Bradycardia
Table of Contents
What is Bradycardia?
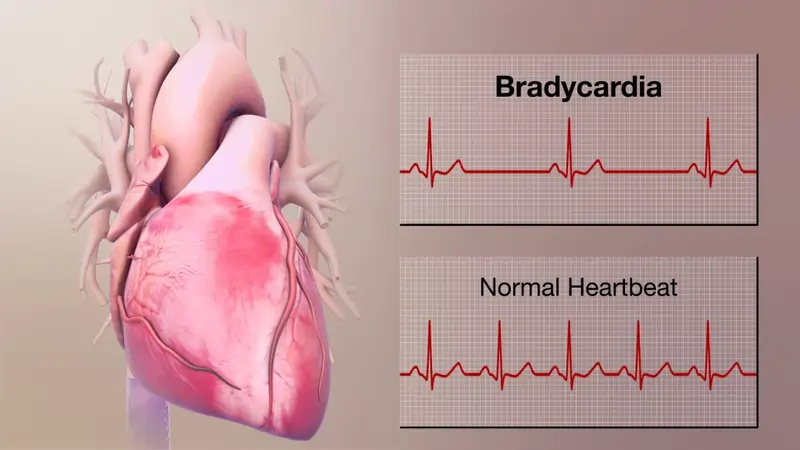
Generally speaking, a slower heart rate when you’re resting is typical. It can indicate healthy health. However, if it beats too slowly, it can be a sign of bradycardia. When you’re at rest, your heart typically beats 60 to 100 times each minute. However, it drops to less than 60 beats per minute when there is bradycardia.
Certain individuals might not have an issue with this. However, it can be a sign that something is wrong with your heart’s electrical system. You should visit a doctor so they can determine why your heart is beating slowly and whether you need treatment.
Bradycardia is a disorder where your heart beats exceptionally slowly, at less than 60 times per minute. If it prevents your heart from pumping enough blood to satisfy your body’s demands, this disease might be deadly. However, bradycardia can sometimes occur without having any negative effects, particularly in persons who are highly physically active.
How can I tell if my heart rate is bradycardia or tachycardia?
The opposite condition of tachycardia is bradycardia.
Bradycardia: The Greek words “bradys” and “cardio” are the source of the term. Together, these terms signify “slow heart.” The Greek word for tachycardia. It is made from the Greek terms “techies” and “cardio.” Together, these terms denote a “swift heart.”
Who is affected by it?
Bradycardia can affect anybody of any age or background, however, it is more frequent in persons over the age of 65. Younger individuals and children are less likely to experience it because as you age, your heart rate normally decreases. The exception is when it occurs as a result of a condition you were born with (whether genetically or not).
Additionally, it occurs more frequently in people who have specific illnesses, some of which you can inherit from your parents, or if you take specific medications. It can also occur as a result of chest traumas, nutritional issues, and eating disorders.
It may be helpful to comprehend how the heart typically beats in order to comprehend the causes of bradycardia.
The four chambers of the typical heart are divided into two atria and two ventricles. A group of cells known as the sinus node may be located in the right atrium, the heart’s upper right chamber. The natural pacemaker is the sinus node. It produces the signal for every heartbeat.
Bradycardia happens when these signals are suppressed or slowed down. Bradycardia typically starts in the heart’s sinus node area. For some people (bradycardia-tachycardia syndrome), sinus node problems can cause alternating rapid and slow heart rates.
How prevalent is this illness?
Bradycardia is a prevalent condition in persons of specific ages and under specific conditions. It most frequently happens in the following:
Those above 65. About 1 in 600 persons over 65 who have this illness experience symptoms. This indicates that more than 500,000 persons over the age of 65 experience symptoms of this illness. However, there are more persons than usual who have bradycardia but no symptoms are most likely considerably higher. When elderly persons are sleeping, bradycardia is very
prevalent.
Individuals who are highly active physically. Exercise enthusiasts may get bradycardia due to their physical fitness. The bradycardia does not impair these individuals because, while beating more slowly, their hearts pump blood more effectively and adequately for their bodies’ demands.
Bradycardia – Is it an arrhythmia?
Bradycardia, which has a slower pace than usual, is an arrhythmia (abnormal heartbeat). Adults have normal heart rates between 60 and 100 beats per minute.
