Active Cycle Of Breathing Technique (ACBT)
Table of Contents
Introduction
The Active Cycle of Breathing Techniques (ACBT) is a patient-performed active breathing method that can be used to mobilize and remove excess pulmonary secretions as well as enhance overall lung function. It is a versatile therapy strategy that may be utilized in conjunction with positioning and is adaptable to most individuals.
Depending on the patient’s situation, each component can be utilized alone or as part of the ACBT cycle. After learning ACBT, the patient can be encouraged to utilize it alone, without the supervision of a physiotherapist.
There is no need for any specific equipment for this activity.
It’s used to:
- Clear and loosened pulmonary secretions. This lowers the chance of chest infections.
- Improve pulmonary ventilation.
- Increase the efficacy of your cough.
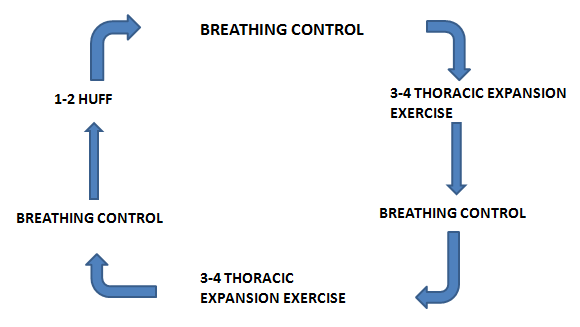
ACBT consists of three main phases:
- Breathing Control
- Deep Breathing Exercises or Thoracic Expansion Exercises
- Huffing or Forced Expiratory Technique (FET)
The approach can be changed depending on the patient’s condition. Additionally, if and when needed, a manual method (MT) or positive pressure can be used to produce a more complicated cycle to aid in the elimination of secretions in the lungs. Percussion or expiratory vibrations may be included.
Randomized controlled research found that the active cyclic breathing method, along with routine chest physiotherapy, improved arterial oxygenation, heart rate, and pain perception after Coronary Artery Bypass Surgery (CABG).
Breathing Control
Breathing control is used to relax the airways and ease symptoms such as wheezing and tightness that might arise after coughing or being out of breath. It is the interval of respite between the more active aspects of the approach. Allowing the patient to close their eyes while controlling their breathing might also assist in creating calm. Breathing control is essential in between the more vigorous ACBT exercises because it allows the airways to relax.
Breathing Control can also assist if you have shortness of breath, fear, bronchospasm, anxiety, or are in a panic. The time spent exercising breathing control may vary depending on how out of breath the patient is.
When employing this approach with a patient as part of ACBT, the patient is normally asked to take six breaths.
Instructions to patient:
If you can, softly inhale and exhale via your nose. If you cannot, breathe through your mouth instead(the patient breathes according to his rate).
It’s preferable to practice breathing control with “pursed lips breathing” if you exhale through your mouth.
With each exhalation, try to relax your shoulders and release any tension in your body.
Gradually try to make the breaths slower.
Breathing control should be maintained until the person feels ready to go on to the next stage of the cycle.
Deep Breathing Exercises or Thoracic Expansion Exercises
Deep breathing/thoracic expansion exercises are deep breathing exercises that focus on inspiration and aid in the loosening of pulmonary secretions.
Active inspiration is frequently followed by a three-second end-inspiratory hold before a passive, comfortable, and unforced expiration.
Instructions to patient:
Maintain a relaxed chest and shoulders.
Take a long, slow, and deep breath in, preferably via your nose.
Hold the air in your lungs for 2-3 seconds after your inhalation before exhaling (this is known as an inspiratory hold).
Breathe out gradually and relax, as if sighing.
Repeat 3–5 times more. If the patient becomes dizzy, they must return to the breathing control phase of the cycle.
Proprioceptive input with the therapist or patient placing their hands on the thoracic cage can help with maximum inspiration.
This has been linked to more chest wall movement and better ventilation.
To compensate for asynchronous ventilation that may occur in some respiratory disorders due to sputum retention and/or atelectasis, a breath hold might be added to the deep breath.
Huffing or Forced Expiratory Technique
This is a strategy for moving secretions downstream towards the mouth that have been mobilized by deep breathing/thoracic expansion exercises. Instead of coughing, a huff is released via an open mouth and throat. Huffing assists in moving sputum from the small airways to the larger airways, where it is eliminated by coughing while coughing alone cannot remove sputum from the small airways.
The patient is initially taught to take a medium breath in and a medium breath out with mild to moderate effort and protracted expiratory flow, with the glottis open. The duration of the huff and the power of contraction of the expiratory muscles should be adjusted to optimize secretion clearance by increasing airflow.
There are two types of huff:
- Medium Volume Huff
- High Volume Huff.
Medium Volume Huff
This promotes the passage of lower-level secretions through your airways.
