Soleus Strain
Table of Contents
What is a Soleus Muscle Strain?
A soleus strain is a type of muscle injury that specifically affects the soleus muscle, which is located in the calf. The soleus is one of the two muscles that make up the calf, with the other being the larger gastrocnemius muscle.
When loads from activity cause damage to muscle fibres, a strain in the muscle occurs. Soleus strain is frequently associated with a gradual onset of pain that frequently lacks a clear mechanism of injury (MOI).
The intramuscular aponeurosis restricted sensory innervation could be the cause of this. When a particular MOI is found, steady-state running seems to be the most frequent cause of harm.
Anatomy of Soleus muscle and Triceps surae
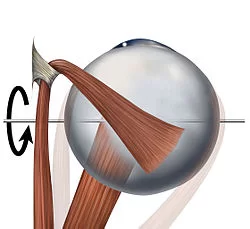
Soleus muscle in the body is situated in the leg’s superficial posterior compartment Located deep to the gastrocnemius muscle, the soleus is a potent lower limb muscle. It forms the triceps surae, or calf muscle, along with the gastrocnemius and plantaris muscles. It is multipennate and extends from the back of the knee to the ankle.
Among the calf muscles, the soleus has the largest physiological cross-sectional area (CSA), and it is believed to supply up to 80% of the force produced by the triceps surae.

Origin of soleus muscle
The top third of the fibula shaft and the posterior surface of the head; the Tendinous arch connecting the tibia and fibula, located in the middle third of the tibia’s medial border.
Insertion of soleus muscle
The posterior surface of the calcaneus through the tendon of Achilles
The action of soleus muscle
Ankle plantar flexion of the foot; Reversed origin insertion action: the calcaneus becomes the muscle’s fixed origin when standing; Limiting forward sway, the soleus muscle stabilizes the tibia on the calcaneus.
Nerve supply of soleus muscle
Tibial nerve, S1, S2, L4, L5, and The intramuscular aponeurosis have no sensory supply.
Synergists of soleus muscle
Flexor hallucis longus, Flexor digitorum longus, Peroneus longus and Brevis, Plantaris, Gastrocnemius, and Tibialis posterior.
Antagonist of soleus muscle
the tibialis anterior
Blood supply of soleus muscle
The posterior tibial artery supplies blood distally and the peroneal artery proximally to the soleus muscle; A mixed blood supply supplies muscles; Popliteal, posterior Tibial, and peroneal vascular pedicles supply the proximal muscle, peroneal pedicles supply the distal lateral belly, and segmental posterior Tibial pedicles supply the distal medial belly of the soleus.
Muscle can be transposed medially or laterally to cover defects in the middle third of the leg after the distal pedicles of the posterior tibial artery are ligated and based on the proximal pedicles of the posterior tibial and peroneal arteries; The popliteal vessels give rise to the proximal vasculature, which can consistently transport all muscle fibres except the distal 4 to 5 cm;
The soleus’s intramuscular vasculature splits into a bipenniform segmental pattern. This vascular pattern allows for the use of either half of the soleus muscle, maintaining the integrity of the hemisoleus muscle.
Function of soleus muscle
Soleus serves two main purposes:
- To function as bone
It is a strong plantar flexor and plays a significant role in running, walking, and dancing, along with other calf muscles. In addition, it is a significant postural muscle that prevents the body from collapsing at the ankle when in a stance.
The gastrocnemius is essentially inactive and the soleus bears almost all of the weight during the seated calf raise (knees flexed about 90º). The gastrocnemius is preferentially activated in the eccentric phase of moderate force, while the soleus is preferentially activated in the concentric phase. Slow twitch fibres make up the majority of the muscle tissue in the human soleus, though this percentage can vary from 60% to 100%.
2. Function as muscle pump
As the venous circulatory system passes through the muscle tissue, the soleal pump helps with the venous return from the periphery to the heart when in an upright position.
Causes of soleus strain
Bi-articular muscles like the rectus femoris, gastrocnemius, and hamstrings are the most frequently sprained muscles. Consequently, a gastrocnemius strain is frequently meant when we speak of a “calf strain”.