When your heart beats consistently and normally, you have a sinus rhythm. Sinus bradycardia is the medical term for a regular but slower-than-normal heartbeat. For the most part, sinus bradycardia is a benign arrhythmia, especially in extremely active adults. So even if it moves more slowly than anticipated, it doesn’t cause any harm.
While bradycardia is a medical disorder in and of itself, it frequently coexists with or results from other illnesses. In those circumstances, bradycardia is frequently handled more like a symptom than a distinct illness.
What effects does this condition have on my body?
Your heart beats more slowly than the usual adult heart when you have bradycardia. When your heart’s rate is too slow pace to match your body’s need for oxygen, this becomes an issue. Your entire body is impacted by the lack of oxygen and blood flow, notably your heart and brain.
Significances
What bradycardia signs and symptoms are there?
Many persons with bradycardia have no symptoms at all. This is especially true for those with bradycardia who are also highly physically active since they have more effective hearts. People whose hearts can’t or won’t adjust typically experience the following symptoms:
- Shortness of breath.
- Chest pain (angina).
- Fatigue.
- Heart palpitations (the unpleasant feeling of your heartbeat without using your hands to feel for your pulse).
- Memory problems.
- Confusion.
- Difficulty concentrating.
- Dizziness, lightheadedness, and fainting (syncope).
- Irritability, agitation, or other personality changes.
The effects of bradycardia on the heart and the brain create these symptoms.
- Brain: The typical human brain weighs roughly 3 pounds or 1.6% of a 180-pound person’s total weight. Although it is little, your brain receives 15% to 20% of the blood that leaves your heart. Your brain’s ability to operate is affected if there is insufficient blood supply.
- Heart: The signs of bradycardia frequently resemble those of heart failure. Angina, chest discomfort, or pressure that is an indication of heart disease, can also resemble bradycardia.
What causes this medical condition?
A variety of factors can cause bradycardia. The following list contains several of the additional most typical causes.
- Deficits in electrolytes: Your heart rate might be impacted if you don’t consume enough electrolytes including calcium, magnesium, and potassium.
- Several medicines, including those used to treat cardiac irregularities and high blood pressure.
- Thyroid illness results from an imbalance of hormones in the body, which is a congenital condition or issue you have from birth.
- The condition known as obstructive sleep apnea occurs when you repeatedly stop breathing while sleeping.
- Inflammation: This includes inflammation of the pericardial sac that surrounds and cushions your heart (pericarditis), the heart muscle itself (myocarditis), or the endocardium (inner lining of the heart).
- Infections: If the bacteria that often cause strep throat infections aren’t promptly treated, they can potentially harm your heart, particularly your heart valves.
- Rheumatic heart disease and rheumatic fever: When a bacterial illness like strep throat is not treated right away, rheumatic fever may develop. A few years later, rheumatic heart disease develops as a result of rheumatic fever.
- Lyme illness: This illness is brought on by microorganisms that tick bites transmit. If you wait too long to get treatment for this infection, also known as borreliosis, your heart may suffer.
- Chagas illness: This ailment, which is similar to Lyme disease, is brought on by a parasite that you can catch from blood-sucking insects known as “kissing bugs.”
- Sinus infection syndrome: This is when the sinoatrial (SA) node, a group of cells that operates as the heart’s natural pacemaker, malfunctions.
- This implies that the electrical current that passes around your heart and forces various portions to squeeze at the appropriate times isn’t properly created by the SA node.
- Blocked heart: Any disruption in the electrical system of your heart is referred to by this general word. The electrical current’s movement is blocked or slowed down by these disruptions, which stops your heart from beating normally. In the electrical conduction system of the heart, blocks can form at several locations.
- Drugs: These include narcotic pharmaceuticals, lithium, beta-blockers, calcium-channel blockers, anti-arrhythmia drugs, lithium, and depressants, among other prescription drugs. Cannabis (marijuana), a substance used recreationally, can also induce bradycardia.
- Heart operation: Repair of inherited (or congenital) cardiac problems, valve replacement, and valve repair are all potential causes of bradycardia.
- Radiation treatment: Radiation heart disease can develop as a result of this treatment’s hazardous side effects.
Other conditions include:
- Heart attack.
- Heart failure.
- Coronary artery disease.
- Duchenne muscular dystrophy.
- Long Q-T syndrome.
- Lupus.
