Biofeedback
Cueing of Cadence
Functional Electrical Stimulation
Treadmill Training
Treadmill training may be utilized for both Gait education and Training but also to aid improvements in aerobic function. Treadmill training should be completed with the patient’s body weight some part supported by a harness in order to grade the amount of body weight supported, which can be used for individuals with significant functional limitations. See Gait training in stroke.
People who are able to walk independently after stroke should be offered treadmill training with or without body weight support or other walking-orientated interventions at a higher intensity than usual care and as an adjunct to other treatments. (Level 1)
Electromechanical Assisted Robotic-Gait-Training
Electromechanical-assisted gait training, with and without partial body weight support as well as with or without FES, is used as an adjunct to overground gait training for the rehabilitation of patients after stroke and can be used to give non-ambulatory patients intensive practice (in terms of high repetitions) of complex gait cycles.
Automated electromechanical gait machines consist either of a robot-driven exoskeleton orthosis or an electromechanical solution with two driven foot-plates simulating the phases of gait and offer reduced effort for therapists, as they no longer need to set the paretic limbs or assist trunk movements.
The main difference between electromechanical-assisted and treadmill training is that the process of gait training is automated and supported by an electromechanical solution.
Current research indicates that repetitive gait training in combination with physiotherapy may improve walking ability in patients after stroke.
See the Video of Robotic Rehabilitation for the Lower Extremity.
A patient who can’t walk after a stroke would be led to electromechanical-assisted gait training including body weight support.
Rhythmic Cueing Metronome
Motor Control research shall provide consider as proof that auditory rhythm will improve timing and variability of motor responses, specifically, in motor tasks with different timing requirements or in disorders affected timing, external rhythm may provide additional stability to timekeeper mechanisms in the brain.
Cueing of Cadence will be utilized in addition to conventional gait training for improved stride length & gait speed.
Virtual Reality
Advances in virtual reality technology meaning that devices can use computer and gaming technology, such as the Nintendo Wii, are now found in many people’s houses. The potential of these types of adjuncts to maximize task-related practice and increase energy expenditure has begun to be explored. Show Virtual Reality for Individuals infected by Stroke
Virtual Reality Training can be regained in addition to conventional gait training.
Overground Walking 4 Point Walker
Overground walking includes walking and walking-related activities on a solid surface, where the therapist can observe the patient’s gait, also on a level surface, and can the patient do a range of different activities and exercises to influence the patient gait.
The advantage has that over-ground gait training may be used in almost any setting or location not requiring a great deal of high-tech equipment.
It can be demo overground gait training by stroke patients who have the ability to walk without physical support is more effective in increasing walking distance and decreasing stress than walking on a treadmill.
Community Walking
Individualized goals could be set and assistance with adaptive equipment, information, and further referred to other agencies would be provided for individuals who can difficulty with outdoor mobility in the community.
Walking training can be good for some individuals and if provided, should include in a variety of community settings and environments, and can also incorporate virtual reality training that mimics community walking.
Orthotics
AFO ( ankle foot orthotics)
Orthotics can be an intervention designed to change body parts; support and stabilize not responsive muscles so an activity will be performed, or be an adjunct to enable participation in a life role example work.
KNGF Clinical Guidelines recommends a trial of Ankle Foot Orthotics for patients whose safe and/or efficient walking ability is impeded by drop foot during the swing phase of walking following Multidisciplinary consultation.
regularly fitted lower limb orthoses can be used to shorten limitations in walking ability. Improvement in walking can cause while the orthosis is worn.
Upper Limb Training
85% of gradually after stroke experience altered arm function, with approximately 40% of individuals being infected by upper limb function long time. Lost of arm function side effect quality of life, and functional motor recovery in affected upper body parts in patients with hemiplegia has the primary goal of physical therapists. “recently ether has no high-quality proof for any interventions that have daily life practice, and evidence can insufficient to enable comparison of the relative effectiveness of interventions.” In other words, the proof has insufficient to show which of the interventions are the most effective for improving upper limb function”.
Patients with stroke with potential or actual arm movement would be given every opportunity to practice functional activities that incorporate movements that have of high intensity, repetitive, and task-specific. These activities can be bilateral or unilateral depending on the task.
