SPINAL TUMOR
INTRODUCTION:
- Spinal tumors are abnormal growth of cells(mass) that develop inside the spinal column, usually causing pain and other symptoms.
- Spine tumors may arise from any of the structures of the spine or the spinal column.
- They may arise in the cervical (neck), thoracic (mid-back) or lumbosacral (low back) regions.
- They may originate in the spinal cord itself, the spinal roots, the dural sac which surrounds the spinal cord, or the vertebrae (bones).
- They may be primary—originating from the spine or spinal cord—or metastatic, originating elsewhere (ie, lung, breast, etc).
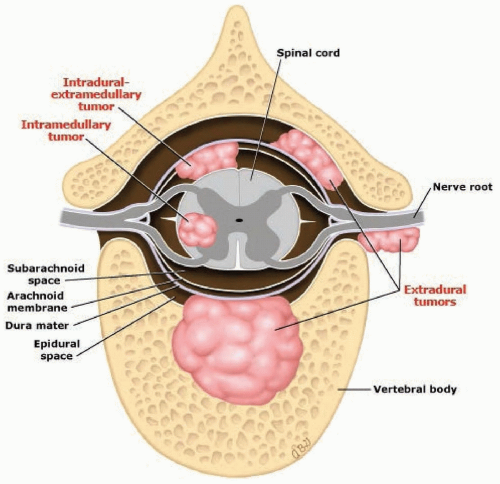
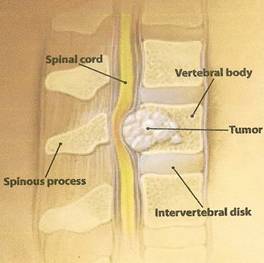
ANATOMY:
- The Spinal Cord starts at the brain stem and goes to the tail bone. It is about as wide as your little finger and extends the length of your back.
- Messages are carried from the spinal cord to and from the brain to the rest of the body.
- The brain and spinal cord are protected by bony structures: the skull and spinal column.
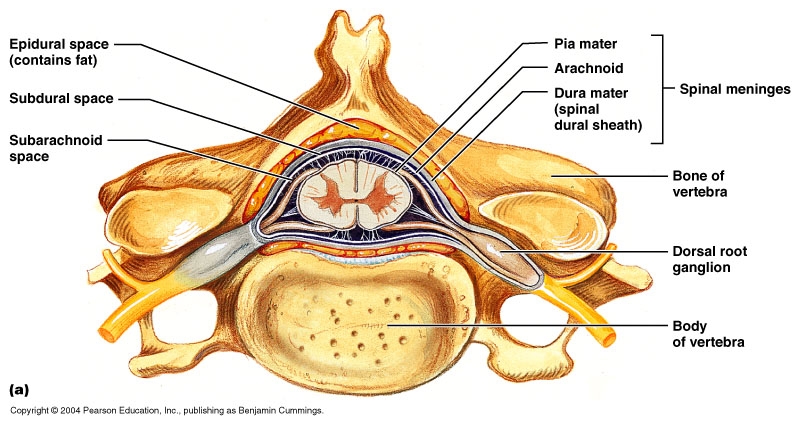
- Meninges are membranes that cover and protect the brain and spinal cord.
- There are three layers of meninges: Dura mater (closest to the bone), Arachnoid loosely around the brain, Pia mater is closely attached to the brain and spinal cord surface.
TYPES:
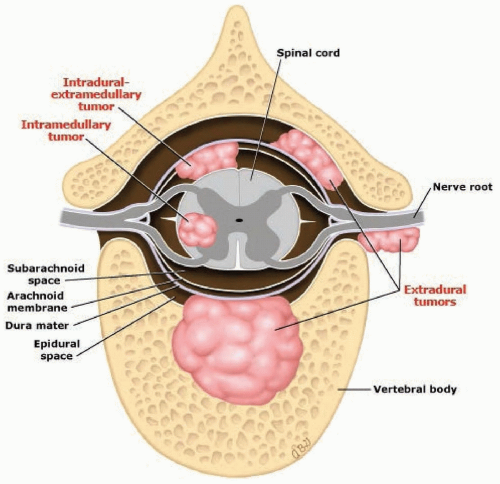
There are three common types of spinal tumors: vertebral column tumors, intradural-extramedullary tumors, and intramedullary tumors.