These long, biarticular muscles are subjected to high internal forces and quick changes in muscle length and contraction mode during athletic activities like sprinting, which increases the risk of strain. Despite this, it has also been noted that calf muscle strains can happen during regular daily activities as well as slow-lengthening muscle actions like those done by ballet dancers. Injuries from calf muscle strains can occur in a variety of sports, including rugby, football, tennis, athletics, and dancing. In football, 92% of injuries are to the muscles, and 13% are to the calves.
Risk factors of soleus strain
The biggest risk factors for calf strain is player age and history of calf strains or other leg injuries; player attributes like height, weight, sex, and side dominance are unlikely to be linked to calf muscle injuries.
One explanation for age-related tissue changes could be that skeletal muscle quality and function gradually deteriorate with age, leading to neuromuscular maladaptation that limit muscle force and contraction rate. Sometimes the repaired tissue performs less well than it should.
This implies that prior muscle injury may be associated with a higher risk of subsequent injury because optimal tissue functionality is protective. Previous calf, hamstring, quadriceps, adductor, and knee injuries have been found to be risk factors for another calf injury
Symptoms of Soleus Strain
Distinguishing between muscle strains within the calf complex is crucial for developing an accurate prognosis, and a suitable treatment plan, and preventing further injuries.
- A torn calf muscle may result in:
- Have trouble standing on tiptoe or tensing your calf muscles.
- Aches in your muscles when you point your toes or flex your ankle.
- Inability to bend your knee.
- A pop or snap sensation in your leg.
- A sudden ache in your lower leg’s back.
- Enlargement of the calf muscle.
- Your calf muscle is bruised.
The majority of people who have pulled calf muscles say that they were unable to resume their activity right after the injury. The gastrocnemius muscle’s medial head is where calf strains are most frequently found. The patient experiences an abrupt onset of pain in the calf and frequently describes hearing or feeling a “pop” in the medial aspect of the posterior calf, or they feel as though they’ve been kicked in the back of their leg. Usually, during the next 24 hours, significant pain and swelling occur. Since a middle-aged tennis player abruptly extended their knee in the classic presentation, strains in the gastrocnemius are also known as “tennis legs.”
When the knee is bent, damage is sustained to the soleus muscle. The most frequent kinds of injuries to the soleus muscle are strains of the proximal medial musculotendinous junction. Soleus has a lower risk of injury than gastrocnemius. It mostly consists of type slow-twitch muscle fibres and only crosses the ankle. In addition, compared to gastrocnemius injuries, soleus strains typically present clinically as sub-acute injuries rather than as dramatic ones. Middle-aged patients who are physically active or in poor condition are often the ones who suffer from this condition.
The symptoms will probably manifest similarly to a gastrocnemius strain, but the pain may feel deeper to the patient and be a little more distal. Because soleus strains are often mistaken for thrombophlebitis, injuries to the soleus muscle may go unreported.
Because soleus strains are sometimes confused with gastrocnemius strains or misdiagnosed as thrombophlebitis, soleus muscle injuries may go unreported. A soleus strain hurts when the calf muscle is contracted or when pressure is applied to the Achilles tendon, either higher up in the calf muscle or about 4 cm above the point where the tendon insertions into the heel bone. Walking on tip-toe and stretching the tendon will exacerbate the pain.
Diagnosis of soleus strain
A soleus injury can be difficult to diagnose solely by physical examination. For this reason, an MRI or ultrasound are usually used by medical professionals to confirm this diagnosis.
Although ultrasounds are not as effective in identifying this kind of injury, physicians may still use them. A person’s symptoms will also be inquired about by a doctor. A soleus strain will hurt someone when: Dorsiflexion is the lifting of the foot by pointing the toes upward, stretching the foot, or walking on tiptoe, performed by the calf muscles pressing on the Achilles tendon. The physician will diagnose the soleus injury and categorize it as a grade 1, 2, or 3 strain.
