Posterior Pelvic Tilt
Table of Contents
What is a Posterior Pelvic Tilt?
Posterior pelvic tilt is a biomechanical condition characterized by the rotation of the pelvis in a backward direction, causing the pelvic bones to tilt posteriorly.
This movement is mostly linked to changes in the pelvic position, which impact the spine’s alignment and posture in general. Although some degree of pelvic tilt is necessary for the best possible function and range of motion, an excessive posterior pelvic tilt can result in a number of musculoskeletal problems.
The distribution of forces throughout the body can be impacted by a change from the neutral position of the pelvis, which is vital for stabilizing and supporting the spine. People who have a posterior pelvic tilt may have symptoms including tight hip flexors, lower back pain, and abnormal biomechanics when walking or standing.
Effective preventive and treatment options for posterior pelvic tilt require a thorough understanding of the condition’s cause, symptoms, and possible outcomes. In order to treat this problem and improve general musculoskeletal health, a mix of focused workouts, postural awareness, and, in certain situations, expert advice is required.
Related Anatomy
It is necessary to investigate the structures involved in pelvic movement and stability before delving into the anatomy connected to posterior pelvic tilt. Anatomical components of note include:
Pelvis:
The bony structure that joins the lower limbs to the spine is called the pelvis. It is made up of the coccyx, sacrum, and two hip bones, each of which is made up of the pubis, ischium, and ilium.
The pelvic girdle bears the weight of the body and provides a strong base for the spine. Alignment correctly is essential for best performance.
Spine:
The lumbar spine, one of the areas of the spine, is especially important in relation to posterior pelvic tilt. The five vertebrae (L1–L5) that make up the lumbar spine join the thoracic spine and sacrum.
Muscles:
When it comes to pelvic tilt, the iliopsoas muscle is important. An anterior pelvic tilt may be caused by tight hip flexors, which may then have an impact on pelvic posture.
Hamstrings: Pelvic tilt can have an impact on these rear thigh muscles, particularly in situations when posterior pelvic tilt is present.
Connective Tissues:
Ligaments: The sacroiliac ligaments and other pelvic ligaments support pelvic stability. The tension and functionality of these ligaments can be affected by modifications in pelvic tilt.
Understanding the interaction among these anatomical components is essential to understanding posterior pelvic tilt mechanics. This biomechanical issue can be caused by structural differences, muscle imbalances, and ligamentous laxity.
Type of Pelvic Tilt
The direction in which the pelvis rotates distinguishes the several forms of pelvic tilt, each of which can present itself in a variety of ways. There are 3 main forms of pelvic tilt:
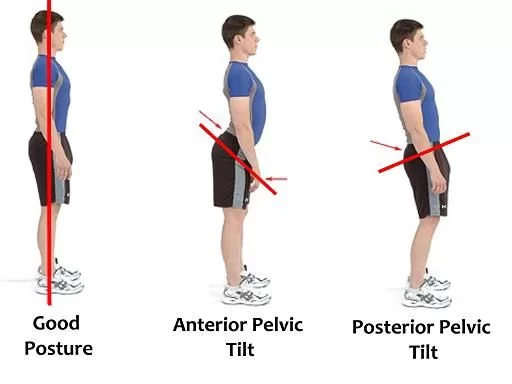
When there is an anterior pelvic tilt, the front of the pelvic bone is lower than the rear due to the pelvis rotating forward. This causes the abdomen to protrude and the lower spine to curve further (lumbar lordosis). Anterior pelvic tilt is frequently caused by weak ab and gluteal muscles as well as tight hip flexors.
Posterior Pelvic Tilt:
In contrast, the pelvis rotates backward in a posterior pelvic tilt, putting the back of the pelvic bone lower than the front. This kind of tilt may cause the lower back to round out and flatten the normal lumbar curvature. Posterior pelvic tilt can be caused by abnormalities in core muscles, weak hip flexors, and tight hamstrings.
One hip will sit higher than the other due to lateral pelvic tilt, which is the tilting of the pelvis to one side. This lateral displacement may have an impact on the spine’s alignment, resulting in an uneven trunk and shoulders. Scoliosis, uneven leg length, hip abductors, and adductor muscle imbalances are common causes of lateral pelvic tilt.
Causes of Posterior Pelvic Tilt
Numerous causes might contribute to posterior pelvic tilt, but a combination of muscle imbalances, lifestyle decisions, and structural problems is frequently the primary cause. Typical reasons include some of the following:
Muscle Imbalances:
Weak Abdominal Muscles: A difficulty in supporting the pelvis in an anterior posture may be caused by a lack of strength in the abdominal muscles, namely the rectus abdominis and transverse abdominis.
