Dysphonia (Hoarse voice): When Your Voice Takes a Wrong Turn
Table of Contents
What is Dysphonia?
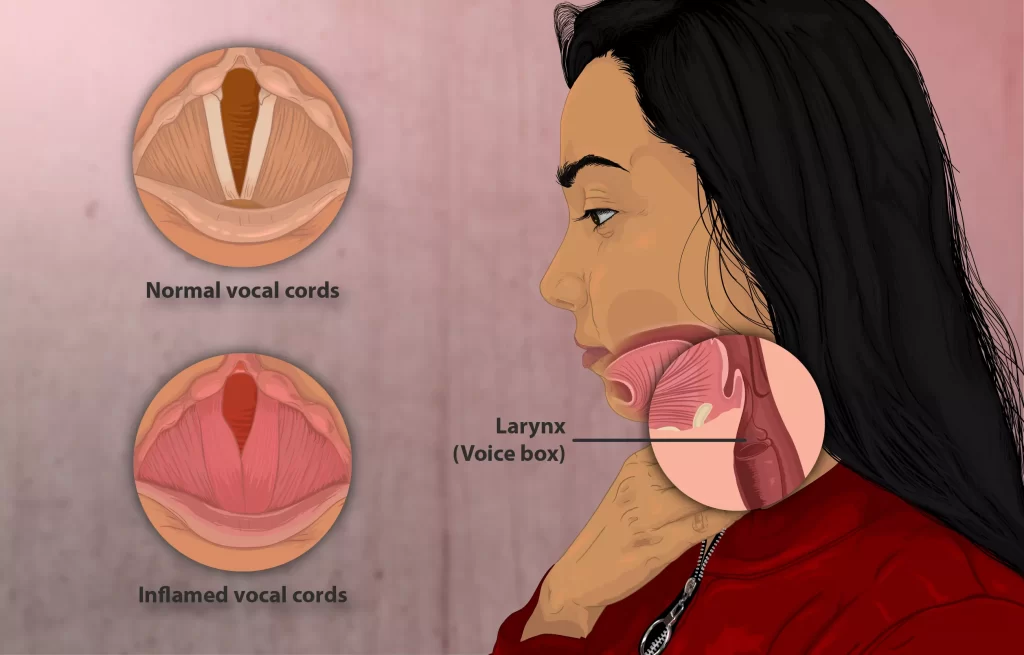
The disorder known as dysphonia, or hoarseness, affects the quality of your voice. It sounds like the instruments in your voice, your vocal cords, are out of tune, producing a variety of disagreeable noises.
A hoarse voice, sometimes referred to as dysphonia or hoarseness is caused by an involuntary breathy, raspy, or strained voice that is lower in pitch or volume. An uncomfortable or scratchy feeling in the throat might be linked to a hoarse voice. Vocal fold issues in the larynx are frequently the cause of hoarseness.
Laryngitis, which can be brought on by allergies, a cold, or an upper respiratory infection, could be the cause. Temporary hoarseness can also result from loud cheering at athletic events, speaking loudly in noisy environments, talking for extended periods without pausing, singing loudly, and speaking in an unnaturally high or low pitch.
A hoarse voice is sometimes referred to as dysphonia or hoarseness, There are also additional reasons why people lose their voice, and the usual course of treatment is to cure the underlying problem and rest the voice. Drinking lots of water can help if the issue is caused by vocal abuse or overuse.
It appeared to affect women and older people more frequently. Additionally, there is a higher risk for some occupational categories, such as singers and teachers.
What are the Types of Dysphonia?
There are two main types of voice disorders: biological and functional.
The reason for organic dysphonia, which arises from a physiological alteration in one of the speech subsystems (for voice, typically breathing, laryngeal architecture, and/or other portions of the vocal tract are affected), is what separates these major divisions from one another.
Function dysphonia, on the other hand, is the term used to describe hoarseness brought on by excessive or abusive vocal use. Furthermore, structural and neurogenic dysphonia are two categories into which organic dysphonia can be classified by the ASHA; neurogenic dysphonia is characterized as decreased vocal structure functioning as a result of a neurological issue (in the central nervous system or peripheral nervous system).
Psychogenic dysphonia is another subtype of functional dysphonia that has been recognized by experts. It is characterized as a vocal disorder without a known cause that is assumed to be the result of mental stresses in one’s surroundings.