First-grade soleus strain
A person suffering from a grade 1 strain could encounter: Sharpness or pain during the beginning of an activity, followed by mild discomfort or no pain tightness, sore muscles or aches after an activity
Second-grade soleus strain
The following signs could indicate a grade 2 soleus strain: Sharpness or pain during a task that prevents you from finishing it Walking pain following the activity bruises or discolorations
Third-grade soleus strain
Grade 3 soleus strain symptoms include: Severe discomfort, incapacity to engage in physical activity, notable bruises or discolorations, and swelling
Differential diagnosis of soleus strain
Shin splints
Which occurs due to medial tibial stress tension syndrome
Achilles tendinopathy
Foot fasciitis
Joints and/or muscle sprains as a result of the ankle’s decreased range of motion.
The following section discusses additional sports-related lower limb injuries that share the same symptoms and course of care as a calf strain.
CECS (Chronic exertional compartment syndrome)
it stands for chronic exertional compartment syndrome. During training, CECS initially causes mild pain, which may go away later. Later stages are characterized by earlier onset, increased pain, longer duration, and the need to stop activity. Leg cramps, paraesthesia, numbness, and weakness are common complaints. Exercise-induced increases in intramuscular blood flow lead to compartmental pressure, capillary compression, and ischemia, which is the cause of CECS.
The gastrocnemius, soleus, and plantaris are the three distinct muscles that make up the calf muscle.
The calf muscle that is most frequently strained is the gastrocnemius. The gastrocnemius, which is situated behind the knee as well, is bigger than the soleus.
While strains in the gastrocnemius are more likely to occur suddenly, injuries to the soleus muscle are usually the consequence of overuse. Often referred to as tennis leg, this strain is frequently brought on by rapid motions like jumping or sprinting.
Plantaris injuries
Plantaris injuries are uncommon because the muscle is underutilized and well-protected by other muscles. As a matter of fact, this muscle is not necessary for the body to function, and 7–20 percent of people may not have it. An MRI is used by physicians to identify a plantaris strain.
The tendinitis
Tendinitis is the medical term for tendon inflammation. Muscles and bones are joined by thick cords called tendons. It can be difficult when they become angry.
Sporadic claudication
Walking-related pain in the calf, thigh, or buttock muscles is a hallmark of the early stages of ischemic leg pain. Walking improves blood flow to the muscles, facilitating increased oxygen uptake and toxin removal. If the arteries are unhealthy and the muscles do not get the extra blood they require, toxins build up in the muscles and cause pain and weakness. In the early stages of the disease, this occurs at a significant distance, like a half-mile. A person can walk a shorter distance—for instance, 100 yards—before feeling pain if the artery narrowing gets worse. Eventually, leg pain for some patients prevents them from moving more than a few yards.
A common sports-related injury that most commonly affects middle-aged individuals is a tennis leg. In the middle of your calf, you might experience an abrupt, intense (acute) pain. You might also hear or feel something snap.
Usually caused by a rip in the gastrocnemius muscle, it can also happen as a result of a build-up of fluid between the gastrocnemius and soleus muscles. Ten percent of patients with tennis leg symptoms are actually suffering from a blood clot, not a calf strain. This is the reason a precise diagnosis is so crucial.
When to see a Doctor?
who exhibit signs of a gastrocnemius or soleus strain may be suffering from deep vein thrombosis (DVT). DVT is a type of leg blood clot that, if it spreads to the lungs, can result in serious complications. If a person experiences any of the following calf symptoms, they should see a doctor right away as these could be signs of DVT: extreme, acute pain. considerable soreness bruising, discolouration, swelling, or a noticeable defect redness.
Acquiring an accurate diagnosis and creating a customized treatment plan will expedite the healing process and avert re-injury. In addition, if the strain is severe, a doctor might suggest physiotherapy for rehabilitation.
Treatment of Soleus Strain
Immediate soleus strain
The RICE method is a common first treatment recommended by doctors for injuries and strains of the muscles. By the RICE method, we mean:
Rest
Try not to move the sore muscle as much as you can. Get enough rest so that your body can heal itself.
Ice
To relieve pain and inflammation, apply ice to the afflicted area. To prevent ice burns to the skin, cover the ice with a thin towel.
Compression
To reduce swelling, wrap the afflicted area with a medical bandage. Avoid wrapping the leg too tightly as this may stop the blood supply. If the area appears blue, feels cold, or is tingly, loosen the bandage.
