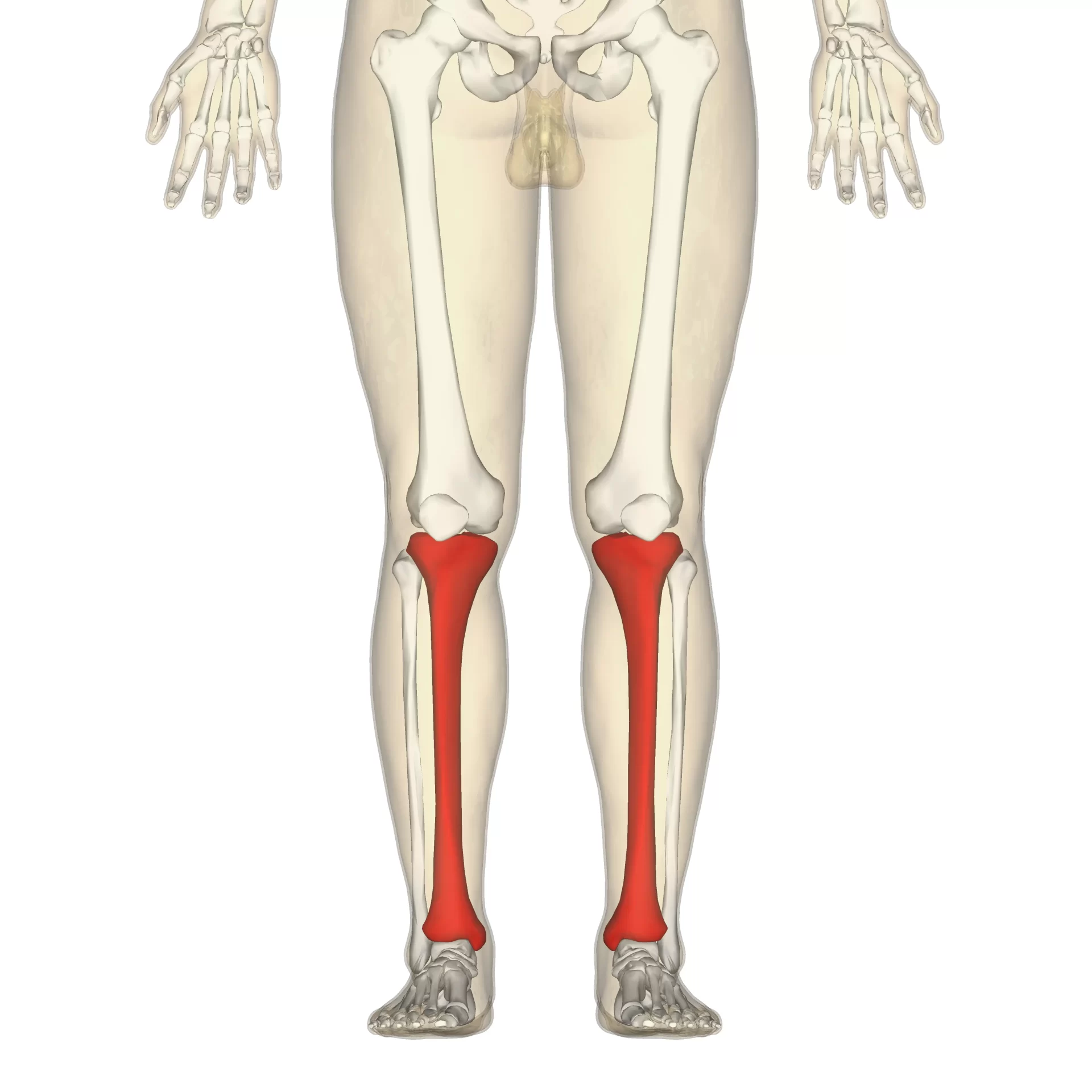
Tibia Bone
Table of Contents
Introduction of the tibia bone
- The Tibia Bone, which is the second-largest bone in the body, is primarily used for weight bearing, with the medial portion of the tibia supporting the majority of the stress. Eleven muscles, which enable dorsiflexion and plantar flexion at the ankle joint and extension and flexion at the knee joint, many muscles attach at this location.
- The interosseous membrane connects the tibia to the fibula as it travels medially from just below the knee joint to the ankle joint.
- The posterior surface about the posterior compartment of the leg, the lateral surface about the anterior compartment, and the medial surface are primarily subcutaneous.