1.VERTEBRAL COLUMN TUMORS(EXTRADURAL TUMORS):
Primary tumors: These tumors occur in the vertebral column, and grow either from the bone or disc elements of the spine. They typically occur in younger adults. Osteogenic sarcoma (osteosarcoma) is the most common malignant bone tumor. Most primary spinal tumors are quite rare and usually grow slowly.
Metastatic tumors: Most often, spinal tumors metastasize (spread) from cancer in another area of the body.These tumors usually produce pain that does not get better with rest, may be worse at night, and is often accompanied by other signs of serious illness (such as weight loss, fever/chills/shakes, nausea or vomiting).
In women, spinal tumors most frequently spread from cancer that originates in the breast or lung.
In men, spinal tumors most frequently spread from cancer that originates in the prostate or lung.
2. INTRADURAL-EXTRAMEDULLARY TUMORS:
Intradural-Extramedullary (inside the dura) tumors grow within the spinal canal (under the membrane that covers the spinal cord) but outside of the nerves. Usually, these tumors are benign and slow growing. However, they can cause symptoms of pain and weakness.
Most of these spinal tumors are:
Meningiomas that occur in the membranes surrounding the spinal cord and are usually benign but may be malignant. These tumors are more common in middle age and elderly women.
Nerve sheath tumors (schwannomas and neurofibromas) that arise from the nerve roots that come off the spinal cord. Again, this type of tumor is usually benign and slow growing, and it may be years before any neurological problems occur.
These tumors are often meningiomas, Schwannomas, or neurofibromas.
3. INTRAMEDULLARY TUMORS:
Intramedullary tumors grow from inside the spinal cord or inside the individual nerves and often arise from the cells that provide physical support and insulation for the nervous system (glial cells). These tumors occur most often in the cervical spine (neck). They tend to be benign, but surgery to remove the tumor may be difficult.
They are often astrocytomas, ependymomas, or hemangioblastomas. Intramedullary tumors are usually benign.
The two most common types of intramedullary tumors are astrocytomas and ependymomas.
CAUSES:
The cause of most primary spinal tumors is unknown. Some of them may be attributed to exposure to cancer-causing agents. Spinal cord lymphomas, which are cancers that affect lymphocytes (a type of immune cell), are more common in people with compromised immune systems. There appears to be a higher incidence of spinal tumors in particular families, so there is most likely a genetic component.
In a small number of cases, primary tumors may result from the presence of these two genetic diseases:
Neurofibromatosis 2:
In this hereditary disorder, benign tumors may develop in the arachnoid layer of the spinal cord or in the supporting glial cells. However, the more common tumors associated with this disorder affect the nerves related to hearing and can inevitably lead to loss of hearing in one or both ears.
Von Hippel-Lindau disease:
This rare, multi-system disorder is associated with benign blood vessel tumors (hemangioblastomas) in the brain, retina and spinal cord, and with other types of tumors in the kidneys or adrenal glands.
SYMPTOMS:-
The symptoms depend on the location, type of tumor and the patient’s general health. Tumors that have spread to the spine from another site often progress quickly. Primary tumors often progress slowly over weeks to years.
Tumors in the spinal cord usually cause symptoms, sometimes over large portions of the body. Tumors outside the spinal cord may grow for a long time before causing nerve damage.
- Abnormal sensations or loss of sensation, especially in the legs (may be in the knee or ankle, with or without shooting pain down the leg)
Back pain that gets worse over time, is often in the middle or lower back, is usually severe and not relieved by pain medicine, gets worse when lying down or straining (such as during a cough or sneeze), and may extend to the hips or legs - Cold sensation of the legs, cool fingers or hands, or coolness of other areas
- Fecal incontinence
- Inability to keep from leaking urine (urinary incontinence)
- Muscle contractions, twitches or spasms (fasciculations)
- Muscle function loss
- Muscle weakness in the legs that causes falls, makes walking difficult and may get worse
- Metastatic tumors usually produce pain that does not get better with rest, may be worse at night and is often accompanied by other signs of serious illness (such as weight loss, fever, chills, shakes, nausea or vomiting).
DIAGNOSIS:
If your doctor suspects that you may have a spinal tumor, he or she may recommend x-rays of the spine and other diagnostic tests, including:
Computed tomography (CT) scan:
Computed tomography can determine the location of the tumor on the spinal cord, and also can help to detect swelling, bleeding and other associated conditions. The technique creates a cross-sectional view of the body’s tissue and structure using a computer and an X-ray camera that rotates around the body. A dye sometimes is injected into a vein before the scan to help show differences between tissues, which makes it easier to see the tumor.