Elevation
To lessen pain and bruises, try to keep the leg above the heart. Over-the-counter (OTC) pain relievers: To relieve pain and lessen inflammation, people can take an OTC pain reliever like ibuprofen. The healing period for a pulled calf muscle can range from several weeks to months, depending on how severe the injury is. In order to treat a severely strained or torn calf muscle, a doctor might advise surgery. Damage to surrounding blood vessels from muscle injuries may result in localized bleeding beneath the skin. Blood clots or hematomas can develop from blood cells that gather in muscle tissue. A hematoma can be treated by a physician with aspiration, a minimally invasive procedure.
Operative treatment of Soleus Strain
Nonoperative therapy is the cornerstone of care. Operative management is rarely necessary, but in the most extreme cases—complete grade-III ruptures, contractures, fibrosis, significant hematoma, acute compartment syndrome, or myositis ossificans—it might be taken into consideration. When there is a total tear in the muscles, standing on the metatarsal heads becomes impossible.
Physiotherapy treatment of soleus strain
Rest and giving the injury enough time to heal are the main treatments for calf strains, but in more serious situations, surgery may be required.
Gentle passive stretching, isometric exercises, and concentric exercises are all part of the conservative treatment. Massage and electrotherapy can be used in the later stages.
Goals of the first course of treatment: in order to reduce bleeding and avoid complications.
Protocols for managing soft tissue injuries ought to be initiated as soon as the damage happens. The concepts of PEACE and LOVE ought to be implemented. Additional physiotherapy techniques include: If it is feasible, the leg can be elevated and taped or wrapped in a compressive garment.
The use of NSAIDs after significant bleeding must be carefully monitored because they have an anti-platelet effect that can exacerbate bleeding, and applying them too soon can also Maintain plantar flexor range of motion requires mild passive stretching exercises that don’t cause pain. In the later phases, after the inflammation has subsided, a low-load static stretch and the application of superficial heat together increase muscle flexibility.
Along with mild exercises for the injured muscle, isotonic exercises for the antagonists tibialis anterior and peronei are advised. In the initial days after an injury, light activity within pain tolerance will aid in the promotion of healing.
Low-heeled shoes are advised to promote a better heel-toe gait.
Gentle passive stretching can be replaced with active stretches in both the straightened knee position (gastrocnemius) and the flexed knee position (soleus) once the calf muscles can be fully extended without pain.
- Gradual strengthening or loading training of the calf muscles should be preferred in order to have a total recovery. The sooner loading training is commenced the more rapid recovery expected.
- Back to sport and a specific type of plyometric training should be commenced before full-back to sport.

Strains may cause long-lasting pain, despite adequate early exercise. Treatment outcome is guaranteed when: pain is gone, the calf muscle of the body can be fully extended, strength is back to normal life, knee and ankle range of motion are normal, and excessive tenderness has gone.
Tapping is used to treat soleus strain.
Soleus stretching different method
Soleus muscle stretching: You can relieve pain and tightness in your muscles by stretching.
Foam roller soleus stretch

Take a seat on the ground and extend your legs in front of you. Position a foam roller underneath the leg’s targeted calf area.
Place the leg that is in contact with the foam roller on top of the other leg. Fully relax the lower leg. Use the upper leg to exert downward pressure. Make side-to-side movements with the lower leg. Ensure that the entire area of the calf is covered. Keep going for two minutes.
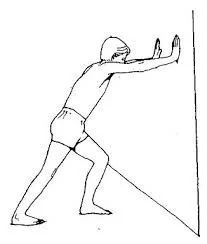
Wall lunges

Put yourself in a lunge posture. (The side that will be stretched will be the leg in front.) For support, place both hands against the wall. Make sure your front side foot is facing the front side Extend your knee as far forward as you can. Remember to maintain your heel’s contact with the ground. Put as much weight as possible on the front leg. For at least thirty seconds, hold.
Progression: Position a tiny block beneath the leading leg’s forefoot.
Standing stretch of soleus muscle
Get to your feet. Put one leg on the forward side of you and the other behind you. (The side that is stretched will be the leg at the back.) Maintain the rear leg’s foot pointed forward. Put more weight on the back leg of your body. Permit the rear leg’s knee to travel as far forward as it can. For at least thirty seconds, hold.