- The medial malleolus is a distal medial protuberance that forms the distal section of the tibia, which has a box-like structure. tibia is the second larger and stronger bone of the body which make it benefited from prevention from injuries or any pathology.
- The proximal tibia is composed of five surfaces. As below mentioned,
- There is a clear articulation between the inferior surface of the tibia and the talus.
- Ankle joint capsule connection is made possible by the extensor tendons covering the anterior side.
- The tibialis posterior muscle is there in a groove on the posterior surface.
- The interosseous membrane attaches to the lateral surface by a fibular notch.
- The medial malleolus is composed of a broad bony protrusion called the medial surface.
Embryology and Development of the Tibia Bone
Embryology and Development of the Tibia Bone is as mentioned below ,
- Beginning at birth, the proximal ossification center closes at age 16 for females and age 18 for males.
- A primary center for the diaphysis (shaft) and a secondary center for each epiphysis (extremity) make up the ossified tibia. Around the seventh week of fetal life, ossification starts in the center of the body and progressively moves outward towards the extremities.
- Nearly 34 weeks gestation is when the center of the upper epiphysis first develops. It is flattened in shape and has a thin tongue-shaped process in front.
- This creates the tuberosity; in the second year, the lower epiphysis emerges. Periodically, there are two more centers: one for the medial malleolus and one for the tongue-shaped feature of the upper epiphysis, which creates the tuberosity.
Region of the tibia bone
The Region of the tibial bone is described below,
The Proximal end of the tibia bone
The Proximal end of the tibia bone is as follows ,
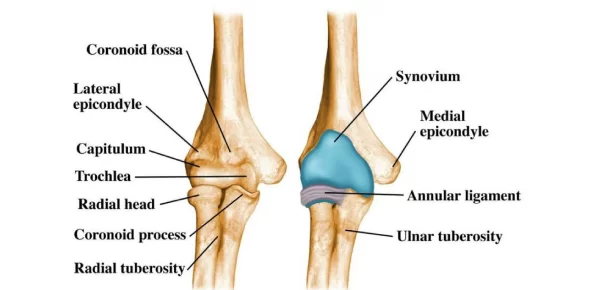
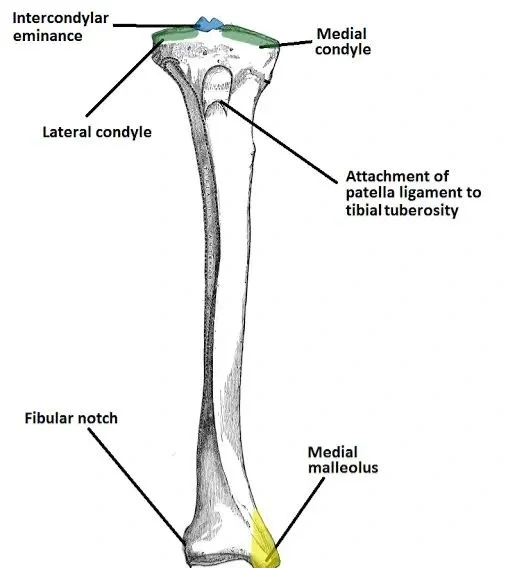
- The medial and lateral condyles enlarge the proximal tibia and facilitate weight bearing. The tibial plateau is a level area formed by the condyles. The femoral condyles and this structure articulate to generate the main knee joint articulation.
- The inter-condylar space, which is situated between the condyles, extends upward on both sides as the medial and lateral inter-condylar tubercles. The menisci and ligaments of the knee joint adhere mostly to this region. The tibia’s intercondylar tubercles and the femur’s intercondylar fossa articulate.
The Shaft of the tibia bone
The Shaft of the tibia bone is as follows ,
- The front, posterior, and lateral surfaces of the prism-shaped tibia shaft are its three borders. Only the anatomically and therapeutically significant borders and surfaces are covered in this passage to avoid repetition.