Take a normal-sized breath in, followed by an energetic, lengthy breath out until your lungs are empty. Let’s pretend you’re attempting to steam a mirror.
High Volume Huff
Take a big breath in, open your lips wide, and immediately puff out.
Only puff 1-2 times simultaneously, as huffing continuously might cause your chest to tighten.
When you huff, listen for crackles. If you hear them, you may need to cough and clear secretions; attempt to spit them out into a tissue or a cup.
A sputum bowl. Avoid coughing excessively since this may limit the effectiveness of the approach and make it too tiresome.
Repeat for about 10 minutes, or until the chest feels clearer.
Small lengthy huffs transport sputum from the lower chest to the upper chest, whereas huge short huffs transfer sputum from the upper chest to the lower chest, so utilize both.
Coughing
If puffing alone does not remove your sputum, coughing should be added. However, if it clears your sputum, you might not need to cough.
Long episodes of coughing should be avoided since they can be exhausting and cause you to feel out of breath, as well as making your throat or chest painful or tight. Cough only if the sputum can be easily removed; otherwise, return to the beginning of the cycle.
Indications
Post-operative/pain (rib fracture/ICC).
Chronic sputum production, as seen in chronic bronchitis and cystic fibrosis.
Sputum output has increased dramatically.
Inadequate growth.
Retention of Sputum.
SOBAR/SOBOE.
Cystic Fibrosis (CF).
Bronchiectasis.
Atelectasis.
Muscle weakness in the respiratory system.
Ventilation using mechanical means.
Asthma.
Breathing rate/effort has increased.
Airway rattling can be heard.
Secretions are palpable.
Contraindications
Patients are not breathing on their own.
The patient is unconscious.
Patients who are incapable of following directions.
Agitated or perplexed.
Positioning
ACBT can be done while sitting or while in a postural drainage posture. You might begin by sitting until you feel comfortable and confident enough to attempt other ones. Extensive research backs up its usefulness in sitting and gravity-assisted poses. The optimal posture for you to complete the ACBT will, however, be determined by your medical condition and how well it works for you.
Maintain a proper breathing pattern when sitting, with relaxed shoulders, neck, and back supported, since this increases diaphragm function and reduces stress on the musculoskeletal system. Make sure you are comfortable, well-supported, and calm in whichever posture you choose.
The ACBT can be conducted with or without the assistance of a person who provides vibration, percussion, and shaking. The patient may engage in self-percussion/compression.
Individuals prefer the horizontal, side-lying posture, which has been demonstrated to be equally successful as the head-down tipping position.
Duration and Frequency
ACBT should be performed for about 10 minutes, or until your chest feels clear of sputum.
When you’re feeling good, you might just need to perform ACBT once or twice a day. You may need to do it more frequently if you have more sputum. When you’re sick or have a lot of sputum, you may need to undertake shorter or more frequent sessions.
Precaution
Throughout ACBT, it is critical to monitor for dizziness or increasing shortness of breath. If a patient becomes dizzy with deep breathing,
To alleviate dizziness, limit the amount of deep breaths taken during each cycle and return to breathing control.
Inadequate pain control where needed.
Bronchospasm.
Acute, unstable head, neck, or spinal surgery.
Possible side effects
Bronchospasm is associated with hyperreactive airways.
Shortness of breath due to decreased oxygen saturation.
Arrhythmias of the heart.
Atelectasis.
Fatigue.
Summary
When it is easiest for you to move the sputum from your chest, or when you feel sputum has built up in your lungs, practice your exercises. The first indicator might be that you’re getting short of breath or coughing more. It is also vital to attempt to incorporate your breathing exercises into your life and daily routine so that you can practice them on a regular basis. Avoid practicing ACBT immediately after eating. You should talk to your physiotherapist about it.
FAQs
Active Cycle of Breathing Technique – Duration and Frequency
ACBT should be performed for about 10 minutes, or until your chest feels clear of sputum. When you’re feeling good, you might just need to perform ACBT once or twice a day. You may need to do it more frequently if you have more sputum.
Precaution. Throughout ACBT, it is critical to monitor for dizziness or increasing shortness of breath. Reduce the amount of deep breaths done during each cycle and return to breathing control if a patient feels dizzy while deep breathing.
Take 3 to 5 long, calm, deep breaths in, preferably via your nose. Pause for 2-3 seconds at the end of each inhalation, then exhale slowly through your lips, like a sigh. Maintain a comfortable posture with your shoulders and chest. Steps 1 and 2 should be repeated multiple times before proceeding to step 3.
The active cycle of breathing technique (ACBT) comprises three phases of distinct breathing methods that assist in eliminating mucus from the lungs. The first step assists you in relaxing your airways. The second step assists in getting air behind mucus and clearing mucous. The third phase aids in the removal of mucus from your lungs.
ACBT is useful in raising expectorated sputum volume, decreasing secretion viscoelasticity, and alleviating symptoms such as dyspnea.