Bilateral Arm Training
Bilateral Arm Training considers intensive training of bilateral coordination able to practice bimanual skills. During bilateral arm training, movement patterns or activities can be performed with both hands regularly but independent from each other and may also be cyclic.
This approach was developed in response to identified limitations of Constraint Induced Movement Therapy (CIMT) which precludes the opportunity to practice bilateral skills particularly functional activities that are inherently bimanual.
Unilateral and bilateral training is similarly effective. However, intervention success can depend on the severity of upper extremities paresis and the time of intervention post-stroke.
Bilateral arm training can be used as part of comprehensive goal-directed rehabilitation. Although, when matched for dosage, unilateral training may be more effective.
Constraint Induced Movement Therapy
Constraint-induced movement therapy (CIMT) includes intensive targeted practice with the affected limb while restraining the nonaffected body part, it means during task-specific practice, individuals with hemiplegic stroke have been forced to use their affected limb. See Constraint Induced Movement Therapy
Original CIMT Applicable for 2 to 3 weeks consisting of immobilization of the non-paretic arm with a padded mitt for 90% of working hours induced task-oriented training with a high no of repetitions for 6 hours in one day; and behavioral strategies to improve both compliance and transfer of the activities practicing from the clinical setting to the patient’s home environment.
High-intensity mCIMT Consists of immobilization of the non-paretic arm with a padded mitt for 90% of waking hours with between 3 to 6 hours of task-oriented training one day. Found to be more beneficial in the starting stage of rehabilitation with minimum effect on chronic upper limb impairment.
Low-intensity mCIMT Consisted of immobilization of the normal arm with a padded mitt for greater than 0% to < 90% of waking hours with between 0 to 3 hours of task-oriented training a day.
Intensive Constraint Included Movement Therapy (minimum 2 hours of active therapy per day for 2 weeks, adds restraint for at minimum 6 hours a day) could be provided to increase arm and hand use alone with 20 degrees of active wrist extension and 10 degrees of active finger extension.
Trunk restraint can also be operated into the active therapy periods at any stage post-stroke.
Electrical Stimulation
Functional Electrical Stimulation looks like it moderately improves upper body part activity compared with both no intervention and training alone. Current proof described that electrical stimulation could be used in stroke rehabilitation to improve the ability to perform functional upper body parts functions. See Electrical Stimulation
Robot-Assisted Arm Training
The robot-mediated treatment utilizes automatic devices to provide passive, active, or resistive limb movement which should allow for extended periods of treatment that are responsive to the particular needs of the one by one using the person’s movement as feedback, as the ability to change during time. There has now conflicting proof and there has still limited proof to suggest when or how the robot-assisted arm movement could be used. People with decreased arm function post-stroke would only be offered robot-assisted movement therapy or neuromuscular electrical stimulation as an adjunct to conventional therapy in the context of a clinical trial.
Show Robotic Rehabilitation Lower Extremity and Upper Extremity.
Robot/ Mechanical supported arm training would be used to ameliorate upper body part function in individualities with mild to severe arm weakness after stroke” such an adjunct to conventional remedy in the environment of a clinical trial”.
virtual reality
The substantiation base for virtual reality and interactive videotape gaming- grounded interventions for the arm( like an adjunct to usual care to increase overall remedy time) has developed, though studies have frequently been of lower quality and further exploration is demanded.
Mirror Therapy
Mirror Therapy can be used as an adjunct to routine remedies to ameliorate arm function after stroke for individualities with mild to moderate weakness, complex indigenous pain patterns,s and/ or neglect.
Mental Practice
Motor imagery( MI) has an internal process of trial for a given action in order to ameliorate motor function while Mental Practice( MP) has a training system that cognitively demonstrates a physical skill using MI in the not presence of overt, physical movements for the moto of increase motor skill performance. Show Mental Imagery
Weak Recommendation
Mental practice, which has no cognitive impairment exists, in connection with active motor train shall be used to ameliorate arm function for individuals with mild to moderate weakness in their arm.
Splinting
Routine practices are similar not include Hand and wrist orthoses( slivers) as they can have nothing effect on function, pain, or range of movement.
