Chest Physiyotherapy Treatment
Table of Contents
What is Chest Physiotherapy Treatment (CPT)?
Chest physiotherapy is a specialized form of physical therapy that focuses on the respiratory system, specifically the chest and lungs. It involves a range of techniques aimed at improving lung function, clearing mucus and secretions from the airways, and enhancing overall respiratory health. This therapy is commonly used to manage various respiratory conditions such as cystic fibrosis, chronic obstructive pulmonary disease (COPD), pneumonia, bronchiectasis, and other conditions that affect breathing and lung function.
Mucus is produced by the lungs to aid in germ defense. Cystic fibrosis causes mucus to thicken and become difficult to remove. This is pus.
Infections are possible. Infections induce lung inflammation or edema. Infections and inflammation both increase mucus production. More Mucus in the lungs might cause further infections. This cycle of infection, inflammation, and increased mucus can be harmful to the lungs and reduce lung function.
How to Do It?
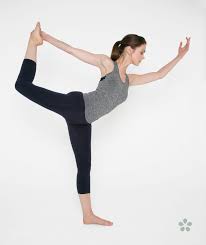
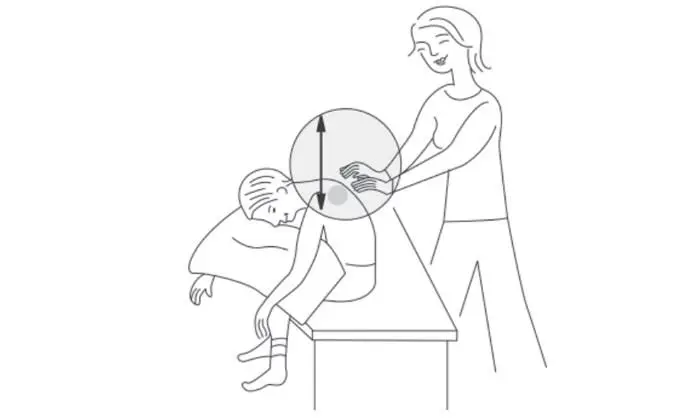
Postural drainage involves lying or sitting in various postures such that the area of the lung to be drained is as high as feasible. Percussion, vibration, and gravity are then used to empty that portion of the lung. These positions may be adjusted to your child’s requirements by your care team.
The carer can clap on the individual’s chest wall while the person with CF is in one of the positions. Typically, this is done for three to five minutes, followed by 15 seconds of vibration over the same area (or during five exhalations). The individual is then advised to cough or puff vigorously to clear the mucus from the lungs.
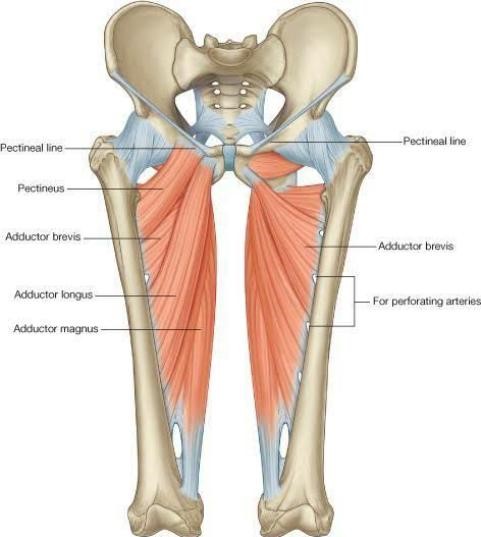
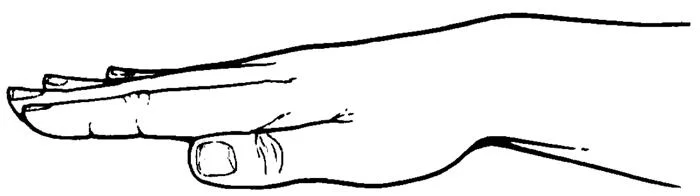
Clapping (percussion) on the chest wall over the region of the lung to be drained aids in the movement of mucus into the bigger airways. As illustrated in the illustration below, the hand is cupped as if to hold water, but with the palm facing down. The cupped hand bends to the chest wall, trapping an air cushion to ease the clapping.