Tight Hamstrings: A posterior pelvic tilt can be caused by hamstrings that are too short and too tight, which can force the pelvis backward.
Hip Flexor Tightness:
A posterior pull from tightness in the hip flexors, particularly the iliopsoas muscle, can cause the pelvis to tilt backward.
Imbalanced Gluteal Muscles:
Pelvic misalignment may result from weakness in the gluteal muscles, particularly the gluteus maximus, which extends the hip.
Sitting Habits:
Sitting for extended periods of time, especially when slouched or unsupported, can lead to postural problems such as posterior pelvic tilt and muscular imbalances.
Structural Factors:
Sacroiliac Joint Dysfunction: Pelvic tilt may be caused by problems at the sacroiliac joint, which is where the sacrum and ilium meet.
Leg Length Disparity: When there is a disparity in leg length, the pelvis may experience unequal pressures that might push it backward.
Postural Habits:
Over time, poor postural patterns that cause pelvic tilt include slouching and standing with an excessive curve in the lower back.
Genetics:
A hereditary tendency to specific anatomical or biomechanical problems that lead to posterior pelvic tilt may exist in certain situations.
Inactivity and Weak Core Muscles:
Insufficient exercise and weak core muscles can exacerbate postural problems and muscular imbalances, including pelvic pain.
Identifying certain characteristics contributing to a person’s posterior pelvic tilt is essential to developing a treatment and preventative strategy that works.
Posterior Pelvic Tilt Symptoms
The symptoms of posterior pelvic tilt can vary widely and in intensity from person to person. The following are typical signs of posterior pelvic tilt:
One of the most typical symptoms is lower back pain, which is frequently accompanied by lumbar soreness or hurting. This may be the outcome of the spine’s changed curvature brought on by posterior pelvic tilt.
Hip Pain:
Hip pain or discomfort is common in those with posterior pelvic tilt, particularly in the back and sides. The muscles around the hip joint have changed in tension and location, which is responsible for this.
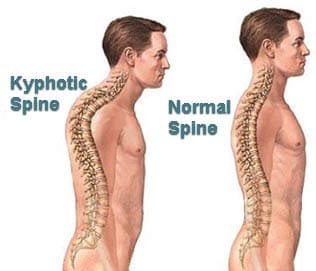
Reduced Lumbar Lordosis:
The normal lumbar curvature flattens when there is a posterior pelvic tilt. Lower back stiffness and soreness might be attributed to this decrease in lumbar lordosis.
Tight Hamstrings:
The normal lumbar curvature flattens when there is a posterior pelvic tilt. Lower back stiffness and soreness might be due to this decrease in lumbar lordosis.
Poor Posture:
A readily identifiable posture with a flattened lower back and projecting belly is caused by posterior pelvic tilt. The entire spine may be out of alignment as a result, impacting posture as a whole.
Gait Abnormalities:
The mechanics of walking can be impacted by modifications in pelvic position. A swaying or altered gait may be seen in individuals with posterior pelvic tilt, which may cause pain or instability when walking.
Sciatic Nerve Irritation:
A posterior pelvic tilt may occasionally aggravate the sciatic nerve, resulting in symptoms like numbness, tingling, or radiating pain in the buttocks and down the back of the leg.
Difficulty with Activities:
People with posterior pelvic tilt may find it difficult or painful to do specific tasks, such as standing for long periods of time, lifting things, or exercising.
Muscle Imbalances:
Unbalances in muscle strength and flexibility may result from the tilt, and they might cause further discomfort or exacerbate pre-existing musculoskeletal conditions.
It’s crucial to remember that each person may experience posterior pelvic tilt differently in terms of its degree and particular symptoms.
Anterior Pelvic Tilt v/s Posterior Pelvic Tilt
Two separate biomechanical problems affecting the rotation of the pelvis are anterior and posterior pelvic tilts. The two are compared as follows:
- Pelvic Orientation:
- Anterior Pelvic Tilt (APT): In APT, the front of the pelvic bone is lower than the back due to a forward rotation of the pelvis. An expanded lumbar lordosis (arch) and a projecting belly are the outcomes of this.
- Pelvic tilt to the posterior (PPT): PPT is a rotation of the pelvis in which the back of the pelvis is positioned lower than the front. This may result in a rounded lower back by flattening the natural lumbar curvature.
- Spinal Curvature:
- APT: Increases the lumbar lordosis, or curvature of the lower spine.
- PPT: Reduces the lumbar curvature’s natural curve.
- Muscle Imbalances:
- APT: Frequently linked to weak abdominal and gluteal muscles, tight hip flexors, and lower back pain.
