Salter-Harris Fracture
Table of Contents
What is a Salter-Harris Fracture?
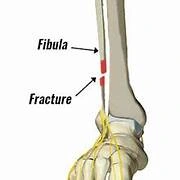
A Salter-Harris fracture is a fracture in a child’s bone’s growth plate. A growth plate is a layer of developing tissue near the ends of a child’s bones. It’s critical to get this condition diagnosed because it can stunt a child’s growth.
Salter-Harris fractures can occur in any long bone, from the legs to the fingers. Please continue reading to learn more about Salter-Harris fractures and how to treat, diagnose, and prevent them.
Salter-Harris fractures are fractures that only occur in children’s developing bones. They are pretty common, accounting for 15% to 30% of all paediatric fractures.
Trauma or overuse usually causes growth plate fractures on the wrist, fingers, and lower leg. As a result, child pitchers and gymnasts are more likely to suffer from these fractures. Boys are also more likely to develop this condition because they participate in more high-risk physical activities.
It is critical to have these fractures diagnosed as soon as possible. They can stunt a child’s growth by causing damage to the growth plates at the ends of their bones. Growth plates are delicate cartilage discs found on the ends of children’s long bones where growth occurs.
If your child’s limbs, wrists, or fingers are not treated correctly or on time, they may become unequal in length or crooked. If you suspect your child has a fracture, take them to the doctor as soon as possible. If there is a fracture, they should see an orthopedist within five to seven days of the injury for the best outcome.
Classification of Salter-Harris Fracture
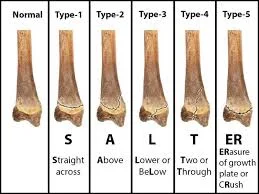
Five types of Salter-Harris fractures are recognized:
A growth plate fracture is referred to as type I. The fracture line goes through the growth plate or the physis. The longitudinal force that separates the epiphysis from the metaphysis through the physis causes type I fractures.
Type II gets into both the growth plate and the metaphysis. The epiphysis is not involved in this. Out of all the Salter-Harris fractures, this is the most typical.
Type III fractures are intra-articular fractures that go through the growth plate and epiphysis. When this happens, it usually happens at the distal end of the tibia. This type of fracture may form two epiphyseal segments if it extends the entire length of the physis. Because the epiphysis is involved, articular cartilage damage is possible. A Tillaux fracture of the ankle, which is a fracture of the anterolateral aspect of the growth plate and epiphysis, is one example of this
Type IV can be found in the epiphysis, growth plate, and metaphysis.
Type V is a growth plate crushing or compression injury that affects the growth plate. The force travels through the epiphysis and physis, potentially disrupting the germinal matrix, hypertrophic region, and vascular supply.
Though Harris-Salter V fractures are extremely rare, they can occur as a result of electric shock, frostbite, or irradiation. Because this fracture pattern is usually the result of a severe injury, the prognosis is usually poor, resulting in bone growth arrest
Type VI-Type IX fractures are also possible, but they are uncommon.
Causes of Salter-Harris Fracture
Salter-Harris fractures are usually the result of a traumatic event, such as a fall or a car accident. Repetitive pressure on the long bone during sports or other high-impact activities can also cause bone injury over time.
Types I through III are typically caused by a rotating or twisting force, such as twisting the leg during a fall. Types IV and V, on the other hand, are typically caused by compression or a crushing force. Non-traumatic causes of type V fractures include bone infection (i.e., osteomyelitis) and growth plate death (i.e., epiphyseal aseptic necrosis).
Mechanism of injury
Salter-Harris fractures are frequently the result of sports-related injuries. Still, they have also been linked to child abuse, genetics, injury from extreme colds, radiation and medications, neurological disorders, and metabolic diseases, all of which affect the growth plate.
Sports account for roughly one-third of Salter-Harris fractures, with recreational activities accounting for the other half. They can be caused by a single injury or by repetitive stresses on the upper and lower extremities.
Symptoms of Salter-Harris Fracture
If your child presents the following symptoms, they may have a Salter-Harris fracture:
- Tenderness in the suspected fracture area
- Swelling in the suspected fracture area
- Impossibility of putting weight on the affected area
- Impossibility of moving the affected area
A Salter-Harris fracture does not always result in a crooked or deformed joint. Take your child to the doctor if they are complaining of severe pain or pain that is not going away, or if they are not using their joint or bearing weight on their limb.
Diagnosis
A clinician will typically conduct a medical evaluation for diagnosis, which will include a review of the event’s history, and symptoms, and a physical examination of the area. The medical evaluation is usually followed by an X-ray.
Type I fractures can be seen on an X-ray as a slight separation of the epiphysis from the bone, but these fractures are usually not visible because they affect the cartilage rather than the bone. As a result, a type I fracture diagnosis is frequently based solely on symptoms and medical evaluation.
Type V fractures are frequently overlooked because they only involve injury to the growth plate rather than physical breakage. When there is evidence of growth arrest, these fractures are usually detected during follow-up visits.
Treatment of Salter-Harris Fracture
The initial focus of treatment is frequently on controlling swelling and pain. Elevating the affected limb and icing the area may help to reduce swelling. When necessary, pain can be treated with medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or local anaesthetic injections. Rest is frequently advised to aid in recovery.