It is noteworthy that there is significant overlap between these kinds and that they are not mutually exclusive. For instance, there are numerous causes of Muscle Tension Dysphonia (MTD), such as organic pathology-related MTD (also known as the organic type), vocal use-related MTD (also known as the functional type), and psychological or personality-related factors (also known as the psychogenic type).
Natural dysphonia
- Acute laryngitis (bacterial or viral) – (Persistent: GERD, LPR, smoking)
- Neoplasm (dysplasia, premalignant form) – Squamous cell carcinoma is a malignant tumor.
- Trauma (Iatrogenic: intubation, surgery) – (Unintentional: sharp, piercing, heat)
- hormonal (the condition, hypothyroidism)
- Amyloidosis in the bloodstream Iatrogenic (from inhaled corticosteroids)
Dysphonia functional
- Misuse of psychogenic voice
- idiopathic
What are the Causes of Dysphonia?
The most frequent causes of hoarseness are functional dysphonia (30%) and laryngitis (acute 42.1%; chronic 9.7%). Additionally, laryngeal tumors (malignant 2.2 – 3.0%; benign 10.7 – 31% ) can induce hoarseness. Neurogenic disorders (2.8 – 8.0%), psychogenic conditions (2.0 – 2.2%), and aging (2%), on the whole, are less common causes.
Dysphonia can be brought on by several different factors that create irregular vibrations of the vocal folds. These factors can include everything from systemic illnesses to verbal abuse and misuse. Five broad categories can be used to categorize causes of dysphonia.
Neoplastic/structural: Tissue growth abnormalities of the vocal folds.
- Dysplasia
- cysts
- Polyps
- Nodules
- Cancer
Inflammatory: Tissue alterations brought on by inflammation in the vocal folds.
- Allergies
- infections
- Backflow
- Consuming tobacco
- Trauma
- verbal mistreatment
Neuromuscular: Any disturbances in the neural system parts that regulate the function of the larynx.
- Multiple Sclerosis
- Myasthenia Gravis
- Parkinson’s Disease
- Sporadic Dysphonia
- damage to the nerves
Related Systemic Disorders: Voice-related symptoms can be indicative of systemic disorders.
- Acromegaly
- Amyloidosis
- Hypothyroidism
- Sarcoidosis
Technical: Linked to inadequate muscular function or psychological strain, without any accompanying physiological irregularities in the larynx.
- Psychogenic such as dissociation disorder
- Excess demands
- Stress
- Vocal strain
Misuse of the voice: People who depend largely on their voice, such as singers and teachers, are prone to vocal misuse, which can lead to weariness and inflammation.
Acid reflux: Vocal cord irritation from stomach acid applying into the larynx can cause hoarseness
Employment
According to certain theories, some occupational groups may be more susceptible to dysphonia because of the high vocal demands of their jobs. Teachers and singers have been the main subjects of research on this topic, while some studies have looked at other groups of people who use their voices a lot, such as actors, cheerleaders, aerobic instructors, etc.
Currently, it is recognized that dysphonia is a common complaint among teachers and vocalists. Educators who teach physical education, work in noisy settings, or speak loudly out of habit are also more vulnerable.
Dysphonia clericorum, often known as clergyman’s throat, was the name used in the past to describe excruciating dysphonia connected to public speaking, especially among preachers. However, because different research has used substantially diverse approaches to acquire data (e.g., using different operational definitions for “singer”), the precise prevalence rates among occupational voice users are uncertain.
Mechanism
The larynx, sometimes referred to as the voice box, is a structure that contains the vocal folds and is situated in the front region of the neck. It is made up of many supporting cartilages and ligaments. Exhaled air from the lungs travels up the vocal tract during regular voice production.
The vocal folds at the larynx migrate toward the tract’s midline as a result of the air exhaled (a process known as adduction). The adducted vocal folds stay partially open rather than shut entirely. The glottis is the name given to the little space between the folds.
The vocal folds vibrate as a result of the air particles being distorted as they pass through the glottis. Voice, or phonation, is produced by this vibrating motion. The ability to create a suitable level of phonation is impaired in dysphonia. More precisely, it stems from a dysfunction of the larynx’s nerve supply or vocal fold vibration.