- PPT: This may be caused by weakening hip flexor and abdominal flexor muscles as well as tight hamstrings.
- Abdominal Appearance:
- APT: Because of the forward tilt of the pelvis, the abdomen protrudes when they present.
- PPT: The pelvis’s backward inclination may cause the lower abdomen to seem flatter.
- Hip Position:
- APT: The hip joint may appear more flexed.
- PPT: The hip joint may appear more extended.
- Effect on Posture:
- APT: Makes the lower back curvature more pronounced and contributes to a swayback posture.
- PPT: This may be a factor in the rounded or slouched posture of the lower back.
- Common Causes:
- APT: Muscle imbalances, sedentary lifestyles, and extended sitting are typical reasons.
- PPT: Certain structural problems, tight hamstrings, and weak core muscles can all be contributing factors.
- Symptoms:
- APT: This may lead to a variety of musculoskeletal problems and cause hip and back pain.
- PPT: Frequently linked to hamstring tightness, hip discomfort, and lower back pain.
- Treatment Approach:
- APT: Treatment usually consists of strengthening weak muscles (glutes, abdominals) and stretching tight muscles (hip flexors, lower back).
- PPT: Emphasizes strengthening weaker muscles (hip flexors, abdominals) and stretching tight muscles (hamstrings).
- Postural Impact:
- APT: Results in a forward-leaning posture.
- PPT: This may lead to a backward-leaning or rounded posture.
It is essential to understand the distinctions between anterior and posterior pelvic tilt when creating focused treatments.
Diagnose Posterior Pelvic Tilt
A thorough examination by a medical expert, such as a sports medicine specialist, orthopedic physician, or physical therapist, is usually required to diagnose posterior pelvic tilt.
Here are a few typical procedures and techniques utilized throughout the diagnostic process:
Clinical Evaluation:
A comprehensive clinical examination will be carried out by the healthcare professional, which will include a review of the patient’s medical history and a discussion of any symptoms, activities, or lifestyle choices that may exacerbate pelvic tilt.
Physical Assessment:
In order to evaluate posture, spinal alignment, and pelvic position, the medical expert will conduct a physical examination. It is important to watch how the patient stands, sits, and walks.
Tests of Range of Motion:
Tests of range of motion are used to assess the hip joints, spine, and surrounding muscles for flexibility and mobility. Limited range of motion in specific regions could be a sign of imbalances or stiff muscles.
Evaluation of Muscle Length and Strength:
Important muscle groups including the gluteal, hamstring, abdominal, and hip flexors are measured for length and strength. One possible cause of pelvic tilt is weakness or stiffness in certain muscles.
Palpation:
Palpation is a technique the healthcare professional may use to find regions of weak, tense, or painful muscles. Further information on musculoskeletal imbalances can be obtained by palpating particular muscles and bony landmarks.
Imaging studies (if necessary):
While a clinical examination is the main method used to diagnose posterior pelvic tilt, imaging tests like MRIs and X-rays may also be requested in specific circumstances. These investigations can offer comprehensive details on the pelvis, spine, and other musculoskeletal structures’ alignment.
Assessment of Functional Movement:
Examining an individual’s movement patterns while performing particular tasks is part of a functional movement evaluation. This can assist in identifying dysfunctions and compensatory motions that lead to pelvic tilt.
Evaluation of Leg Length Discrepancy:
Verifying whether there are any disparities in leg length is crucial since pelvic tilt might be exacerbated by a notable variation in leg length. This might entail assessing the legs’ length or using specialist equipment.
Treatment of Posterior Pelvic Tilt
A personalized treatment plan can be created by the healthcare professional when posterior pelvic tilt has been diagnosed. Corrective exercises, stretching, and strengthening exercises are sometimes combined with posture instruction as a kind of treatment.
It is important to tackle the fundamental reasons behind the problems, such as imbalanced muscles and bad posture, in order to effectively treat and avoid recurring problems.
Stretching Tight Muscles:
Stretching Your Hamstrings: To increase flexibility and lessen stress in the back of your thighs, concentrate on stretching your hamstrings.
Hip Flexor Stretching: Specifically targeting the iliopsoas, this exercise helps ease stress and improve pelvic alignment.
Strengthening Weak Muscles:
Abdominal Exercises: Building strength in the abdominis and transverse abdominis can assist in supporting the pelvis.
Exercises for the Gluteal Muscles: Focusing on the gluteus maximus in particular might help to maintain appropriate pelvic alignment.
Strengthening the Core:
Exercises that target the obliques and lower back muscles as well as the entire core can help with general stability.