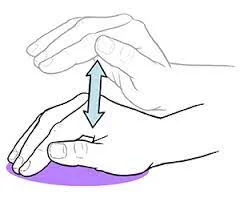
This image is a cupped hand illustration.
Percussion is performed firmly and consistently. Each rhythm should sound hollow. Because the majority of the action occurs in the wrist and the arm is relaxed, percussion is less exhausting to perform. Percussion should not be uncomfortable or sting if the hand is appropriately cupped.
It is very important not to clap over the:
Spine
Breastbone
Stomach
Different percussion devices may be used instead of the standard cupped hand method to avoid injury to the spleen on the left, liver on the right, and kidneys in the lower back. Request a recommendation from your CF doctor or respiratory therapist for one that will work best for you.
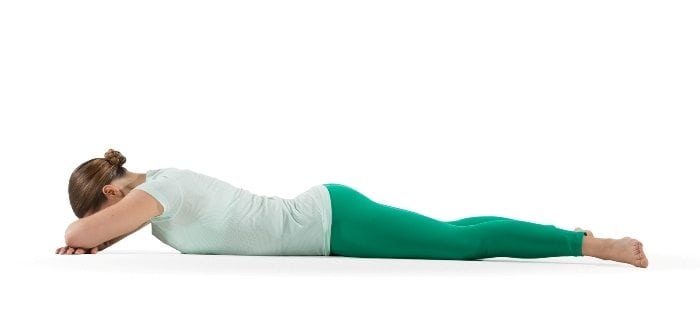
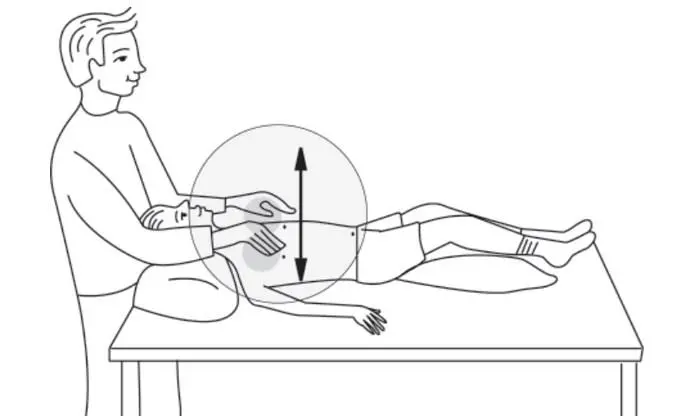
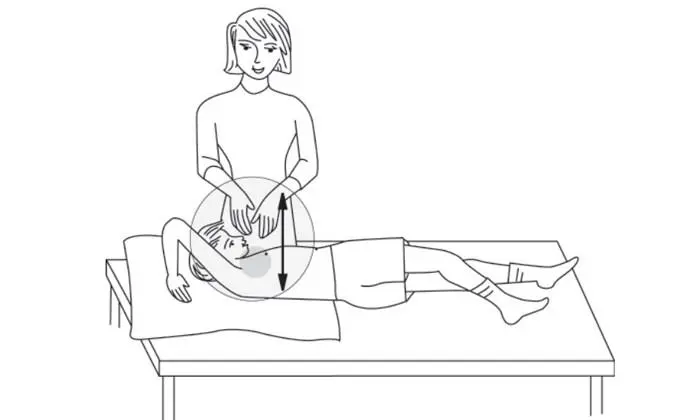
Vibration is a method that gently vibrates the mucus to allow it to enter the bigger airways. The carer lays a firm palm on the chest wall over the drained lung and tenses the arm and shoulder muscles to generate a precise shaking motion. The carer then applies gentle pressure to the vibrated region. (The carer can also place one hand over the other and vibrate by pressing the top and bottom hands against each other.)