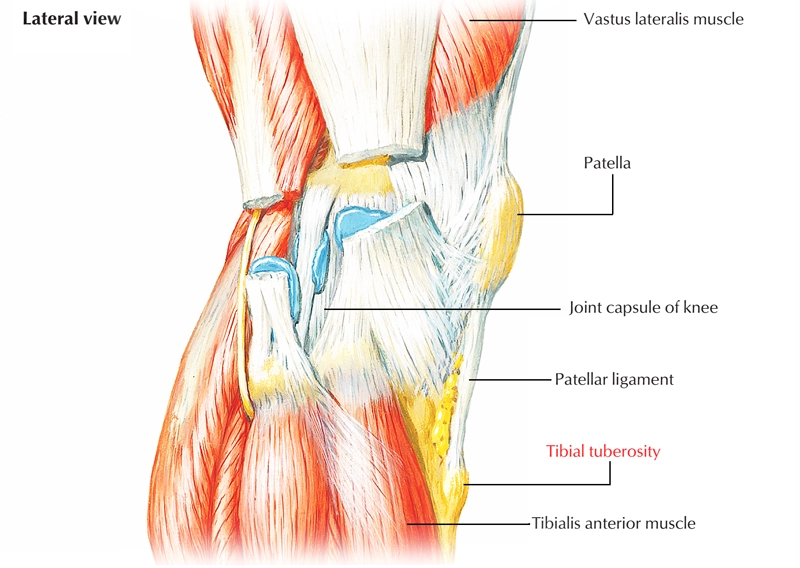
- Subcutaneously perceptible along the anterior leg area, extending down to the shin. The patellar ligament’s attachment location, the tibial tuberosity, denotes the proximal side of the anterior border. The sole line, a bone ridge, denotes the posterior surface. Part of the soleus muscle arises from this line, which extends inferomedial before merging with the tibia’s medial border. A nutritional artery is typically located close to the sole line.
- The interosseous boundary is another name for the lateral border. It provides attachment to the distal interosseous membrane, which connects the tibia and fibula.
The distal end of the tibia bone
The distal end of the tibia bone is as follows ,
To help with weight bearing, the tibia’s distal end expands. On the medial aspect of the tibia, the medial malleolus is a bony protrusion that extends inferiorly. It forms a portion of the ankle joint by articulating with the tarsal bones. There is a groove on the tibia’s posterior surface via which the tendon goes.
Identification of the side of the tibia bone
Finding the Tibia Bones on the Left and Right both sides of the body, Here’s a short method for telling the left tibia from the right.
- The medial malleolus, a bony projection, should be at the bottom of the vertically held bone, with the lateral and medial condyles at the top.
- Determine which side the larger medial condyle faces by identifying it now. It is a right tibia if it faces left, and vice versa.
- As an alternative, you might look at the side that the medial malleolus is on. It is a right tibia if it is positioned on the right side, and vice versa.
Tibia bone in the other animals
tibia bone in other animals describes as follows ,
Most other tetrapods have tibiae that are fundamentally comparable to human tibiae. In reptiles, birds, and amphibians, which lack patella, the tendon of the quadriceps muscle is instead attached to the tuberosity of the tibia, a crest to which the patellar ligament connects in mammals.
Lymphatics and Blood Supply of the tibia bone
Lymphatics and Blood Supply of tibia bone is as follows ,
- The nutritional artery and the periosteal vessels provide the tibia with its blood supply. After splitting off from the posterior tibial artery, the nutritional artery enters the bone posteriorly and distal to the soleal line. The origin of the periosteal vessels is the anterior tibial artery.
- Every principal nerve that supplies adjacent compartments is a branch that supplies the tibia. The anterior aspect of the tibia is supplied by the branches of the deep fibular nerve in the leg’s anterior compartment, whereas the tibial nerve supplies the posterior side of the tibia in the posterior compartment of the leg.
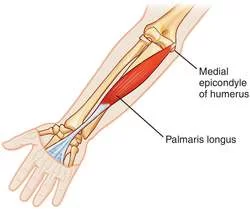
Muscle inserted at the tibia bone
Muscle inserted at the tibia bone is as follows ,
- The tibia has a lateral tubercle, also Known as Gerdy tubercle, it is the place where the tendon of fasciae latae inserted in that part of a tibia bone.
- The tibial tuberosity is the part of the bone where the quadriceps femoris muscle inserts the anterior side.
- On the pes anserinus, the gracilis, semitendinosus, and sartorius insert anteromedial.
- The medial condyle is a part of the tibia the bone where the horizontal head of the semimembranosus muscle inserts the bone.
- The popliteal inserts on the posterior sole line.
Origin of the Muscles at the Tibia Bone
Origin of the Muscles at the Tibia Bone is as belows ,
- The upper two-thirds of the lateral tibia is the Origin of the tibialis anterior muscle in the bone.
- The lateral condyle of the tibia bone is the site of origin of the extensor digitorum longus muscle in the lower limb.