Magnetic resonance imagining (MRI) scan:
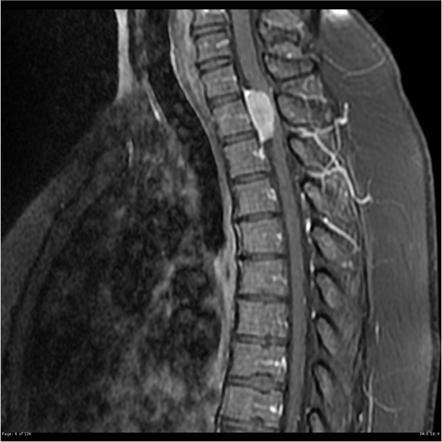
This technique gives a picture of the spinal cord using a powerful magnet, a radio wave transmitter and a computer. It can provide better pictures of tumors near bone than computed tomography.
Myelogram:
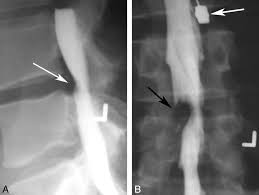
This is a specialized X-ray technique in which a dye that absorbs X-rays is injected into the spinal cord. The dye outlines the spinal cord, but will not pass through the tumor, creating an image with a dark or narrowed area that indicates the tumor’s location. Myelograms are done only occasionally because MRI provides similar information and does not require a spinal injection.
Lumbar puncture:
This procedure removes a sample of cerebrospinal fluid, which is tested for abnormal cells that may suggest the presence of a spinal cord tumor.
Biopsy:
A sample of the tumor may be removed and examined under a microscope to confirm the diagnosis and rule out other conditions. However, it can be difficult to obtain a biopsy of a spinal cord tumor without damaging the spinal cord so careful planning and imaging (such as MRI or CT scan or both) are important. In many cases (especially when a person is known to have cancer already), treatment of the spinal cord tumor may not require a biopsy.
TREATMENT:
MEDICAL:-
There are many different types of drugs and medications used for spinal tumor patients. Your doctor may suggest:
Non-steroidal anti-inflammatory drugs (NSAIDs):
NSAIDs reduce inflammation. Although many of these drugs are available over-the-counter, always discuss use with your doctor before you take an NSAID to avoid a drug interaction.
Corticosteroids or glucocorticosteroids:
These are prescription anti-inflammatory medications such as oral prednisolone, methylprednisolone, and dexamethasone. These are systemic drugs that affect the entire body and are prescribed for a short time.
Opioids:
Also called narcotics, opioids are powerful pain-relieving drugs with a high risk for dependency. These drugs are available by prescription only and include morphine (e.g., Kadian), codeine, and oxycodone (e.g., OyxContin).
Anti-epileptic drugs (e.g., Neurontin) and certain anti-depressant medications (e.g., Cymbalta):
These are effective to treat neuropathic pain. Neuropathic pain is a complex disorder involving nerves that are damaged or dysfunctional.
Osteoporosis drugs (e.g., bisphosphonates):
Osteoporosis drugs interfere with the action of osteoclasts, normal cells that break down bone. When bone breaks down faster than it is replaced (by osteoblasts), bone mineral density is reduced. Treatment using a drug to treat osteoporosis can help preserve bone density.
CHEMOTHERAPY:
Standard treatment for many types of cancer, chemotherapy uses medications to destroy cancer cells or stop them from growing. Your doctor can determine whether chemotherapy might be beneficial for you, either alone or in combination with radiation therapy.
Side effects may include fatigue, nausea, vomiting, increased risk of infection, and hair loss.
RADIATION THERAPY:
This may be used to eliminate the remnants of tumors that remain after surgery, to treat inoperable tumors, or to treat those tumors where surgery is too risky.
Medications may help ease some of the side effects of radiation, such as nausea and vomiting.
Sometimes, your radiation therapy regimen may be adjusted to help minimize the amount of healthy tissue that’s damaged and to make the treatment more effective. Modifications may range from simply changing the dosage of radiation to using sophisticated techniques such as 3-D conformal radiation therapy.