Progression
Position a tiny block beneath the rear leg’s forefoot. Soleus stretch in lie down position On the ground, lie down. Bring your knee up to your chest. Grasp the forefoot’s underside. Firmly bring your foot in your direction. For at least thirty seconds, hold. (Note: If you are unable to reach your feet, you might want to wrap your foot in a towel.)
Soleus stretch in chair

Take a seat in a chair. Bring your knee up to your chest. Slide your back up against the chair. Grasp the forefoot’s underside. Firmly bring your foot in your direction. For at least thirty seconds, hold.
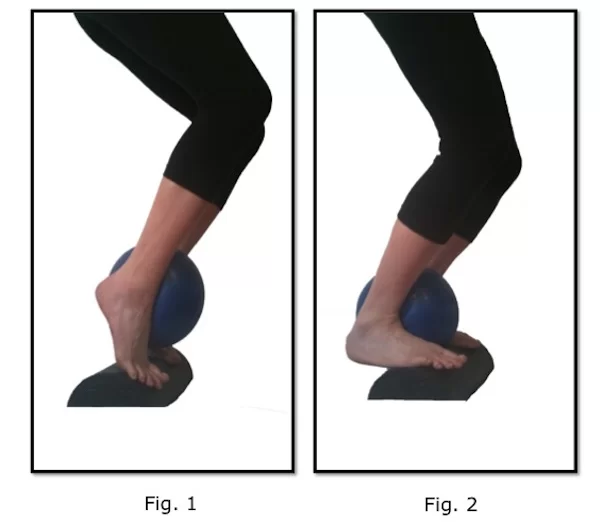
Soleus stretch in half kneeling
On the ground, take a half-kneeling lunge position. (Refer to above) (The side that will be stretched will be the leg in front.) In the front leg, place a small block beneath the forefoot. Hold the foot facing front and forward. Put more weight on your front leg. Bring your knee forward. Keep your heel off the ground at all times. Hold for around for thirty seconds.
Soleus stretch in a squat
Lay your back all the way against the wall. All the way down, squat. Without allowing them to lift off the ground, bring your heels as close to the wall as you can. Put more weight on the tops of your feet by bending your body forward.
Soleus stretches against the wall

Place your front foot up against a wall. Bring your heel as near to the wall as you can. Maintain your heel on the ground. Put all of your weight of body on that foot. Take a forward lunge and move your knee towards the wall. Hold off for 30 seconds.
Eccentric contraction of soleus muscle
Put yourself in a chair and bend your knees to a 90-degree angle. With your heels off the edge, place your forefoot on top of a step. Put a substantial weight above your knee. When your calf muscles are deeply stretched, slowly bring your heels down. Return to the neutral position by raising your heels. Do this ten times over.
Toe tap exercise

This isn’t a stretch, exactly, but it will strengthen the Soleus muscle when extended. This will assist in increasing this muscle’s flexibility. Straighten your posture and grasp a stationary object for stability. Throughout this exercise, keep the knee of the leg that is on the ground in line with your toes. Stretch out your toes as far as possible
Tapping is used to assist the soleus muscle For athletes who want to go back to playing games or other activities that case majority of calf strains heal well with conservative care; without medication or surgery, the muscle forms a tiny fibrous scar. When symptoms subside and strength, flexibility, and range of motion return to levels similar to the contralateral side, full recovery has occurred.
Soleus strengthening different methods
- Double leg raise

Stretching your legs out in forward of you while you are sitting on the ground. Place a foam roller beneath the calf region of the leg that needs work. Place one leg on top of the other that has been in contact with the foam roller.
Completely unwind the lower leg. Apply pressure downward with the upper leg. Use the lower leg to move from side to side. Make sure the calf is completely covered. Continue for a full two minutes.
Progression:
In order to allow your heels to drop below your toes, begin standing on a stairway or similar surface. Lower your heels as close to the floor as you can while maintaining the balls of your feet on the stairs. Next, raise your heels as much as you are able to.
To increase the intensity, add weight. With one hand holding a dumbbell or other weight, repeat the exercise. For balance, keep your hand against a wall.
