Palatoglossus Muscle
Table of Contents
Palatoglossus Muscle Anatomy
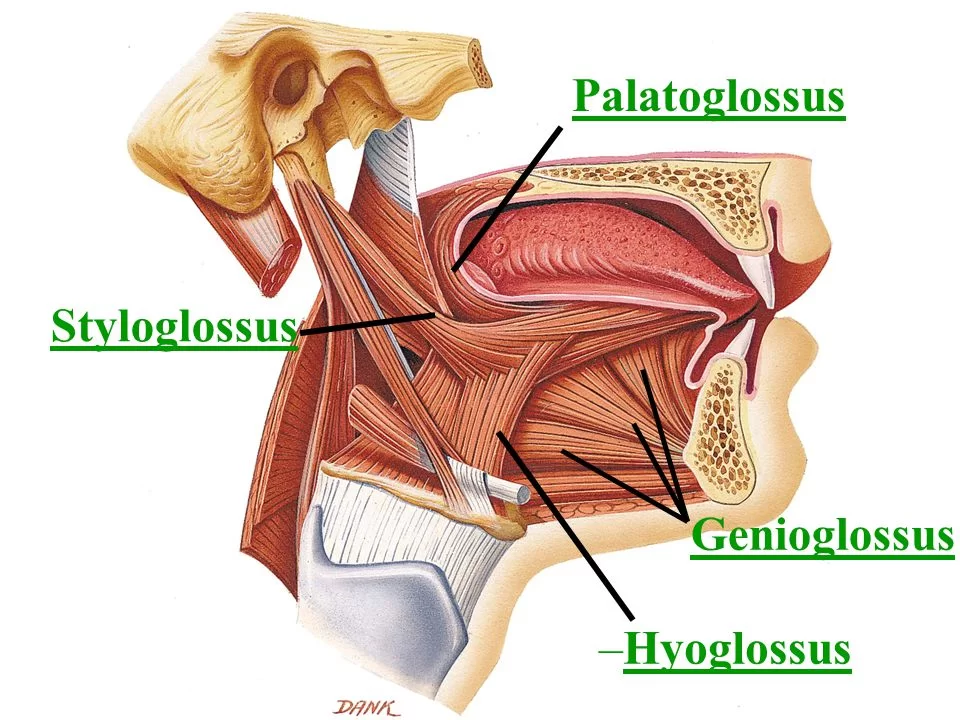
The palatoglossus muscle is a significant anatomical structure located in the oral cavity. It is one of the four extrinsic muscles of the tongue and plays a crucial role in the movement and function of the tongue.
Structure
Palatoglossus arises from the palatine aponeurosis of the soft palate, where it is continuous with the muscle of the opposite side, and passing downward, forward, and lateralward in front of the palatine tonsil, is inserted into the side of the tongue, some of its fibers spreading over the dorsum, and others passing deeply into the substance of the organ to intermingle with the transverse muscle of the tongue.
Origin
Palatine aponeurosis.
Insertion
Side of the Tongue.
Nerve Supply
Vagus nerve (via pharyngeal branch to pharyngeal plexus).
It is the only tongue muscle that does not get innervation from the hypoglossal nerve (CN XII).
Blood Supply and Lymphatic Drainage
The lingual artery, a branch of the external carotid artery, provides the vascular flow. The tonsillar artery, a branch of the facial artery, also contributes to some collateral circulation. The deep cervical group of lymph nodes receives lymphatic outflow.
Functions:
The root of the tongue is raised by the palatoglossus muscle.
It roughly connects the ipsilateral (same side) and contralateral (opposite side) palatoglossal arches, dividing the oropharynx from the oral cavity.
Elevates posterior tongue, closes the oropharyngeal isthmus, and aids initiation of swallowing. This muscle also prevents the spill of saliva from the vestibule into the oropharynx by maintaining the palatoglossal arch.
Raising the back part of the tongue.
Course of the Muscle
The palatine aponeurosis’ inferior surface is where the muscle originates. It inserts into the posterolateral surface of the tongue after descending inferiorly, forwardly, and laterally with the contralateral side muscle prior to the palatine tonsil. While some of the muscle’s fibers extend across the tongue’s dorsal surface, other fibers penetrate deeply into the tongue’s substance and interact with the transverses linguae, one of the tongue’s intrinsic muscles.
The palatoglossus is a small muscle as compared to the other palate muscles. The muscle that divides the tonsil’s superior portion from the “supratonsillar fat” The tonsillar pillar’s anterior border is formed by the muscle.
Anatomical Variations
There has been evidence of variation in the palatoglossus muscle’s attachment site in the soft palate. In some people, this area is close to the uvula.
The absence of a solid anchoring point towards which the tongue elevates may affect the palatoglossus muscle’s ability to elevate the tongue. On the other hand, this attachment helps to lower the soft palate. The fulcrum, or the posterior rim of the hard palate, and the applied force, or the action of the palatoglossus muscle, are situated between the load, or the majority of the soft palate, in this class II lever system action.