Dysphonia VS Dysarthria
| Feature | Dysphonia | Dysarthria |
| Focus | Voice quality | Speech coordination and control |
| Cause | Overuse of voice, lumps, infections, neurological problems, and psychological aspects | harm to the nervous system |
| Symptoms | Breathiness, hoarseness, and vocal weakness | slurred speech, muffled noises, and unusual volume or pitch |
| Treatment | Surgery, voice therapy, and vocal hygiene (sometimes) | Speech therapy, assistive technology |
How to diagnose Dysphonia?
A multidisciplinary team, including an otolaryngologist (a specialist in the ears, nose, and throat) and a speech-language pathologist, completes the assessment and diagnosis of a dysphonic voice. This process involves the use of both objective and subjective measures to evaluate the vocal fold tissue’s condition and vibration patterns, in addition to the voice’s quality.
For instance, an excessively high or low voice can indicate aberrant pitch, while an excessively quiet or loud voice can indicate abnormal loudness. Similarly, repetitive (i.e., very flat) or inappropriately fluctuating voices indicate abnormal variability, whereas frequent, inappropriate gaps indicate abnormal quality. Although the terms dysphonia and hoarseness are frequently used interchangeably, it’s vital to understand that they are not the same thing.
The term “hoarseness” is only used to describe how someone perceives the sound or perceptual quality of a dysphonic voice. While hoarseness is a typical dysphonia symptom (or complaint), additional indications and symptoms may also exist, including breathiness, roughness, and dryness. Moreover, a voice can be labeled as dysphonic if it interferes with an individual’s ability to meet their functional or occupational needs or if it is unsuitable for their age or sex.
Auditory-perceptual measures
Because they are quick and non-invasive, auditory-perceptual measurements are the most often utilized method by physicians to assess voice quality. In addition, in a therapeutic context, these metrics showed their reliability. A patient’s voice quality is rated for several characteristics, such as overall severity, breathiness, roughness, strain, volume, and pitch.
These assessments are carried out when a person speaks freely, reads a sentence or paragraph aloud, or produces vowels repeatedly. Two official voice rating scales that are frequently used for this purpose are the CAPE-V (Consensus Auditory Perceptual Evaluation—Voice) and the GRBAS (Grade, Roughness, Breathiness, Asthenia, Strain).
Vocal fold imaging
Clinicians can diagnose vocal pathology and evaluate the quality of the vocal fold vibrations by using vocal fold imaging techniques to analyze the vocal folds. The main clinical tool utilized for this is laryngeal stroboscopy.
Using a rigid or flexible laryngoscope and synchronized flashing light, laryngeal stroboscopy creates an image of the motion of the vocal folds; however, this image is not produced in real time because it is averaged over multiple vibratory cycles. Patients with moderate to severe dysphonia are not candidates for this treatment since it depends on periodic vocal fold vibration.
While laryngeal stroboscopy, high-speed digital imaging of the vocal folds (videokymography) is not constrained by the same factors.
Images are captured at a rate of 8000 frames per second using a rigid endoscope, and the images are shown instantly. Additionally, this method enables the imaging of aperiodic vibrations, making it applicable to individuals exhibiting dysphonia in all severity levels.
Acoustic measures
Vocal function can be objectively measured with the use of acoustic measurements. Algorithms for signal processing are used on voice recordings captured either spontaneously or during prolonged phonation. Then, fundamental frequency, signal amplitude, jitter, shimmer, and noise-to-harmonic ratios are among the acoustic properties that can be investigated. However, individuals with severe dysphonia cannot use these measurements because of limits established by the algorithms used.
Aerodynamic measures
Measures of air volume, airflow, and subglottal air pressure are examples of aerodynamic voice measures. Individual differences in the normal aerodynamic properties of voice result in a wide range of values that overlap between dysphonic patients and those who are not. This restricts the measures’ applicability as a diagnostic tool. However, they can be a helpful supplementary tool in conjunction with other voice assessment tools, or they can be used to track the effectiveness of therapy over time.
What is the Treatment of Dysphonia?
Voice disorders can be categorized into different categories, such as organic (structural or neurogenic), functional, neurological (psychogenic), or iatrogenic, even though there is no universal classification for voice issues.
There exist a variety of therapy options that might be suggested to the patient, contingent on the diagnosis, severity, and classification of the voice disorder. Professionals must remember that no one treatment works for everyone. Instead, a clinical approach must determine what the best course of action is for that specific patient.