2. Calf raised with one leg.
By performing the calf raise on one leg, you can intensify it. In this manner, you can further strengthen your calf muscle.
Beginning stance: Balance by standing on one leg close to a wall while bending the other leg behind you. To safeguard the joints, make sure the leg you’re working on has its ankle, knee, and hip in a vertical alignment.
Action: To lift your body higher, apply pressure to the ball of your foot. Retighten your abdominal muscles to prevent moving forward or backward.
Progression:
Step out onto a stairway or something similar. Allow your heel to fall below the step while maintaining the ball of your foot on the stair. Next, raise your body as high as you can. To increase the intensity, add weight. Using one hand, hold a dumbbell or other weight. For balance, rest the other hand against the wall.
3. The seated Calf Lift.

Using a calf exercise machine, you can perform this exercise at home or at the gym. The exercise targets the soleus and gastrocnemius muscles.
At the house.
Starting stance: Place your feet flat on the ground and sit in a sturdy, firm chair. Maintain a straight alignment of your knees over your feet. Keep your knees from bending in or out. To add resistance, bend forward and place your hands on your thighs, just below your knees.
Action: To lift your heels as high as possible, gently press into the balls of your feet. Then gradually bring your heels down. Repeat.
In the fitness center.
Starting stance: Place your feet flat on the platform as you position yourself inside the calf press machine. You can now bring your heels down to the floor. Release the safety latch on the machine and shift the weight onto your calves.
Step 1: Lower the weight by lowering your heels as far as possible towards the floor. Step 2: Press into the balls of your feet to raise your heels as high as you can.
4. Sports for Building Calves and other
Playing these sports will help to tone and strengthen your calves. Exercises like walking, hiking, and running are great for strengthening your calves, especially when you go uphill. The harder the climb, the more effort your calves must put in.
Running sports, like basketball, tennis, and soccer, require you to sprint, jump, and apply force to your calves in order to rapidly change direction or accelerate. They are therefore excellent for toning calves. Every time you take a step up and down in step class or other dance forms, your calves will get a workout.
Safety measures to note while exercises
- To ensure the safety and efficacy of your calf-strengthening exercises, adhere to these guidelines. To develop strength, perform the exercises two or three times a week with consistency.
- Make sure you remain conscious of your body alignment by going slowly through each exercise. For a slow count of two to four, press up. After that, slowly count backward from four.
- To prevent injury, adjust your exercise regimen to your current level of fitness. If you’re not sure how much weight is safe for you to use, consult a fitness expert. Aim for eight to twelve repetitions of each exercise for one to three sets as a general guideline for strength training. Even though your muscles are tired, you should be able to complete your repetitions.
- Gradually increase the muscle’s load over time. For example, increase the weight by 10% to 15% every two weeks.
- If you have previously suffered from a muscle injury in your foot, ankle, or calf, consult your physician first. Certain exercises might not be advised depending on your health or physical condition.
Advanced treatments of soleus strain
1. Blood flow restriction therapy (BFRT)
Blood flow restriction therapy (BFRT), deep water running, LBPPT, and, to a lesser degree, emerging therapies like platelet-rich plasma and stem cell therapy are further treatments for muscle rehabilitation.
Using a restriction band proximally on the extremity to block venous blood outflow while preserving arterial blood inflow, BFRT entails mild resistance training. The muscles are mechanically stressed by light resistance training, and anaerobic metabolism is stimulated and tissue hypoxia is created when a restriction band is used. Studies have indicated that BFRT is superior to unrestricted light resistance training in terms of muscle strength, hypertrophy, and angiogenesis; however, fewer muscles are recruited than with unrestricted heavy resistance training.
In theory, mechanical and metabolic stress combined are thought to have a biological mechanism even though it is unknown.
Signaling pathways within cells that cause fast-twitch muscle fibre recruitment, protein synthesis, and myogenic stem cell stimulation. As a progressive rehabilitation technique to encourage muscle regeneration and healing, BFRT may be helpful as heavy resistance training is frequently not advised in the early phases of recovery.