There is a significant increase in the muscle’s capacity to raise the tongue in these situations. This attachment, however, does not help to lessen the soft palate. The class III lever system that underpins this action places the applied force between the load and the fulcrum. Rather than lowering the soft palate, these people primarily approximate the tongue and soft palate during swallowing by elevating the tongue.
Embryology
Only the palatoglossus muscle comes from the fourth branchial arch of the tongue. The occipital myotomes are the source of all other tongue muscles. For this reason, the palatoglossus muscle, which is innervated by the tenth cranial nerve (vagus nerve), is the only tongue muscle not innervated by the twelfth cranial nerve (hypoglossal nerve).
Clinical Importance
Velar positioning is provided by the levator veli palatini muscle in combination with the palatoglossus and palatopharyngeus muscle’s ability to elevate the velar region.
Role in obstructive sleep apnea:
Research has demonstrated that retropalatal space can widen in response to electrical stimulation of the palatoglossus muscle nerve, which helps lessen the severity of obstructive sleep apnea. The mechanism underlying this function is that stimulation of the nerve moves the tongue base forward, perhaps causing the anterior palatal pillar to migrate anteriorly and advancing the palate. Concurrently, the palatoglossus muscle facilitates anterior movement of the soft palate and aids in the expansion of the retropalatal region.
Role in tonsillar cancer:
Tonsillar cancer typically originates from the anterior tonsillar pillar and tends to expand locally to the tongue, superomedial to the soft palate, or nasopharynx. The tumor can impact the anterior tonsillar pillar and the palatoglossus muscle, so affecting the hard and soft palates as well as the base of the tongue. The pterygoid muscles, levator palatine, and tensor palatine may be impacted if the tumor is located in the palate.
Function in tongue base cancer:
A tumor at the base of the tongue, especially if it affects the posterior third, has the potential to spread to the anterior tonsillar pillar by traveling down the palatoglossal muscle. It may extend to the nasopharyngeal region via the veli palatini muscles and then, via the palatoglossus muscle, to the soft palate.
Role in cleft lip and palate: In cleft patients, achieving an appropriate length for the soft palate is necessary for both continuity and function; this calls for the reconstitution of the levator veli palatini, palatopharyngeus, and palatoglossus.
Deep to the palatoglossus muscle, the peritonsillar abscess typically develops superior to the tonsillar area, which is the intersection of the anterior tonsillar pillar and the base of the uvula.
Clinical Importance
Compared to individuals without obstructive sleep apnea, it has been demonstrated that patients with obstructive sleep apnea experience a collapse of the lateral pharyngeal wall during airflow. This collapse could occur as a result of a potential delay in the constrictor muscle relaxation during the expiratory-inspiratory transition. A procedure called lateral pharyngoplasty was created to address these pathophysiological facets of apnea. The lateral pharyngeal wall is repaired via myotomy of the superior constrictor muscles and suturing of the lateral pedicle flaps to the palatoglossus muscle.
Midline soft palate splitting and anterior mucosa removal are two of the surgical techniques used in zeta-pharyngoplasty. The posterior palatal mucosa is sewn to the anteriorly removed margin after the palatoglossus muscle is severed for this purpose.
Role in Glossectomy:
The extent of tumor dissemination determines the region that can be surgically removed during a tongue tumor operation. Depending on the area that is removed, glossectomy procedures can be categorized into several groups.
Type IIIb glossectomy, also known as compartmental hemiglossectomy, involves the mucosa, submucosa, intrinsic muscles (transversalis, verticalis, inferior longitudinalis, and superior longitudinalis), and extrinsic muscles (genioglossus, hyoglossus, styloglossus, and the inferior portion of the palatoglossus muscle) on the same side.
FAQs
The back part of the tongue is raised by the palatoglossus muscle. Additionally, it drags the soft palate inferiorly, reducing the oropharyngeal isthmus’ diameter.
The palatoglossal muscle is an extrinsic tongue muscle and a soft palate muscle. Its surface is covered in oral mucosa, and the palatoglossal arch is visible.
The Vagus nerve (cranial nerve (CN) X/XI group) innervates the palatoglossus muscle, an extrinsic muscle.
The palatoglossus, a soft palate muscle, and the mucosa that covers it together make up the palatoglossal arch (also known as the palatoglossal fold).
Origin: The muscle originates from the palatine aponeurosis’ oral side, where it joins with the opposing muscle.
the tongue
One of the four extrinsic muscles of the tongue is the palatoglossus. The palatine aponeurosis, a fibrous layer at the back roof of the mouth known as the soft palate, is where this muscle gets its start. The palatoglossus muscle then descends from this point and joins with the tongue.
References
- Rathee, M., & Jain, P. (2023, June 5). Anatomy, head and neck, palatoglossus muscle (Glossopalatinus, palatoglossal). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK549823/
- Palatoglossus muscle. (2024, January 19). In Wikipedia. https://en.wikipedia.org/wiki/Palatoglossus_muscle