Variants of the tibia bone in Physiology
Variants of the tibia bone in Physiology is A ball and socket ankle joint, as opposed to the typical hinged ankle joint, is one of the physiologic varieties involving the tibia. The distal tibia in this variation articulates with a rounded superior talus and is concave.
Fibula bone Vs tibia bone
The most special features of tibia bone and fibula bone which differ from each other is as follows ,
- The tibia and fibula are the two bones that make up your lower leg. The longer tibia is made up of your ankle at the top (proximal) and part of your knee at the bottom (distal). As a result of bearing weight, the tibia supports your body when you stand and walk.
- The fibula primarily gives your leg structural support and does not bear as much weight.
Clinical Significance
the signs and symptoms of tibial stress syndrome is as below mentioned paragraph which related to tibia bone. tibia is the second larger and stronger bone of the body which make it benefited from prevention from injuries or any pathology.
Widespread, recurring lower leg pain is the hallmark of shin splints, also known as medial tibial stress syndrome. Although the exact mechanism is unknown, biomechanical anomalies that result in excessive force on the tibia are thought to be the cause.
Due to their frequent application of excessive leg power, runners and aerobic dancers are the most common users of it. It is often associated with the trinity of conditions that affect female athletes: amenorrhoea, low caloric intake, and osteoporosis. A substantial area of the distal medial tibia can be palpated to elicit pain, a sign of medial tibial stress syndrome. Traction periostitis is the etiology.
the signs and symptoms of Osgood-Schlatter disease is as below mentioned paragraph which related to tibia bone.
Osgood-Schlatter disease, or apophysitis of the tibial tubercle in the tibia bone is Known for pain Under the knee that worsens with movement and goes away with rest if given to the patient
Other Concerns
Compartment syndrome is one of the most dangerous side effects of a tibial fracture, and if it is not treated quickly, it can result in leg necrosis.
Paget’s Bone disease
the signs and symptoms of paget’ s disease is as below mentioned paragraph which related to tibia bone.
Osteitis deforming, often known as Paget’s disease of the bone, is a long-term bone condition. Those over 50 and those descended from Northern Europe are typically affected. Among the symptoms are:
- ache in the joints or bones.
- bent legs or arms.
- curved shape of the back.
Tibial torsion
the signs and symptoms of tibial torsion is as below mentioned paragraph which related to tibia bone.
- The tibia serves as the primary structural support of the lower limb and is primarily in charge of the foot’s position, function, and motion. The congenital disease known as internal tibial torsion results in the tibia rotating in the direction of the medial side. To put it simply, the toes point in the direction of each other as the tibias rotate inward. It’s common to call this “pigeon-toeing.” A benign ailment, tibial torsion normally heals on its own during the first four years of life.
- The doctor of a child will probably wish to keep an eye on the child’s growth and development to look for any issues. In most cases, braces and other corrective equipment are not required.
Congenital Tibial pseudarthrosis
the signs and symptoms of Congenital Tibial pseudarthrosis is as below mentioned paragraph which related to tibia bone.
The uncommon ailment known as pseudoarthrosis of the tibia is typically not identified until the tibia spontaneously fractures. It is very difficult to treat the pseudo arthrosis and repair the fracture once the tibia fractures.
Hemimelia’s Tibia
the signs and symptoms of Hemimelia’s Tibia is as below mentioned paragraph which related to tibia bone.
- A rare disorder called tibial hemimelia often affects the development of one limb exclusively. This word refers to a wide range of tibia, fibula, knee, and ankle presentations. Tibial bowing is the term for the bending of the tibia, which can occur alone or in conjunction with the fibula. It’s also possible that the tibia is absent or deformed.
- Only the proximal or distal end of the tibia may be visible in certain instances of tibial hemimelia. The fibula may have a duplicate fibula or be larger to make up for it.
- Tibial hemimelia can be treated with very few options that depend in part on how the tibia and fibula are formed generally. Amputation and prosthesis replacement are frequently the best course of action. the signs and symptoms of Hemimelia’s Tibia is as describe in above mentioned paragraph will help you to get diagnose the condition ,
Surgical approach to managing tibial bone fractures
Fractures of the tibial plateau:
Surgical approach to managing tibial bone plateue fractures is as follows,
- These fractures cause effusion and knee discomfort. They typically happen as a result of a car striking a pedestrian’s fixed knee, or “bumper fracture.” tibia is the second larger and stronger bone of the body which make it benefited from prevention from injuries or any pathology. The Schatzker classification is used to categorize them, and nonsurgical or surgical techniques are employed to attain stable alignment. Open reduction internal fixation and external fixation are examples of operational techniques.