There are three primary categories of treatment: voice therapy, surgery, and medicine. Certain voice abnormalities require a combination of treatment modalities when appropriate. For example, anti-reflux medications or botulinum toxin (botox) are used as part of a medical treatment. One important treatment for voice problems like spasmodic dysphonia is Botox. Patients who have an underlying cause of voice abuse or misuse are the primary candidates for voice therapy. In addition, laryngologists advise patients to undergo this kind of treatment for functional dysphonia and organic voice disorders, such as vocal fold nodules, cysts, or polyps.
Additionally, some surgical procedures can be used, such as laryngeal framework surgery, which involves manipulating the voice box, phono microsurgery, which involves removing vocal fold lesions under a microscope, and injection augmentation, which involves injecting a material into the vocal folds to increase closure. Patients with organic dysphonia may benefit from surgical interventions.
Dysphonia may be treated by a combination of indirect treatment (an approach that modifies external factors affecting the vocal folds) and direct treatment (an approach that focuses primarily on mechanisms operating during the use of the vocal folds, such as respiration or phonation).
Direct therapies
Direct therapies focus on the vocal production’s physical components. Methods can be used to control breathing patterns, alter laryngeal tension, or alter vocal fold contact. The yawn-sigh method, ideal pitch, laryngeal manipulation, humming, the accent approach, and the Lee Silverman Voice Treatment are a few notable methods. Circumlaryngeal manual treatment, which has been utilized to ease tension and massage the hyoid-laryngeal muscles, is an illustration of direct therapy.
Chronic elevation of the larynx causes tension in this area frequently. The patient is made to hum or hold a vowel while pressure is applied to certain locations. Dysphonia caused by muscular strain is frequently treated with traditional voice treatment.
Indirect therapies
External variables that could affect vocal production are taken into consideration in indirect therapy. This includes refraining from damaging vocal behaviors as well as upholding vocal hygiene standards. Proper hydration of the vocal folds, monitoring voice use and rest, refraining from vocal abuse (e.g., shouting, clearing the throat), and considering lifestyle decisions that may impact vocal health (e.g., smoking, sleeping habits) are all examples of vocal hygiene.
Before engaging in demanding vocal exercises, vocal warm-ups, and cool-downs can be used to enhance muscle tension and reduce the chance of damage. It should be remembered that vocal hygiene techniques by themselves only have a limited therapeutic impact on dysphonia; as such, they should be combined with other interventions.
Medication and surgery
Organic dysphonias have been indicated for treatment using medical and surgical interventions. Botulinum toxin injection is a useful treatment for spasmodic dysphonia, which is a condition in which the vocal folds hyper-adduce sound waves that cause hoarseness on occasion. The thyro-arytenoid muscle’s acetylcholine release is blocked by the toxin.
While the use of botulinum toxin injections is thought to be rather safe, patients respond differently to treatment at first; some have reported negative effects from the injections, including difficulty swallowing and breathy voice quality. Males may have breathiness for a longer duration than females.
How can I Prevent Dysphonia?
studies on prevention have been carried out since some professions—such as teaching—are more susceptible to acquiring dysphonia. The effectiveness of dysphonia preventive techniques has not yet been conclusively proven, however research is constantly being conducted in this area.
Professionals have identified two main forms of vocal training that can aid in prevention: direct and indirect. While indirect prevention strategies refer to modifications to the underlying physiological mechanism for voice production (e.g., altering postural habits, respiratory training, modifying how vocal fold adduction occurs), direct prevention refers to efforts to decrease conditions that may serve to increase vocal strain (e.g., patient education, relaxation strategies, etc.).
Differential Diagnosis
- Acute laryngitis (42.1%)
- Chronic laryngitis (9.7%)
- Functional dysphonia
- Muscle tension dysphonia
- Benign lesions
- Vocal fold nodules
- Vocal fold cysts
- Malignant tumors
- Squamous cell carcinoma
- Lymphoma
- Neurological conditions
- Multiple sclerosis
- Vocal tremor
- Laryngeal dystonia/Spasmodic dysphonia
- Parkinson’s disease
- Amyotrophic lateral sclerosis
- Myasthenia gravis
- Systemic conditions
- Hypothyroidism
- Rheumatoid arthritis
- Systemic lupus
- Wegener’s granulomatosis
- Sarcoidosis
- Amyloidosis
- Tuberculosis
- Aging
What is the Prognosis of Dysphonia?