SURGICAL:
Possible Surgical Procedures for Spinal Tumors:
Be assured that your spine surgeon will explain the recommended procedure, including how to prepare for surgery, if hospitalization is necessary, and basically what to expect. Of course, he will answer all of your questions so you can make a fully informed decision.
Depending on the type of spinal tumor and its location, surgery may include one or more of the following procedures:
DECOMPRESSION:
Remove the entire tumor or part of it. Medical terms used include debulk (make smaller), excise (complete removal), or resection (partial removal). These types of procedures decompress or relieve pressure to the spinal cord and nerve roots, thereby helping to reduce pain and other symptoms.
EMBOLIZATION:
An interventional technique, usually performed by a radiologist, slows or cuts off the tumor’s blood supply. Embolization (embolotherapy) causes the tumor to shrink.
KYPHOPLASTY/VERTEBROPLASTY:
Both are minimally invasive surgical procedures that stabilize a fractured vertebra and help relieve pain. A spinal tumor that develops within or invades (metastasize, spread) a vertebra may cause bony compression or fracture. While kyphoplasty and vertebroplasty both involve the injection of surgical bone cement into the fracture to stabilize it, each procedure is different.
Kyphoplasty uses orthopedic balloons that are inserted into the fracture, inflated to create a hole or cavity, and removed before the bone cement is injected.
Vertebroplasty does not use balloons. However, a newer technique combines vertebroplasty with radiofrequency ablation to remove the tumor tissue and create a cavity for the bone cement. Radiofrequency ablation uses radio wave energy to break the tumor’s cellular molecular bonds to help remove tissue and create the cavity.
Both procedures provide immediate fracture stabilization.
RADIOSURGERY(CyberKnife):
This is a non-surgical procedure that delivers precisely targeted radiation to treat certain spine tumors1. Radiosurgery treatment is administered during one or more sessions using high-dose of radiation. This treatment does not immediately remove the tumor like surgery. Rather, the tumor disappears with time.
SPINAL STABILIZATION:
A spinal tumor can cause your spine to become unstable, especially after a decompression procedure (or other surgery) removes bony parts or tissues, such as an intervertebral disc. Spinal instability increases the risk for serious neurologic injury, such as bowel or bladder dysfunction or paralysis.
Spinal stabilization may be included with another surgical procedure to treat your tumor. Stabilization usually involves spinal instrumentation and bone graft. Instrumentation may include implantation of plates, interbody devices, and screws to immediately stabilize the spine. Bone graft, either taken from your body (autograft), donor bone (allograft), or other type, helps to stimulate new bone growth to join the spinal segment together as it heals. Fusion occurs when new bone growth joins vertebrae together.
Spinal decompression and stabilization may be performed as a minimally invasive procedure or by using a more traditional open approach (longer incision, longer recovery time.
COMPLICATIONS OF SPINAL SURGERY:
-pressure sores
-tightness and contracture
-impairments in tone
-osteoporosis
-urinary complications
-respiratory complications
PHYSIOTHERAPY MANAGEMENT:
AIMS ARE:–
1.prevention of all secondary complications as a result of being bed ridden.
2.restoration of functional independency to the maximum possible limit.
3.psychological councelling.
COUNSELING:
- A patient who is depressed cannot cooperate with the therapist which will have a negative effect on the overall rehabilitation of the patient.
- Hence to gain maximum cooperation from the patient the therapist should give appropriate psychological counseling that will enable the patient to come out of state of depression.
- The patient needs to be told regarding his condition but at the same time the therapist should try and highlight the positive features contained in the patient even at this stage which in turn will inspire the patient to look at his future in a more convincing manner.
- However one should not give false hopes to the patient as the expectation of patient may be too high.
MAINTAINING PASSIVE AND ACTIVE RANGE OF MOTION:
- The patient’s lower limb should be moved passively by the therapist through full range of motion if the patient is not able to perform the movement actively.
- Wherever the patient is likely to put his active efforts to perform the movement, the therapist should encourage it as this will not only maintain the active range but will also help the patient to maintain the properties in his muscles.
- Passive movements need to be given every two hourly hence the patient’s relative attending him should be taught the correct way of handling and giving passive movement without producing undesired movement of the spine.
- Passive movements helps to maintain the normal physiological length of soft tissues and prevents tightness.
- It maintains the memory of the movement pattern in the brain which may help in the later stages of recovery.