Cardiorespiratory Training
There has an additive range of aerobic exercise options being penetrated by people with the following Stroke. These range from aerobic exercise programs like overground walking or routine training programs and an array of sporting and exercise classes to the use of technology(e.g. virtual reality training). These options, supported by the growing body of evidence, present the therapist and case with the capability to elect a program for individual timing and should be carried out in an applicable terrain. See Stroke The part of Physical exertion.
Rehabilitation would induce collective flashback exercise interventions to increase cardiorespiratory fitness.
Exercise Statement
Consensus- grounded Recommendations
Commence cardiorespiratory training during their inpatient stay.
Encourage them to share in ongoing regular physical exertion anyhow of the position of disability.
Strength Training
Progressive resistance training would be offered to those with decreased strength in their arms or legs.
Circuit Class
Van de Port et al( 2012) set up that task-acquainted circuit training in cases with mild to moderate disability after stroke is safe and as effective as a collectively adjusted face-to-face treatment in the first six months after stroke but wasn’t superior to usual care in terms of tone reported mobility according to the mobility sphere of the stroke impact scale.
Circuit training did prove further effective in terms of walking speed, stair walking, and walking distance, though differences were small; 9 cm/ s for walking speed and 20 m for walking distance, independently. There’s also growing approval that circuit training is effective at perfecting the walking faculty of cases in the habitual phase of stroke.
The benefit of Circuit Training is Another important aspect of the task acquainted circuit training is that it’s offered in groups ranging from two to eight cases, lowering rates of staff to cases and thus a possible further cost-effective treatment.
Hydrotherapy
destruction in water can enhance the treatment of neurologically bloodied individualities with both remedial, cerebral, and social benefits.
Hydrotherapy is the term used for exercise in warm water and is a popular treatment for cases with neurologic and musculoskeletal conditions and is defined by the Hydrotherapy Association of Chartered Physiotherapists Guidance on Good Practice in Hydrotherapy as a remedy program using the parcels of water, designed by a suitably good physiotherapist, to improve function, perfectly in a purpose- erected and suitably heated hydrotherapy pool.
Merholz et al( 2011) set up inadequate approval to conclude that water-grounded conditioning for people after a stroke is effective for reducing disability but likewise set up inadequate approval to conclude that water-grounded exercises are ineffective or indeed dangerous.
A recent RCT showed positive results and a large enhancement in high-position balance and walking function after a 4- week hydrotherapy program. Further exploration is needed which needs to concentrate on advanced and larger RCTs to estimate the effectiveness of water-grounded exercises for people after stroke. A randomized control trial suggests that submarine remedy has positive issues, contributing to perfecting cases’ moods and quality of life with acquired brain injury.
Electrotherapy
Electrical stimulation may be used for those with reduced strength in their arms or legs( particularly for those with lower than antigravity strength).
Electrical stimulation may be used to help or reduce shoulder subluxation.
Spasticity Management
There’s considerable debate on the description, physiological nature, and significance of spasticity. Spasticity can create discomfort or pain and can be associated with exertion limitation. Spasticity is common, especially in anon-functional arms with a close association between spasticity and other impairments of arm function and mobility.
Stretch
Stretch may be applied in a number of ways during neurological recovery to achieve different goods. The types of stretching used include; Fast/ Quick, Dragged, and Maintained. presently the approval for stretching in stroke recuperation is weak in relation to its use in spasticity operation.
Routine use of stretch to reduce spasticity isn’t recommended.
Adjunct curatives to Botulinum toxin A similar to electrical stimulation, casting, taping, and stretching may be used to reduce spasticity.
Surgical treatment:
Contracture operation
A muscle contracture is an endless shortening of a muscle or joint. It’s generally in response to dragged hypertonic spasticity in a concentrated muscle area. Contractures aren’t uncommon in branches affected by spasticity. Contractures can stymie conditioning similar to washing or putting on clothes, and may also be uncomfortable or painful and limit the capability to sit in a wheelchair or mobilize. A careful to determine whether stretch increases common mobility in people with contractures or those at threat of developing contractures provides moderate to high-quality substantiation that stretch, whether unresistant or through the means of flake or serial casting, doesn’t have a clinically important effect on common mobility in people with neurological conditions.
For people with stroke at threat of developing contracture, routine use of slivers or dragged positioning of upper or lower branch muscles in a dragged position( stretch) isn’t recommended.