- Rheumatoid arthritis.
- Scleroderma.
- Injuries/trauma.
- Hypothermia (low body temperature).
- Hypothyroidism.
- Sleep apnea.
- Intracranial hypertension (excessive pressure on the brain brought on by bruising, swelling, or other conditions).
- Is bradycardia contagious?
- Bradycardia is not contagious but, several of the illnesses that cause bradycardia are contagious.
Heart block (atrioventricular block)
Bradycardia may also develop if electrical impulses from the heart’s top chambers (atria) and lower chambers (ventricles) aren’t transmitted properly. Atrioventricular block, often known as heart block, is the condition that results from this.
- There are three basic categories for heart blockages.
Heart block of the first degree. All electrical signals from the atria reach the ventricles in the mildest form, but the signal is retarded.
- First-degree heart block seldom manifests as a symptom and, in the absence of any other electrical signaling issues, typically does not require medical attention.
- Heart block of the second degree. The ventricles do not receive all electrical inputs. Dropped beats cause a slower and occasionally erratic heart rhythm.
- Heart block in the third (full) degree. The atria do not provide any electrical signals to the ventricles. The ventricles will typically beat on their own but at a very sluggish rate when this occurs.
Test and diagnosis for bradycardia
- How is it identified?
A doctor can recognize bradycardia through a physical examination along with tests that measure your heart rate and look at its rhythm.
What examinations will be performed to identify the condition?
The following are the most likely tests for bradycardia:
- Inspection of the body: A doctor will check your body during a physical examination to look for any signs of illnesses or other conditions. Any impacted regions may also be felt since certain issues result in changes that you may feel but not see.
- ECG or EKG stands for electrocardiogram. Due to its ability to pinpoint your heart’s electrical activity, this test is crucial for identifying bradycardia. Due to its ability to pinpoint your heart’s electrical activity, this test is crucial for identifying bradycardia. The electrodes used in this test attach to the skin of your chest and consist of many sensors (often 12 in number).

- On a paper printing or a computer screen, the electrodes can detect the electrical activity in your heart and display it as a wave.
Bradycardia can also be diagnosed through lab tests, the majority of which can help rule out other issues. These tests consist of:
- These tests check your blood’s levels of electrolytes, particularly calcium, potassium, and magnesium.
- Troponin: A particular kind of troponin, a protein, is present in the cells of your heart muscle. Due to its ability to pinpoint your heart’s electrical activity, this test is crucial for identifying bradycardia. The electrodes used in this test attach to the skin of your chest and consist of many sensors (often 12 in number).
- Bradycardia can also be diagnosed through lab tests, the majority of which can help rule out other issues. These tests consist of:
- These tests check your blood’s levels of electrolytes, particularly calcium, potassium, and magnesium. Levels of thyroid hormones.
Bradycardia may result from hypothyroidism (low thyroid function).
Risk factors
Bradycardia is frequently linked to cardiac illness of some kind that has damaged the heart tissue. Any factor that increases the likelihood of cardiac problems might increase bradycardia. Heart disease risk factors include:
- Older age
- High blood pressure
- Smoking
- Heavy alcohol use
- Illegal drug use
- Stress and anxiety
- Medical intervention or healthy lifestyle modifications may help reduce the risk of heart disease.
- Management and treatment
Is bradycardia curable? How is it treated?
If you have bradycardia but no symptoms, therapy is probably not necessary. Bradycardia is virtually always treatable and occasionally curable when it is present. Sometimes correcting the underlying medical illness that is causing your bradycardia will be enough to end it. When you have bradycardia as a result of a medicine you are taking is an illustration of this.
What drugs or therapies are applied?
There are primarily two approaches to bradycardia treatment.
Medication
An intravenous (IV) or injectable medicine, such as atropine, can make your heart beat more quickly if bradycardia is causing serious issues, such as dangerously low blood pressure. Because patients receiving these drugs may need monitoring along with additional care, treatments like these are often hospital-specific.
To assist enhance heart function, including how forcefully your heart beats or your heart rate, you can also take drugs orally on a daily basis.
Temporary pacing
This entails a piece of equipment having electrical connections that come into contact with or are attached to your chest skin.
Your heart will beat as a result of these connections allowing a small electrical charge to enter your body. Temporary cardiac pacing is a successful short-term therapy for patients who require a permanent pacemaker or whose bradycardia is anticipated to be transient.
