Temporomandibular Joint (TMJ) disorders
Table of Contents
What is Temporomandibular Disorder (TMD)?
- Temporomandibular Disorder (TMD) is a broad term that encompasses disorders of the temporomandibular joint(TMJ) and its associated anatomical structures.
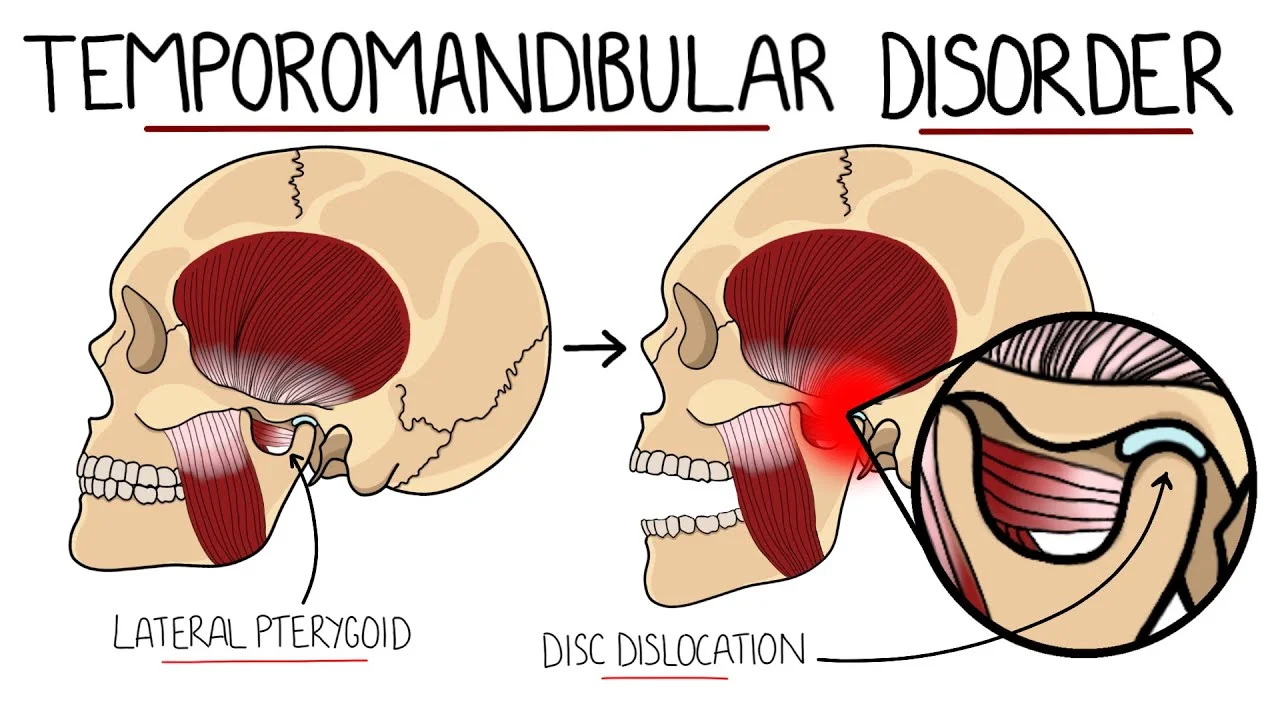
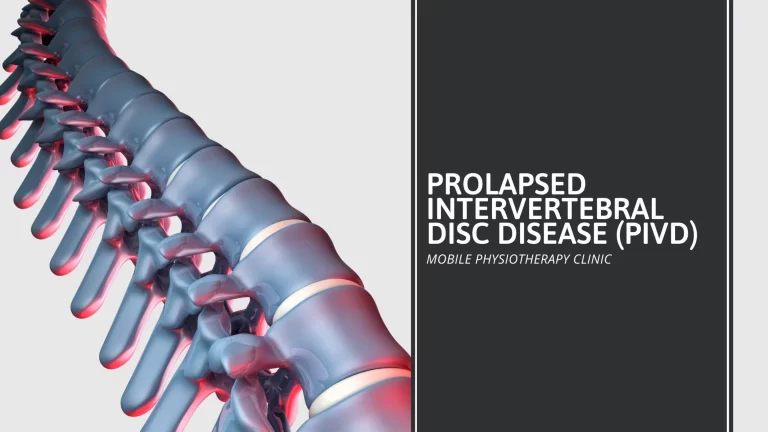
- The Temporomandibular disorder might be intraarticular, due to inflammation, internal structural changes (internal derangement), or degeneration, or it might be extraarticular due to imbalance or over-activity of jaw muscles, commonly the mastication muscles or the cervical muscles.