- Passive movements also help in reducing spasticity if given in a gentle, slow and rhythmic manner.
MAINTENANCE OF BRONCHIAL HYGIENE:
- As the patient is totally bedridden it leads to deconditioning of the respiratory system.
- Moreover in higher cord lesion due to respiratory muscles weakness, the patient needs ventilatory support which further increases the chances of lung infection.
- Hence proper lung hygiene should be maintained by given proper positioning, nebulization and regular suctioning.
- If the patient is not on ventilatory support then he should be taught breathing exercises and encouraged doing it every hour.
CARE OF SKIN:-
Due to constant immobilization the patient can develop pressure sores at certain parts of the body.
Certain areas are more susceptible to develop pressure sores like sacrum, heel, lateral aspect of the knee, occiput, etc. Hence prevention and treatment of pressure sores are very important.
Prevention of pressure sores is achieved by undertaking the following measures:
-The patient’s attendant as well as the nursing staff should be advised to keep changing the position of the patient every 2 hourly to avoid increase weight bearing pressure on certain body parts especially where the subcutaneous fat is very less.
-Good skin hygiene is maintained by given regular sponge bath and applying talcum powder.
As patient with urinary or fecal incontinence are prone to soil the skin around the genital area it is very susceptible to cause skin infection and even urinary tract infection hence more emphasize should be given to these areas to maintain hygiene.
-Bed linen is kept dry and free of creases.
-Beds that bring about a more uniform distribution of body weight should be given. Thus waterbed or airbed is used to equalize the pressure on patient’s body and to prevent areas of increase pressure.
-Gently massaging the pressure susceptible areas also increases the circulation in that areas preventing the chances of skin infection.
In case, in spite of the entire preventive measures if the pressure sores do develop then it should be treated at the early stage and the wound should be prevented from getting infected so that the rate of healing is faster. This can be achieved by the following:
• Regular dressing of wound
• Cryotherapy around the wound area to increase circulation
• Infrared therapy over the wound also increases the blood supply
to the part and thus helps in faster recovery
• If the wound is infected then UVR can be given
• Laser therapy at appropriate dose can be very effective in healing
the sores
• Direct current given at the edges of the sores helps in healing
ACTIVE EXERCISE:
As soon as the patient shows signs of active contraction of muscles and active participation, all the exercises that needs active cooperation of the patient should be started. These exercises are essential to make the patient functionally independent.
The common exercises which are incorporated into the treatment program consist of Mat exercises, strengthening techniques, weight-bearing exercises, the normalizing tone in the lower limb, gait training, and Transfer activities.
-to reduce spasticity:
Spasticity in the muscles can be reduced by the following methods:
• Gentle rhythmic passive movement.
• Sustained gradual stretching either manually or by using splints.
• Prolonged icing over the spastic muscle bulk for about 15 to 20 minutes. Studies have shown that prolonged icing and sustained stretching are equally effective in inhibiting spasticity.
• Faradic stimulation to the weak antagonist muscles can reduce the spasticity of the agonist muscle by the principle of reciprocal inhibition. However, this should be given only when the antagonist muscle is not active voluntarily.
• Reflex inhibiting postures or pattern. Infact, almost all the exercises given in the stage of spasticity are on the basis of reflex inhibiting pattern and postures.
• Biofeedback : This can be used to relax the spastic muscle as well as to activate its antagonist.
MAT EXERCISE:
To prepare the patient for gait training and erect posture mat exercises play a very important role.
These exercises consist of those activities that may help the patient to achieve some functional independency. The activities consist of turning to each sides, rolling and bridging. Similarly in prone position the patient may be given activities such as coming on to forearms, coming on to extended forearms, quadripedal position with the help of some external support, kneeling with support, half kneeling, etc
BRIDGING:

Lie on your back with both knees about 90 Degree.
Then push your feet into the floor, squeeze or tighten your buttocks, and lift your hips off the floor until the shoulders, hips, and knees are all in a straight line.
Hold for about 5 sec, and then slowly lower your hips back down to the floor and rest for up to TEN seconds.
Repeat 10 times.
FOREARM SUPPORT:-

Lie in prone position(face down)
Put forearm at 90 degree with arm and stretch your body up without lifting elbow from floor.
Hold this position for 10-15 sec and then relax.
Repeat this for 10 times.