For stroke survivors, periodical casting may be trialed to reduce severe, patient contracture when the conventional remedy has failed. For stroke survivors at threat of developing contracture or who have developed contracture, active motor training to evoke muscle exertion should be handed.
Fatigue operation
Fatigue is a common complaint post-stroke, and is apparent indeed in those individuals who have made an else complete recovery. Over 40 of long-term stroke survivors report ongoing issues with fatigue which impacts on their diurnal living conditioning with a lack of energy and/ or an increased need to rest every day, as the main characteristics which can be brought on by both internal and physical exertion.
Fatigue has also been associated with depression, and maybe a predictor of shorter survival. operation strategies include the identification of triggers and re-energizers, environmental variations and life changes, scheduling and pacing, cognitive strategies to reduce internal trouble, and cerebral support to address mood, stress, and adaptation.
Individuals with stroke who are medically stable but who report fatigue should be offered an assessment for internal and physical factors that may be contributing, particularly when engagement with healing or quality of life is affected.
- Consensus-grounded Recommendations
- remedy for stroke survivors with fatigue should be organized for ages of the day when they’re most alert.
- Information and education about fatigue should be handed to individuals with Stroke and their Family Caregivers.
- Implicit modifying factors for fatigue should be considered including avoiding sedating medicines and alcohol, screening for sleep-related breathing diseases, and depression
- While there’s inadequate substantiation to guide practice, possible interventions could include exercise and perfecting sleep hygiene
- If your doctor sees that an aneurysm has burst, they may do surgery to clip the aneurysm and prevent additional bleeding. Likewise, a craniotomy may be needed to relieve the pressure on the brain after a large stroke.
- In addition to emergency treatment, your healthcare team will advise you on ways to prevent future strokes.
Occupational therapy:
This will help retrain your brain so you may go about your ADL. This therapy can be especially helpful in improving precise hand movements and muscle control.
Speech therapy:
- A stroke may lead to speech and language impairment. A speech and language therapist can work with you to relearn how to speak.
Or
- if you can find verbal communication difficult after a stroke, they can help you find new ways of communication.
Cognitive therapy:
- After a stroke, many people can have changes to their thinking and reasoning skills. This will lead to behavioral and mood changes.
- An occupational therapist will help you work to regain your former patterns of thinking and behavior and manage your emotional responses.
Psychological treatment:
Psychotherapy
This can often be referred to as “talk therapy” where you are sitting down and speaking to a trained therapist, which could help with a variety of psychiatric disorders including post-stroke depression. If therapy has started early, it can even help prevent post-stroke depression altogether.
Positive psychology
While traditional psychology is focusing on mental illness, positive psychology focuses on mental wellness. It is focusing on creating states of happiness, meaning, and fulfillment by using exercises that help retrain the brain. The book Healing & Happiness After Stroke can touch on positive psychology for stroke survivors.
Mindfulness
This includes the practice of living in the present moment rather than tension about the past or future. There have apps that help with mindfulness, such as mental space.
Cognitive behavior therapy (CBT):
This modality of therapy has based on the idea that our emotions occur due to our thoughts. Challenging negative self-talk will help you improve your psychological well-being.
FAQs
instant deadness or weakness in the face, arm, or leg, mostly on one side of the body. instantly confusion, trouble speaking, or difficulty comprehending speech. instant problem seeing in one or both eyes
Stress can lead the heart to work harder, increase blood pressure, and increase sugar and fat levels in the blood. These things, in turn, can enlarge the risk of clots forming and traveling to the heart or brain, leading to heart attack or stroke.
No two strokes are the same. Some people can experience more such themselves within just a few days, without any lasting physical or good issues. But for others, it can take some months to heal or adjust to any long-term effects.
each stage according to the Brunnstrom approach:
Stage 1:Flaccidity.
Stage 2: Spasticity showing.
Stage 3: Increased Spasticity.
Stage 4: Decreased Spasticity.
Stage 5: Complex Movement Returns.
Stage 6: Spasticity disappears.
Stage 7: Normal Function Returns.
A silent stroke leads to a stroke that doesn’t cause any detectable symptoms. Most strokes are caused by a clot that blocks a blood vessel in the brain. The blockage stops blood and oxygen from reaching that area, causing nearby brain cells to die.


16 Comments