2. Hydrotherapy
For the rehabilitation of muscles, hydrotherapy methods like deep water running may be taken into consideration. Since the Romans originally reported on the application of hydrotherapy for the treatment of orthopaedic conditions, people have engaged in aquatic exercise. In order to provide resistance and compression as well as balance gravity, hydrotherapy makes use of the buoyancy, viscosity, and hydrostatic pressure of water.
One method of weight-supported aerobic training that involves submerging the body partially in water is called “deep water running.” The buoyant force rising, which is equivalent to the downward force of gravity is opposed by the weight of water that the body displaces. As a result, submersion up to different body parts offloads body weight: up to the hips by 40%, the waist by 50%, the sternum by 60%, or the shoulders by 85%. The pool’s slope, flotation devices, and hydrotherapy treadmills that enclose users in glass-covered aquatic cabins can all be used to regulate the depth of immersion.
There are two types of deep water running: cross-country deep water running, which uses kinematics similar to treadmill running, and high-knee deep water running, which uses stair-stepping movement. It has been noted that cross-country and high-knee deep water running both lessen gastrocnemius activation.
Reducing muscle activation in an environment promotes active recovery and lowers the chance of re-injury.
3. Lower-body positive-pressure treadmill (LBPPT)
Compared to hydrotherapy and other weight-supported rehabilitation techniques, LBPPT has become a well-liked substitute. Weight-supported exercise is possible with lower-body positive-pressure treadmills like the Alter, which allow users to customize the amount of their body weight that the treadmill will support in addition to adjusting the treadmill’s speed and inclination.
Users put on neoprene shorts that fasten to the treadmill’s positive air pressure chamber. Users are raised by a variable force generated by the chamber’s differential air pressure, which lessens the effect of body weight and gravity during exercise. LBPPT has been linked in published reports to better muscle function and posture in patients with muscular dystrophy.
LBPPT has shown a linear decrease in gastrocnemius and soleus muscle activation in healthy individuals in relation to the amount of body weight unloaded during exercise, despite the fact that it has not been investigated in the context of muscle strain.. The decrease in muscle activation is comparable to what is obtained when running in deep water at a stride frequency that matches. Moreover, adjustments that lower the treadmill’s inclination and/or speed also reduce the activation of the soleus and gastrocnemius muscles. For this protective reason, published reports have proposed LBPPT as a substitute for hydrotherapy and as a treatment option for patients starting a rehabilitation program.
4. Platelet-rich plasma infusion therapy
An autologous platelet-rich blood product made by centrifuging whole blood is called platelet-rich plasma. It is said that platelets release cytokines and growth factors that promote regeneration.
Although stem cell therapy’s therapeutic applications are still in their infancy, they show promise for muscle recovery. By promoting the growth of new muscle fibres and vascularization, stem cell therapy seeks to restore the skeletal tissue’s structural integrity and functionality. Stem cell therapy has shown accelerated muscle recovery with improved angiogenesis and decreased formation of scar tissue in animal models. A small number of clinical trials have examined stem cell therapy, mainly for the treatment of incontinence disorders and muscular dystrophies. Patients in these clinical trials experienced a range of outcomes, from no change in muscle histology and/or functionality to improvements in these measures, depending on whether they received transplantation. The discrepancies between published reports can be partially attributed to small patient samples, differences in study methodology, and a lack of clarity regarding the biological mechanisms induced by stem cell therapy. More proof supporting the application of stem cell therapy in muscle rehabilitation might come from future studies.
Massage
It is applied in a circular motion. It is also applied with the help of a messenger a known instrument for massage.
Electrotherapy
Physiotherapy rehabilitation can begin after 48 hours of injury, For the first few days give an electric modality to reduce inflammation and pain
Ultrasound
Ultrasound has been used to promote blood flow, improve mobility, and lessen swelling in tissue healing.
Cryotherapy
Applying cryotherapy—which involves applying ice packs and cold water baths to the affected area—can reduce swelling and inflammation. It is recommended to apply colds several times a day for 15 to 30 minutes at a time.
IFT or TENS
Pain and muscle spasms may be lessened with the use of interferential therapy (IFT) or transcutaneous electrical nerve stimulation (TENS).