- There is a strong correlation between postural dysfunction of the cervical spine and Temporomandibular Disorder. There are numerous other conditions that can cause pain in the temporomandibular joint(TMJ) region. It is important to make an accurate diagnosis to ensure that the correct treatment is given and that potentially serious problems are not overlooked.
Relevant Anatomy
temporomandibular joint(TMJ) Anatomy
In an early study on postmortem specimens, it was found that the lateral pterygoid muscle was connected to the medial aspect of a joint capsule, meniscus, and a condyle pterygoid fovea in more than half of the specimens. It indicated that the muscle can have a specific contribution to Temporomandibular Disorder (TMD).
What causes Temporomandibular Joint disorders?
In many cases, it’s not known what causes Temporomandibular Joint disorders. Trauma to the jaw or joint might play a role. There are also other health conditions that can contribute to the development of Temporomandibular Joint disorders.
These include:
- Osteoarthritis
- erosion (wearing away) of your joint
- habitual grinding or clenching of your teeth
- structural jaw issues present at birth
- growth disorders
Symptoms
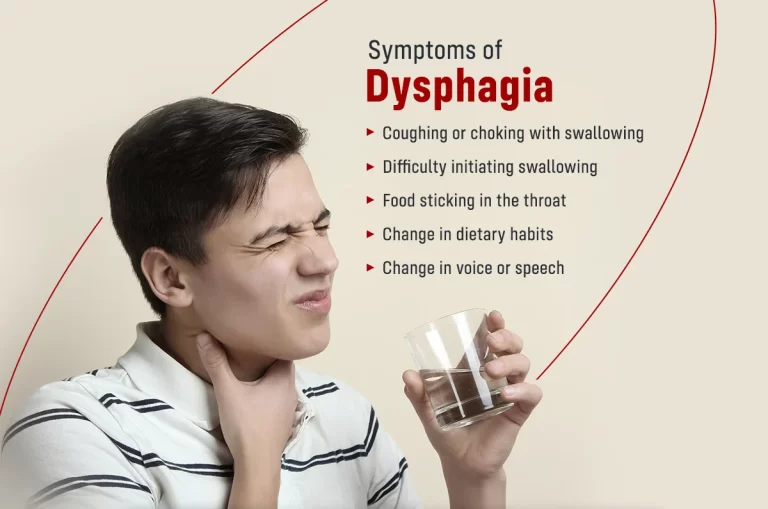
The symptoms of disorders depend on the severity and cause of your condition. The most common symptom of temporomandibular Joint disorders is a pain in the jaw and surrounding muscles.
other symptoms typically associated with these temporomandibular Joint disorders include:
- pain that can be felt in the face or neck
- stiffness in the muscles of a jaw
- limited movement of a jaw
- locking of a jaw
- clicking or popping sound from the temporomandibular Joint site
- dental issues, like wearing down of teeth
- tinnitus (ringing in the ear)
- vertigo
- headaches
- shift in the jaw, changing the way that upper and lower teeth align (called malocclusion)
- Symptoms can show up on just one side of the face or both.
How are Temporomandibular Joint disorders diagnosed?
Temporomandibular Joint disorders can be difficult to diagnose. There are no standard tests to diagnose most of the disorders which fall under that title. A doctor might refer you to a dentist, or an ear, nose, and throat (ENT) specialist to diagnose the condition.
A healthcare professional might examine you to see if there is swelling or tenderness. They might also use several different imaging tests.
These can include:
- X-rays: X-rays of the jaw and teeth usually involve you biting down on the small mouthpiece as your dentist moves an imaging machine around your head. These X-rays allow your dentist to see the bones in and around your jaw, as well as your teeth placement.