Depending on the underlying ailment, persons with dysphonia may have varying prognoses. The prognosis for a patient might vary from bad to good. Individuals who simply need symptomatic treatment for acute laryngitis will often recover in one to three weeks.
In the meantime, voice rest and/or multiple speech therapy sessions may be necessary for individuals with muscular tension dysphonia, vocal fold nodules/polyps, or other functional dysphonia to see improvement in symptoms.
Patients with late-stage laryngeal cancer had 5-year survival rates ranging from 30% to 63%, with metastasis being the most common cause of death. Up to 95% of patients with early-stage laryngeal carcinoma have survived for five years. The importance of diagnosing laryngeal cancer early is highlighted by the significant disparity in prognosis between early and late-stage cases.
What is the Complication of Dysphonia?
Excessive secretions, paraglottic hemorrhage, bleeding, postoperative hematoma, and edema are among the complications that might arise from injecting any kind of material into the vocal fold. These complications are usually caused by the difficulty of fully viewing the vocal folds. Aspiration and airway impairment are uncommon side effects of vocal fold injections, with reported rates of less than 5%.
A tracheostomy may be necessary owing to airway blockage, implant migration or extrusion, inadequate medialization, infection, postoperative hematoma, edema, and the necessity for revision surgery are among the complications associated with laryngeal surgery, including treatments to medialize the vocal fold.
How to Educate Patients of Dysphonia?
Patients who exhibit chronic hoarseness or who have risk indicators such as aspiration, worsening dyspnea, and/or weight loss should be considered for laryngeal cancer. To rule out malignancy, clinicians should consult with an otolaryngologist for additional referral.
Patients should consult their physician if they continue to experience dysphonia that does not go away after four weeks or gets worse. The first line of treatment for muscular tension dysphonia and benign laryngeal lesions is frequently voice rest and speech therapy.
Enhancing Healthcare Team Outcomes
Up to one-third of adults may suffer from dysphonia, a prevalent condition. Healthcare professionals must acknowledge that dysphonia could be a symptom of an underlying disease that needs to be evaluated further and treated right away.
Patient results may suffer if the larynx is not evaluated as soon as possible due to delayed cancer diagnosis. Dysphonia could be the initial sign of a neurological problem that has to be further examined by a neurologist.
Conclusion
Silence may be joy, but not if it becomes difficult for you to speak, sounds different, or disappears completely from your voice due to hoarseness. If your hoarseness persists for more than three weeks, you should see a doctor.
You should also get help if you lump your neck, are having trouble breathing or swallowing, are coughing up blood, or haven’t been able to use your voice in a few days. Your physician will investigate the cause of your hoarseness and assist you in regaining your voice.
FAQ
Types of Medications That Can Change Your Voice
Antidepressants.
Muscle relaxants.
Diuretics.
Antihypertensives (blood pressure medication)
Antihistamines (allergy medications)
Anticholinergics (asthma medications)
High doses of Vitamin C (> 5 grams per day)
Yes, it can occur. Stress is one of the primary reasons for MTD. When we talk about stress, one of the similar phrases used is “feeling uptight”.
There is proof supporting an association between depression and anxiety in patients with chronic disorders. Spasmodic dysphonia (SD) is a chronic, not curable, and disabling voice disease. Reported values of depression and anxiety in SD range from 7.1% to 72%, with a maximum number of 18 patients.
Spasmodic dysphonia can be inherited, or it may happen after an injury to the voice box like an injury or a severe cold. Diagnosis of Spasmodic dysphonia depends on an exam by a multidisciplinary team, involving an otolaryngologist.
It has been estimated that more than 70% of patients with Parkinson’s disease feel voice and speech diseases. Few report that dysphonia, impairment in the ability to speak simply, is one of the disorder’s most minor symptoms.
References
- Hoarse voice. (2023, December 13). In Wikipedia. https://en.wikipedia.org/wiki/Hoarse_voice
- Neighbors, C. (2022, May 1). Dysphonia. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK565881/
- Professional, C. C. M. (n.d.). Hoarseness. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17105-hoarseness