Permanent pacemaker
For many people, a permanent pacemaker is the most efficient treatment for bradycardia. When your heart’s natural pacemaker cells are malfunctioning, as is the case with disorders like sick sinus syndrome, this is very effective.
A permanent pacemaker can treat this issue over the long term and prevent problems from developing, even if it cannot completely cure it. The majority of pacemakers have a lifespan of several years, and some of them contain batteries that may last for almost ten years.
In order to install the pacemaker device, which will send electrical pulses to your heart muscle, you will often need surgery. An electrophysiologist or surgeon will create a tiny pouch beneath your skin during this surgery, which is where the pacemaker will go. Then, they will attach cables, sometimes known as leads, to various places in your heart.
Surgery to implant a pacemaker may be avoided for certain patients. This is due to the availability of more recent catheter-based leadless pacemakers that can be implanted to treat bradyarrhythmias. During this surgery, a doctor makes an incision into a significant blood artery and inserts a tube-like catheter device. Once inside your heart, the pacemaker can be implanted by the provider by guiding the catheter there.
What are the potential bradycardia risks, side effects, of treatments?
Bradycardia complications are more likely to occur when this problem is left untreated for an extended period of time. Because of this, rapid identification and treatment are crucial.
Depending on the medications you get or are already taking, there are a wide range of potential side effects or consequences from medicine. The ideal person to respond to this query is your healthcare practitioner since they can specifically address your position, requirements, and circumstances in their response.
How can I regulate my symptoms or take care of myself?
You shouldn’t try to treat bradycardia by yourself without assistance from a healthcare professional. If you think you might have it, you should visit your doctor as soon as possible.
How soon will I recover following treatment?
If bradycardia is treated, you should start to feel better as soon as it is applied. Numerous drugs (particularly IV medications) used to treat this illness begin to operate fast. If you require a pacemaker, your symptoms should improve right away following surgery, and as you recuperate, you should feel better all around.
After having a pacemaker implanted, most patients recover within a few weeks. The best person to provide you with further information about what to anticipate and how long it can take you to recover is, however, your healthcare physician.
Prevention
Can I lower my chances of acquiring bradycardia or avoid it?
Many people are unable to prevent bradycardia. This is especially true when it comes to bradycardia, which develops as you age naturally or because you’re in excellent physical form.
Bradycardia may only be avoided when one of the following factors occurs:
- Drug usage for fun: You don’t use these medications for any medical purpose, and they are not prescribed to you. You can prevent getting bradycardia by refraining from using recreational drugs, particularly opioids and cannabis-based substances.
- Nervosa anorexia: Receiving treatment can help people with anorexia nervosa prevent long-term problems like bradycardia.
- Bradycardia occurs unexpectedly in all other circumstances. You can’t stop it from happening since you can’t tell when it’ll happen.
- However, despite their efforts to lower their risk, many people will still have bradycardia as a result of aging.
It’s important to follow the instructions on all prescriptions since some medications, especially those used in big doses, may cause bradycardia. Despite the fact that bradycardia is frequently not preventable, doctors offer advice on how to reduce the likelihood of developing cardiac issues.
Follow these heart-healthy recommendations:
- Exercise often: Your doctor may offer advice on the optimum type and amount of exercise for you.
- Adopt a balanced diet: Consider a diet that is well-balanced, heavy in fruits, vegetables, and whole grains, and low in fat, salt, and sugar. Keep a healthy weight. Having more weight and having a high BMI ratio raises your risk of heart disease.
- Maintain healthy cholesterol and blood pressure levels: Adapt your lifestyle and take your medications as directed to control your high blood pressure, diabetes, and cholesterol.
- Avoid smoking: Discuss tactics or programs with your healthcare physician if you need assistance quitting.
- If you choose to drink, do so sparingly. If you choose to drink, use it cautiously. Accordingly, healthy adults can consume up to one drink for women and two for men each day. Talk to a healthcare professional about a program to stop drinking and regulate other alcohol-related behaviors if you are unable to manage your alcohol use.
- Stress management: Strong emotions have the potential to slow heart rate. Some approaches to lower stress include regular exercise, joining a support group, and trying out relaxation techniques like yoga.
- Attend your regular checks: Have routine physicals and notify your doctor of any symptoms or indicators.