- CT scan: A CT scan of the jaw allows the doctor to see the bones and joint tissues in a more advanced way than a regular X-ray.
- MRI: An MRI will show if there are problems with the structure of a jaw. An MRI, or magnetic resonance imaging scan, uses a magnetic field to show detailed images of tissues and organs.
How are Temporomandibular Joint disorders treated?
Because Temporomandibular Joint disorders can have a variety of causes, there are also a variety of ways to treat them.
Physicians typically advise starting with home treatments first. This is due to many of the more complicated treatments still needing more studiesTrusted Source to prove their efficiency.
Home treatments
In a lot of cases, the symptoms of Temporomandibular Joint disorders can be treated with self-care practices at home. To ease the symptoms of Temporomandibular Joint at home, you can:
- Eat soft foods.
- You can use ice to reduce swelling
- Reduce jaw movements
- You have to avoid chewing gum and tough foods (like beef jerky).
- Take measures to reduce stress.
- Use jaw-stretching exercises to help improve your jaw movement.
Medication
If you find that your Temporomandibular Joint is not eased by using home treatments, some medications both over the counter and prescribed by a doctor can provide more relief.
Some of these medications include:
- nonsteroidal anti-inflammatory drugs (NSAIDs)
- corticosteroids
- muscle relaxers
- antidepressants
- local anesthetics
- Your doctor will help you decide which medication is best for you, based on your personal condition and health history.
Surgery or other procedures
If your symptoms do not improve with the methods listed above, your doctor might decide that your condition requires serious treatment.
Botox injections are one such treatment. Typically, these injections are used for painful trigger points or chronic teeth grinding. The evidence behind this treatment is still lackingTrusted Source, however.
In very rare cases, your doctor might recommend surgery to treat your condition. Procedures can include:
- corrective dental treatment to improve the bite and align your teeth
- arthrocentesis, which removes fluid and debris from your joint
- surgery to replace your joint
- Procedures used to treat this condition might, in some cases, make your symptoms worse. Talk with your doctor about the potential risks of this procedure.
Physiotherapy treatment
Relaxed jaw exercise
- Place your tongue behind the upper front teeth on the top of your mouth. Relax the jaw muscles thus allowing your teeth to fall apart.
Goldfish exercises (partial opening)
- Place one finger in front of your ear, where your Temporomandibular Joint is located, and the tongue on the roof of your mouth. Place the chin on your middle or pointer finger. Lower the jaw in half and then close it. There should be some resistance, but it does not be painful. Placing one finger on each Temporomandibular Joint while dropping your lower jaw halfway and closing it again is a variant of this exercise. In one sequence, repeat this exercise 5 to 6 times. One collection should be done six times per day.
Goldfish exercises (full opening)
- Place one finger on your Temporomandibular Joint and another on your chin while keeping the tongue on the roof of your mouth. Return the lower jaw to its natural position. Place one finger on each Temporomandibular Joint as you fully drop your lower jaw and back for a variation of this exercise. To complete one set, repeat this exercise 5 to 6 times. One collection should be completed six times per day.
Chin tucks
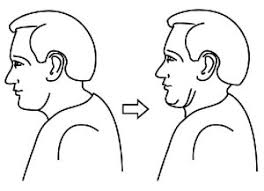
- You have to pull your head straight backward, making a “double chin,” with your shoulders down and chest up. Hold for three seconds and then repeat ten times.
Risk factors
While there are some factors that are often associated with the development of Temporomandibular Joint disorders, they have not been proven to be a direct cause.
Some of these include:
- female hormones (it’s theorized that estrogen might play a role in the development of the Temporomandibular Joint)
- poor posture which strains the muscles of the neck and face
- prolonged stress
- joint hypermobility
How can Temporomandibular Joint be prevented?
You might not be able to prevent Temporomandibular Joint disorder from developing, but you might be able to lower symptoms by lowering your stress levels, employing physical therapy and exercises, and working with the dentist or doctor if you often grind your teeth at night.
Possible solutions for teeth grinding include wearing a mouth guard during the night and occasionally taking muscle relaxants.




One Comment