Vibration is performed with the flattened hand rather than the cupped hand (see illustration below). Exhalation should be as thorough and gradual as feasible.
This image is a flat-hand illustration.
Deep breathing helps to move the loosened mucus and may cause coughing. Breathing through the diaphragm (belly breathing or lower chest breathing) allows a person to take deeper breaths and get air into the lower lungs. When a person breathes in, the belly expands, and when he or she breathes out, the belly contracts. You may learn more about this sort of breathing from your CF respiratory or physical therapist.
Aims
Increased mucus in the respiratory tract.
The following are the goals of chest physiotherapy:
- To aid in the elimination of trapped or excessive airway secretions.
- To increase gas exchange and optimize lung compliance and the ventilation-perfusion ratio.
- To reduce the amount of labor required for breathing.
- Increase your tolerance to exercise.
- Prevent further difficulties.
How Does Chest Physiotherapy Work?
Now that we know how and why airway obstruction occurs, let’s look at how airway-clearing therapies, such as CPT, might help individuals find symptom relief.
As previously stated, CPT refers to a collection of strategies used in tandem to assist in reducing mucus development. It is crucial to note, however, that this sort of therapy can be delivered in one of two ways:
- 1] Manual Chest Physiotherapy (Manual CPT)
- 2] Percussion Vest Therapy
How Does Manual CPT Work?
Manual CPT is often conducted at the patient’s own home. A carer, family member, or respiratory therapist will physically clap on a person’s chest wall while sleeping in various positions: “Clapping (percussion) by the caretaker on the chest wall above the emptied lung helps drive the mucus into the bigger airways.”
The person administering CPT will clap the chest repeatedly, utilizing a steady, even beat, while cupping the hand to assist in easing the clapping movement. Following a sequence of percussion, the carer will use a steady hand to generate a shaking motion to assist in the formation of vibrations in the lungs.
As previously stated, this approach is frequently followed by postural drainage. The patient will be told to sit or lie down in different positions so that gravity can draw the mucus toward the mouth.
How Frequently Is Manual CPT Performed?
Because each person is unique, the frequency and length of CPT will vary. Percussion treatment, on the other hand, might take up to 20-40 minutes to complete from start to finish.
The percussion (clapping) takes roughly 3-5 minutes for each portion of the lung that is being drained. The carer will next flatten his or her palm on the patient’s chest wall over the area being drained after the clapping movement. The carer will then apply gentle pressure and shake the body to induce vibration. This might last about 15 seconds.
Following that, the patient is instructed to cough vigorously to clear the mucus from the lungs.
Each posture is constructed with a large portion of the lung looking downward. When paired with percussion, it is also referred to as postural drainage and percussion (PD&P). A carer or spouse can slap or vibrate the person’s chest at this point to further dislodge and transfer the mucus to the bigger airways, where it can be coughed or puffed out of the body.
How Is Percussion Vest Therapy Performed?
Patients who get high-frequency chest wall oscillation (HFCWO) therapy wear an inflated vest that produces repeating pulses of air that compress and release their upper body, freeing and thinning mucus from the lungs so it may be coughed up more readily.
Though we cannot speak for any percussion vest on the market, the SmartVest Airway Clearance System operates as follows:
Patients will put on their HFCWO treatment garment, which has Velcro-like fasteners and fits comfortably over the shoulders and chest wall. The vest is equipped with a single hose connector that connects to the generator.
During therapy, the garment gently squeezes and releases the chest wall, causing fast air circulation throughout the lungs and shearing mucus away from the lining of the airways, causing it to thin. The oscillation encourages mucus to be driven upward, where it may be coughed up more readily.
Coughing, or “huff cough,” is used in conjunction with HFCWO treatment, since it helps patients bring up loosened phlegm.
A puff cough is comparable to how you would clean your glasses by breathing on them. The patient will begin by deeply breathing through his or her nose. The patient will then press the air out via the mouth in three equal breaths while tugging in the belly area, generating a “huff” sound in the back of the throat. This breathing method, while effective, requires practice and should be practiced 2-3 times.