Prevention of soleus strain
Preventing injuries is simpler than treating them. Here are some pointers to prevent a soleus strain and other muscular injuries: Observing any discomfort. It’s critical to pay attention to your body during exercise and to stop if you experience any pain or uncomfortable muscle tightness.
Getting heated. The risk of injury can be decreased by warming up the muscles with mild aerobic exercises like walking, jogging, or gentle cycling before engaging in intense exercise. Extending. Stretching gently both before and after exercise can also help reduce the risk of injury.
Applying pressure to tense muscles with a foam roller. The use of a foam roller has been shown to improve the range of motion and lessen pain (Trusted Source). In support of these advantages, foam increases soleus flexibility and stability
Recovery duration of soleus strain
The severity, location, and kind of activity you engage in all influence how long it takes for a calf strain to heal. An elite athlete returning to peak performance will require a longer recovery period than someone who is active or participates in sports for enjoyment.
Grade I calf strains can heal in eight days, elite athletes have reported that it takes an average of sixteen weeks to return to their pre-injury level of performance.
Grade II calf strains heal in four to six weeks, but according to one study, dancers need up to fifty weeks on average to return to their previous level of competition.
Grade III calf strains require two to three months to heal, but if surgery is required owing to a serious injury, the healing process may take up to six months.
An injured leg may get worse if you run on it. Rest is necessary for a calf strain to heal. Wait until you are pain-free before jogging or doing other intense exercises. After a calf strain, your healthcare provider will advise you on when to resume running.
Summary
An injury that affects the muscles in the back of the leg is called a calf strain. The degree of pain is a function of the injury’s severity.
Strains of grade I cause very little pain. Strains of grade II cause more pain and will restrict your activities. Your ability to walk may be affected by grade III strains.
Strains in the calf muscles are typically easy to diagnose. However, other factors can occasionally be the source of calf pain. See a doctor if your pain doesn’t subside right away.
Recovery requires rest. Additionally, your physical therapist might advise using heat, ice, and mild stretching techniques. Medication available over the counter can relieve pain.
FAQs
Since soleus injuries dislike prolonged periods of time on feet, avoid long, slow, continuous running at first.
Additionally, they stated that when running compared to walking, the soleus H reflex’s peak amplitude was consistently lower.
It’s crucial to stop cycling and avoid putting any weight on your leg if you have a calf injury.
A calf muscle typically heals in 6 to 8 weeks.
References
- Cluett, J., MD. (2023, August 16). Everything you need to know about a calf strain. Verywell Health. https://www.verywellhealth.com/calf-strain-muscle-spasm-of-the-leg-2549855#toc-calf-strain-symptoms
- Soleus. (n.d.). Physiopedia. https://www.physio-pedia.com/Soleus
- Calf strain. (n.d.). Physiopedia. https://www.physio-pedia.com/Calf_Strain
- Professional, C. C. M. (n.d.-j). Pulled calf muscle. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21558-pulled-calf-muscle
- Cluett, J., MD. (2023, August 16). Everything you need to know about a calf strain. Verywell Health. https://www.verywellhealth.com/calf-strain-muscle-spasm-of-the-leg-2549855#toc-calf-strain-symptoms
- Could your leg pain be varicose veins? (2023, August 23). Mayo Clinic Health System. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/could-your-leg-pain-be-varicose-veins
- O’Connell, K. (2019, March 8). What causes leg pain and how to treat it. Healthline. https://www.healthline.com/health/leg-pain#when-to-seek-help
- Why do my legs hurt? (n.d.). WebMD. https://www.webmd.com/pain-management/ss/slideshow-leg-pain-causes
- M, N. K. (2020, March 6). Leg Pain: symptoms, causes, treatment, medicine, prevention, diagnosis. myUpchar. https://www.google.com/amp/s/www.myupchar.com/en/disease/leg-pain.amp
- Admin. (2019, April 3). At Home Workouts To Relieve Leg Pain – The Vascular Institute of Birmingham. The Vascular Institute of Birmingham. https://new-legs.com/at-home-workouts-to-relieve-leg-pain/
- Cadman, B. (2023, October 9). What are the best foot exercises for healthy feet? https://www.medicalnewstoday.com/articles/32096





One Comment