Schatzker Classification
the types of the Schatzker Classification is as follows,
- Type 1: fracture with a lateral split
- Type 2: fracture with lateral split-depression
- Type 3: fracture with a lateral pure depression
- Type 4 Medial fracture,
- Type 5 Bicondylar fracture,
- Type 6 Metaphyseal-diaphyseal disassociation
Tibial shaft fracture:
Surgical approach to managing tibial bone shaft fractures is as follows,
- Because the medial surface of a tibial shaft fracture is next to the subcutaneous tissue, it is more likely to be open than the majority of long bone fractures. A low or high-energy pattern may be present in the fracture. The spiral fracture caused by torsional injury is the cause of the low energy patterns. A direct force that results in an oblique or wedge fracture is the source of the high-energy pattern. tibia is the second larger and stronger bone of the body which make it benefited from prevention from injuries or any pathology.
- For low-energy fractures that are minimally displaced, Nonoperative therapy is preferred; for high-energy fractures, surgical treatment, such as external fixation, intramedullary nailing, and percutaneous locking plate, is suggested. Significant soft tissue damage, compartment syndrome, malunion, and bone loss can result from these fractures. Distal tibia fractures in the ankle: The inability to bear weight ankle pain and edema are the most common symptoms of these injuries. They typically occur from significant ankle joint inversion or eversion. For low-energy fractures that are minimally displaced, Nonoperative therapy is preferred; for high-energy fractures, surgical treatment, such as external fixation, intramedullary nailing, and percutaneous locking plate, is suggested. Significant soft tissue damage, compartment syndrome, malunion, and bone loss can result from these fractures. Distal tibia fractures in the ankle: The inability to bear weight ankle pain and edema are the most common symptoms of these injuries. They typically occur from significant ankle joint inversion or eversion.
- To identify the type of fracture, the Lauge-Hansen and Danis-Weber classifications are frequently employed. Additionally, there are a few distinct distal tibial fractures with unique names. The distal tibia and its articular surface with the ankle joint are affected by the Pilon fracture, while the anterolateral distal tibial epiphysis is affected by the Tillaux fracture. Internal fixation and open reduction are the most common treatments for distal tibial fractures.
Classification of Lauge-Hansen
the types of the Lauge-Hansen are as follows,
- Adduction-supination
- External rotation in suspension
- pronation-abduction
- external rotation and pronation
To identify the type of fracture, the Lauge-Hansen and Danis-Weber classifications are frequently employed. Additionally, there are a few distinct distal tibial fractures with unique names. The distal tibia and its articular surface with the ankle joint are affected by the Pilon fracture, while the anterolateral distal tibial epiphysis is affected by the Tillaux fracture. Internal fixation and open reduction are the most common treatments for distal tibial fractures.
Danis-Weber categorization
the types of the Danis-Weber categorization are as follows,
- Type A: lateral malleolus fracture located distal to the syndesmosis
- Type B: breakage of the fibula closest to the syndesmoses
A bone density test is the most popular test used to evaluate the condition of your tibia. A bone density test uses low doses of X-rays to gauge how strong your bones are.
Diagnosis of the tibial pathological condition
If you had a tibial fracture, imaging tests such as the following may be recommended by your surgeon or healthcare provider:
- radiography. or it is called as x ray as investigation to find out if there is any crack or other tumors or any pathologies in the bone which known as tibia
- Imaging with magnetic resonance (MRI). Additionaly to find out if there is any soft tissue means muscle or ligament injuries in the structures which is visible in the Imaging with magnetic resonance (MRI)
- CT scan. ct scan is also known as computed tomography for other extra and accurate diagnosis of fracture, tumors or any other pathologies in bone.
Keeping the tibia healthy bone and prevent from breaking
- Wear your seatbelt at all times, dont remove it. It might help one with prevention in case of accidents.
- Wear safety gear when participating in all sports and activities. all sports person must have wear it to prevent any injuries during the game.
- Eat that has fiber in its content. Ask about it to dietition and eat the food they reccomend to it to get your tibia or any bone of the body healthy in nature so it prevent injuries.
- Make use of either a can or a walker if needed. Using of it have benifit in prevent injuries.
Summary
- Your shinbone is called the tibia. Being the second longest bone in your body, it plays a crucial role in your capacity to move and stand. Numerous significant muscles, tendons, nerves, and ligaments are also supported by your tibia. tibia is the second larger and stronger bone of the body which make it benefited from prevention from injuries or any pathology.