Further treatment is usually determined by the type of fracture and additional orthopaedic evaluation. Type I and II fractures are frequently treated with a closed reduction, which involves repositioning a bone without surgery. Following bone realignment, a cast or splint is typically applied to keep the bone stable so that it can heal properly.
Children who suffer from these fractures usually recover with little impact on bone growth. Type III and IV fractures, on the other hand, usually necessitate a surgical procedure known as an open reduction to set the bone back into place, and internal fixation, in which metal is used to stabilize the bone, is frequently required. Because type V is frequently diagnosed several weeks after the initial injury, Treatment options vary greatly depending on the severity of the bone deformity or arrest.
A clinician should typically re-examine the fracture seven to ten days after treatment begins to ensure the bones are healing properly and to assess for any complications. A follow-up X-ray may be recommended in 6 to 12 months to ensure continued bone growth.
Rehabilitation
Physical therapy may be recommended for the patient to regain range of motion, strength, and function. Physical therapy should focus on assisting the patient with adhering to immobilization or weight-bearing protocols in the acute phase following injury or surgical management.
Controlled range of motion exercises and light strength training can be used. Progressive strengthening, range of motion, balance, and proprioception exercises should be implemented after the growth plate has healed sufficiently. Advanced rehabilitation for young athletes should include sport-specific exercises and drills.
Complication
The vast majority of physical injuries heal quickly and completely. Growth disruption or arrest may occur in a minority of cases, resulting in deformity and impaired function.
Physical growth can be affected by:
- Necrosis of the arteries
- Crushing directly (Salter-Harris type V)
- The growth of a bony bar
- Non-union
- Hyperaemia
Prevention
The majority of Salter-Harris fractures are caused by childhood trauma, such as falling off a bike or being pushed down during a sports game.
You can protect your child from Salter-Harris fractures by doing the following:
Encourage your child to take more breaks when playing sports.
Monitoring your child’s athletic training during periods of rapid growth, when your child is more likely to develop growth plate fractures.
You should also encourage your child to prioritize skill development over competition and success. As a result, your child will be less likely to be involved in an accident that could result in Salter-Harris fractures.
Summary
A Salter-Harris fracture is a fracture in a child’s bone’s growth plate, which can stunt a child’s growth. These fractures are common in children, accounting for 15% to 30% of all paediatric fractures. Trauma or overuse usually causes growth plate fractures on the wrist, fingers, and lower leg, making child pitchers and gymnasts more likely to suffer from these fractures. Boys are also more likely to develop this condition due to their participation in high-risk physical activities.
There are five types of Salter-Harris fractures: Type I, Type II, Type III, Type IV, Type V, and Type VI-Type IX. Type I fractures occur when the fracture line goes through the growth plate or the physis, while Type II gets into both the growth plate and the metaphysis. Type III fractures are intra-articular fractures that go through the growth plate and epiphysis, often at the distal end of the tibia. Type IV can be found in the epiphysis, growth plate, and metaphysis. Type V fractures are extremely rare but can occur as a result of electric shock, frostbite, or irradiation.
Salter-Harris fractures are often caused by traumatic events, repetitive pressure during sports, genetics, radiation, medications, neurological disorders, and metabolic diseases. Sports account for roughly one-third of Salter-Harris fractures, with recreational activities accounting for the other half.
Symptoms of a Salter-Harris fracture include tenderness, swelling, the impossibility of putting weight on the affected area, and the impossibility of moving the affected area. Diagnosis involves a medical evaluation, X-ray, and follow-up visits. Treatment focuses on controlling swelling and pain, with rest advised for recovery. Type III and IV fractures require surgery and internal fixation.
Rehabilitation may involve physical therapy to regain range of motion, strength, and function. This should focus on adhering to immobilization or weight-bearing protocols in the acute phase following injury or surgical management.
FAQs
A Salter-Harris fracture is a fracture in a child’s bone’s growth plate. A growth plate is a layer of developing tissue near the ends of a child’s bones. It is critical to diagnose this condition because it can have an impact on a child’s growth.
Type II Salter-Harris fractures are the most common and involve a bone fracture through the growth plate and part of the metaphysis. There are four additional, rare types of Salter-Harris fractures in addition to the five common types.
A Salter-Harris type 1 fracture is the most common type of growth plate fracture. The bone on the outside of the ankle is known as the distal fibula. This injury usually occurs as a result of inverting or rolling the ankle.
Healing typically takes 4-6 weeks, after which time your child can resume sports and activities.
Prescription pain relievers may be administered.
Until further treatment is received, a cast or splint may be used to help prevent movement in the injured area.
Certain Salter-Harris fractures may necessitate surgery to repair.
References:
- What Is a Salter-Harris Fracture? (2021, May 21). WebMD. https://www.webmd.com/children/what-is-salter-harris-fracture
- Salter-Harris Fractures. (n.d.). Physiopedia. https://www.physio-pedia.com/Salter-Harris_Fractures
- Osmosis – Salter-Harris Fracture: What Is It, Types, Treatment, and More. (n.d.). Osmosis. https://www.osmosis.org/answers/salter-harris-fracture
- Levine, R. H. (n.d.). [Figure, Salter-Harris, Types I-V. Contributed by Scott Dulebohn, MD] – StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK430688/figure/article-28713.image.f1/
- Fracture Education : Physeal (growth plate) injuries. (n.d.). https://www.rch.org.au/fracture-education/growth_plate_injuries/physeal_growth_plate_injuries/