Perspective/prognosis
What can I look for if this is my condition?
Bradycardia frequently has no symptoms and poses no health risks. This is especially true for bradycardia patients since they are in good physical condition.
Early identification and treatment increase the likelihood of a successful result for those who do have symptoms or issues related to bradycardia. Delayed treatment often increases your risk of complications or death, particularly when bradycardia occurs as a result of certain diseases.
What is the duration of bradycardia?
Bradycardia might be a temporary issue or a chronic one. How long it lasts typically depends on the underlying reason. When bradycardia is brought on by drugs (recreational or prescribed) or other transient situations, it is more likely to be a short-term issue.
In general, the best person to tell you whether or not this issue will be a temporary problem or whether you’ll have it for the rest of your life is your healthcare professional. You usually need to take medicine every day or undergo surgery to implant a pacemaker if you have symptoms that you will have for the rest of your life.
Life with bradycardia
How can I take care after myself?
If you experience symptoms together with bradycardia, you should:
- Get assistance from your healthcare practitioner. To obtain the greatest advice on how to take care of yourself, you must speak with your healthcare practitioner.
- Take the prescribed prescription: Take your medicine as directed if you have bradycardia and take medication for it. If you have any questions or concerns, you may also ask your doctor for further details on the best way to take your drugs.
- Consult your healthcare physician if advised to do so. When your doctor suggests it, you should visit them if you have bradycardia but no symptoms. Long-term monitoring of your health can help you see any possible dangerous symptoms earlier.
When should I visit my doctor or when should I get medical attention?
Regardless of whether you have bradycardia or not, you should schedule an annual physical with your doctor at least once a year. This annual checkup is crucial for helping your doctor identify a variety of healthcare issues early, particularly those that lack obvious symptoms.
You should consult your doctor if you experience any new symptoms or any changes in your general health if you have bradycardia but no symptoms. If you do experience symptoms, you should also visit your doctor if you observe a change in your symptoms, especially if it interferes with your normal activities.
When should I visit the emergency room of the hospital?
If you get bradycardia symptoms right away, or if they worsen or change abruptly, you should visit the hospital.
Additionally, if you have any of the following symptoms—which can potentially be indications of far more serious conditions like a heart attack—you should visit the hospital as soon as possible:
- Chest pain (angina).
- Shortness of breath (dyspnea).
- Dizziness, lightheadedness, and fainting (syncope).
Summary
Bradycardia is a condition that, depending on the circumstances, may not always cause symptoms or problems. Even so, it’s acceptable to have anxiety or worry if you have unresolved questions or the possibility of future issues. Bradycardia is fortunately a disorder that is usually always curable. Your healthcare practitioner can also provide you with suggestions and counsel that will help you get ready for the challenges you’re experiencing and the future.
FAQs
Why does bradycardia occur? Some people can have bradycardia, especially if they are very physically fit. However, other factors can also contribute to it, including myocarditis, cardiomyopathy, aging-related cardiac damage, and disorders including heart attacks.
When adults are at rest, their hearts normally beat between 60 and 100 times per minute. If you have bradycardia, your heart beats less often than 60 times per minute. Bradycardia can be a major issue if the heart isn’t supplying the body with enough oxygen-rich blood and the pulse is extremely sluggish.
Adults should maintain a heart rate between 60 and 100 beats per minute. When your heart beats consistently and normally, you have a sinus rhythm. Sinus bradycardia is the medical term for a regular but slower-than-normal heartbeat. For the most part, sinus bradycardia is a benign arrhythmia, especially in extremely active adults.
A heart rate below 60 beats per minute is the major sign of bradycardia. The brain and other organs may experience oxygen deprivation as a result of this unusually low heart rate, which may result in symptoms like fainting. Dizziness.
A pacemaker implant, medication changes, or lifestyle changes are all potential treatments for bradycardia. Bradycardia may be alleviated by treating the underlying medical condition that is causing the sluggish heartbeat, such as thyroid illness or sleep apnea.
To diagnose sinus bradycardia, an ECG with a normal sinus rhythm and a heartbeat less than 60 bpm is required. Whenever a typical sinus rhythm meets the parameters listed below: Every QRS is preceded by a P wave in a regular pattern. The P wave in leads 1 and 2 is vertical; the P wave in V1 is biphasic.