- It is a bone with a strong component and has a weight-bearing surface in the lower limb along with fibula bone in the extremities of the body.
FAQs
The tibia, which is the second-largest bone in the body, is primarily used in the leg for weight bearing, with the medial portion of the tibia supporting the majority of the stress.
The most frequently broken long bone in the body is the tibia.
open reduction and internal fixation (ORIF)
The tibia, the second-largest bone in the body, is primarily used in the leg for weight bearing, with the medial aspect of the tibia supporting the majority of the weight load.
If your tibia is fractured, it’s unlikely that you’ll be able to walk, stand, or bear weight on your leg. It’s crucial that you don’t try to “play through the pain” or ignore any symptoms because it involves weight bearing.
Congenital short tibia, another name for tibial hemimelia, is a birth abnormality in which all or a portion of the tibia (shinbone) is absent.
There are three bones in the knee: The thigh bone, or femur, is part of the upper leg. tibia, also known as the shin bone, is the bone in front of the lower leg. The kneecap, or patella, is the thick, triangular bone that rests on top of the other bones at the front of the knee.
Your tibialis anterior muscle gradually weakens as a result of tibial muscular dystrophy. It is brought on by a mutation in a particular gene that codes for a protein required for healthy muscle function. Orthotic devices, surgery, physical therapy, and strengthening exercises are available as forms of treatment.
For boys, this begins at bone age 13, while for girls, it begins at bone age 11. this is the accurate age for growth of bone in genere specific.
References
TeachMeAnatomy. (2020a, June 30). The tibia – proximal – shaft – distal – TeachMeAnatomy. https ://teachmeanatomy.info/lower-limb/bones/tibia/
Bourne, M. (2023, August 8). Anatomy, bony pelvis and lower limb: tibia. StatPearls – NCBI Book shelf. https ://www.ncbi.nlm.nih.gov /books/ NBK526053 /
Professional, C. C. M. (n.d.-u). Tibia. Cleveland Clinic. https://my.clevelandclinic.org/healt h/body/ 23026- tibia
Vasković, J., MD. (2023, November 3). Tibia. Kenhub. https ://www.kenhub.com/en /library / anatomy/tibia
Wikipedia contributors. (2023g, December 9). Tibia. Wikipedia. https://en.m.wikipedia.org/wiki/Tibia
The Editors of Encyclopaedia Britannica. (2023b, December 4). Tibia | Definition, Anatomy, & Facts. Encyclopedia Britannica. https://www.britannica.com/science/tibia
Tibia. (n.d.) . Physiopedia. https://www.physio-pedia.com/ Tibia
Staff. (2022, September 16). Tibia (Shinbone): Definition, Location, anatomy, & Diagrams. The Skeletal System.net. https ://www.theskeletalsystem.net /leg-bone /tibia.html
Donnelly, T. M. (2004). Disease problems of Chinchillas. In Elsevier eBooks (pp. 255–265). https://doi.org/10.1016/b0-72-169377-6/50027-7
Emt-P, R. B. (2023, June 29). The anatomy of the tibia. Verywell Health. https ://www.verywellhealth.com/ tibia-anatomy-4587595#toc-associated -conditions
Grütter R, Cordey J, Bühler M, Johner R, Regazzoni P. The epidemiology of diaphyseal fractures of the tibia. Injury. 2000 Sep;31 Suppl 3:C64-7.
Hunter TB, Peltier LF, Lund PJ. Radiologic history exhibit. Musculoskeletal eponyms: who are those guys ? Radio graphics. 2000 May- Jun;20(3): 819-36.
Russo A, Reginelli A, Zappia M, Rossi C, Fabozzi G, Cerrato M, Macarini L, Coppolino F. Ankle fracture: radiographic approach according to the Lauge -Hansen classification. Musculoskelet Surg. 2013 Aug ;97 Suppl 2:S155-60.
Galbraith RM, Lavallee ME. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculo skelet Med. 2009 Oct 0 7;2(3):127-33.
Whitmore A. Osgood-Schlatter disease. JAAPA. 2013 Oct;26(10):51-2.
Tan BK, Chong S, Koh ZX, Ong ME. EZ-IO in the ED: an observational, prospective study comparing flow rates with proximal and distal tibia intraosseous access in adults. Am J Emerg Med. 2012 Oct; 30(8): 1602- 6.