PRONE LYING ON ARM:-

– Once you’ve mastered the half cobra pose, you can increase the difficulty by moving to the advanced version of this stretch. Begin this exercise by lying on your stomach in the prone position (lying facing down) and slowly press up on your hands while keeping your pelvis in contact with the floor and lower back relaxed.
– Hold the prop-up position for 10 seconds. Aim for 10 repetitions of this stretch.
– Eventually try to hold this pose for longer if it feels good (20-30 seconds).
QUADRUPED POSITION WITH EXTERNAL SUPPORT:-
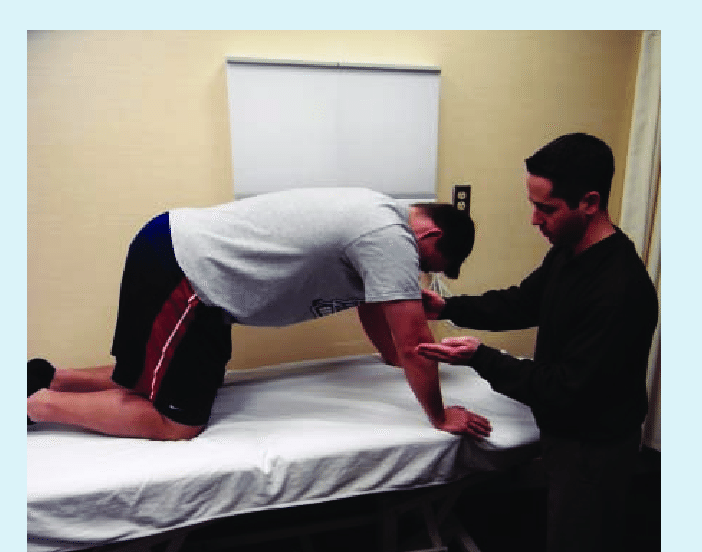
KNEELING WITH SUPPORT:-

HALF KNEELING:-

STRENGTHENING EXERCISE:-
- These consist of exercises to strengthen the lower limb muscles in case of lower motor neuron type of palsy.
- Strengthening of the upper limb is essential as this will help the patient to enable efficiency in activities like transferring, use of walking aids like crutch, and also helps in over all functional rehabilitation.
- Strengthening of trunk muscles is essential for better trunk control and stability which will help in better balancing in sitting or standing.
• Use of tilt table:
In the initial stages when there is no trunk stability patient can be trained for weight bearing on lower limbs by using tilt table. In this the patient’s trunk and the lower limbs are strapped to the tilt table and then the table is tilted such that the patient is in erect position.
• Transfer activities:
- To make the patient independent in ADL, it is necessary to train him to use the wheelchair and transfer from and to wheelchair.
- Easy ways of transfer from bed to wheelchair from wheelchair to low stool and from low stool to floor and back to wheel chair should be taught to patient.
- The patient also should be trained for balance in sitting position if his trunk muscles are also affected.
- Patient should also be taught various ways of locomotion in emergency situation like shuffling in sitting position, semicrawling in prone position with the help of weight bearing on the forearm.
• Gait training:
A paraplegic patient can be made to ambulate with the help of crutches and calipers. There are various types of paraplegic gait that can be taught with the assistance of axillary crutches like shuffling gait, dragging gait, and swing gait.
However, walking should be trained in a gradual manner. The lower limbs are supported with appropriate orthoses and the patient is made to stand in the parallel bar.
The patient is advised to do hyperextension at the hips and trunk to maintain erect posture and balance. Hyperextension of the hip locks the hip with the help of ischiofemoral ligament and thus provides stability.
Once the patient is confident in standing gait training is started by instructing the patient to lift one leg and take weight on other extremity. Stepping forward is taught next and the physiotherapist progresses to walking in parallel bars. After this patient is made to walkout of the parallel bar with the help of walker.
Depending on the trunk stability and confidence of the patient progression can be made to axillary crutches. Elbow crutches or canes can be given only if the upper limb musculature becomes quite strong to weight bear efficiently and within the safety limit of the patient.
Even if the patient is not going to be a community walker, it is important to give him gait training so that he can achieve some independency in activities of daily living (ADL) and to maintain his self-esteem. Weight bearing on the lower limbs in erect posture also acts to slow down the process of osteoporosis and prevent tightness.
• Use of orthosis or appliances:
Lower limb orthosis or gaiter may be used depending on the muscular status in the lower limbs.