Exercises for Hip Mobility:
In order to address any limitations that could be causing pelvic tilt, including activities that increase hip range of motion and mobility.
Postural Correction:
Become conscious of your posture and work on keeping your pelvis in a neutral position while doing regular tasks. This involves aligning oneself properly when standing, sitting, and walking.
Ergonomic Adjustments:
Modify seating and workplace configurations to encourage proper posture. This could involve utilizing supporting equipment, pillows, or seats that are ergonomic.
Physical Therapy:
Collaborating with a physical therapist might prove advantageous for a workout regimen that is both customized and regimented. A physical therapist is able to recognize certain muscular imbalances and customize workouts to meet the needs of each patient.
Body Awareness and Movement Correction:
To address movement habits that lead to pelvic tilt, put an emphasis on body awareness. This might involve using certain workouts and motions to reactivate muscle memory.
Orthopedic Devices (if recommended):
Orthopedic devices, such as shoe lifts or inserts, may be suggested in some situations to alleviate leg length differences that may be a factor in pelvic tilt.
Avoid Prolonged Sitting:
Minimize the amount of time spent sitting, and if you must, practice good posture and take regular pauses to stand and stretch.
Exercise to Correct Posterior Pelvic Tilt:
It’s common to combine strengthening weak muscles with stretches to address and correct posterior pelvic tilt. The following exercises can aid in the correction of posterior pelvic tilt.
Stretching Exercises:
Hamstring Stretch:

With one leg stretched straight and the other bent such that your foot’s sole presses on the inner thigh of the extended leg, take a seat on the floor.
Maintaining a straight back, bend at the hips and stretch forward toward your toes. After 15 to 30 seconds of holding, swap legs.
Stretch Your Hip Flexors:
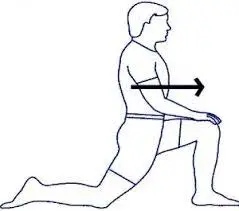
Make a 90-degree angle by bending on one knee and placing the other foot in front of you.
Feel the hip of the kneeling leg extend as you shift your weight forward.
After 15 to 30 sec of hold, perform on the other sides.
Child’s Position:

With your arms out in front of you, begin on your hands and knees and then sit back on your heels.
Reaching your arms forward, ease into the stretch. Hold for a duration of 30 to 1 minute.
Strengthening Exercises:
Pelvic Tilts:
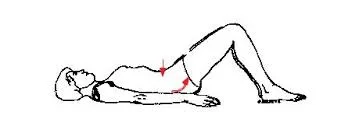
Keep your feet flat on the soft yoga mat and your knees bent in the Supine Position.
Put pressure on your lower back and tighten your abdominal muscles.
After a brief holding, relax.
Ten to fifteen times, repeat.
Bridges:

Keep your feet flat on the soft yoga mat and your knees bent in the Supine Position.
Using your glutes, lift your hips toward the ceiling. After a little period of holding, drop your hips once more.
Do this 12–15 times over.
Leg Lifts:
With your legs straight, lie on your back.
Using your core muscles, raise one leg a few inches off the ground. After a brief moment of holding, release. On the opposite leg, repeat. Do two sets of ten to twelve reps on each leg.
Planks:

Start with your elbows exactly beneath your shoulders in a forearm plank posture.
Engage your core and maintain a straight body alignment from head to heels. As you gain strength, progressively extend the holding time by 20 to 30 seconds.
Dead Bug Exercise:
Lay flat on your back with your legs lifted and your knees bent, your arms reaching upwards.
While maintaining your lower back pressed against the ground, drop one arm and the opposing leg toward the floor. Go back to the beginning and exchange sides. On each side, perform 10–12 repetitions.
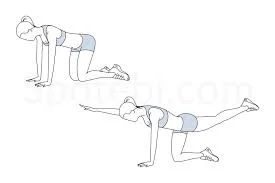
Bird-Dog Exercise:
Place yourself on your hands and knees like you’re on a tabletop.
Stretch one arm and the other leg, maintaining a straight back. Hold for a brief period before switching sides and going back to the beginning position. On each side, perform 10–12 repetitions.
Conclusion
A posterior pelvic tilt is an abnormal tilting of the pelvis backward from its normal position. It results from an imbalance between the muscles of your legs and the muscles of your core, which can be influenced by your everyday posture, anatomy, and movement patterns.
The symptoms might vary, but they can include pain in the back, hamstring tightness, and slouched posture, among others.
Specific muscle-targeting workouts, along with adjustments to sleeping and sitting positions, are frequently part of treatment.





2 Comments