How Long Does CPT Take?
Each therapy session might take anywhere from 20 to 40 minutes. To reduce the risk of vomiting, CPT should be performed before meals or one and a half to two hours after eating. It is normally advised to get up early and go to bed early. If the person is becoming more congested or unwell, the length and frequency of CPT may need to be increased.
Classification
Chest physiotherapy includes a variety of physiotherapy therapies. Based on changing research, chest physiotherapy approaches can be classed as traditional, contemporary, or instrumental.
Conventional Techniques
Traditional chest physiotherapy is another name for conventional chest physiotherapy. It was initially proposed in 1915. Manual handling techniques are used to enhance mucociliary clearance. Chest Physiotherapy was originally called Postural Drainage with Percussion and Vibration (PDPV). Coughing exercises and forced expiratory procedures (huffing) were later added to it. PDPV with puffing produced an effective result. It can be done alone or with the help of another person (a physiotherapist, parent, or carer). PDPV is more effective when combined with bronchodilator medication.
Postural drainage
Postural drainage is the practice of placing a person with the use of gravity to enhance the regular airway clearance process. Postural drainage placement changes depending on whether parts of the lungs have a lot of secretions. The target lung segment(s) are placed superior to the carina in each position. Positions should be kept for 3 to 15 minutes (longer in extreme circumstances).
Standard postures are changed as needed based on the patient’s condition and tolerance. It is critical to auscultate the lungs and determine the postural drainage position before establishing the postural drainage position.
Percussion
Percussion is sometimes referred to as upping, clapping, and tapotement. Percussion’s objective is to transmit kinetic energy to the chest wall and lungs regularly. This is accomplished by rhythmically hammering the thorax with a cupped hand or mechanical device directly over the lung segment(s) to be evacuated.
Vibration
The application of a slight tremorous motion throughout the drainage area (manually done by pushing in the direction that the ribs and soft tissue of the chest move during expiration) is termed as vibration.To loosen and remove airway secretions, a fast vibratory impulse is conveyed through the chest wall from the therapist’s flattened hands via isometric alternating contraction of the forearm flexor and extensor muscles.
Coughing
Coughing encompasses both directed and aided coughing techniques.
Forced Expiratory Technique (FET)
Forced expiratory procedures include diaphragmatic inspiration, relaxation of the scapulohumeral region, and forceful expiration from mid to low lung volumes while keeping the glottis open (“huffing” exercises)It works better than coughing.
Indication of Conventional techniques
- Postural drainage positioning.
- The patient’s inability or reluctance to shift bodily position. Mechanical ventilation, neuromuscular illness, and drug-induced paralysis are among the examples.
- Poor oxygenation due to location (e.g., unilateral lung disease).
- Potential for or presence of atelectasis.
- Presence of artificial airway
PDPV
- Difficulties clearing secretions when expectorated sputum output exceeds 25-30 mL/day (adult).
- In the presence of an artificial airway, there is evidence or suspicion of retained secretions.
- Atelectasis is caused by or thought to be caused by mucus blocking.
- Cystic fibrosis, bronchiectasis, and cavitating lung disease are all diagnosed.
- The patient has excessive sputum or central consolidation.
- Frequency
Patients who are ventilated or severely unwell should be positioned as needed around the clock, with the aim of once per hour or every other hour as tolerated. Less acute individuals should be rotated every 2 hours if tolerated.
PDPV
PDT should be conducted every 4 to 6 hours in critical care patients, including those on mechanical ventilation. Individual treatment assessments should be used to re-evaluate PDT guidelines at least every 48 hours.
Frequency should be decided in spontaneously breathing patients by examining patient response to therapy.
Acute care patient orders should be re-evaluated at least every 72 hours or whenever there is a change in patient status based on patient response to therapy.
Domiciliary patients should be re-evaluated every 3 months and whenever their status changes.
Modern techniques
Several other noninvasive clearing procedures have been developed throughout the years to supplement this basic method. To mobilize secretions, modern treatments employ a version of flow through breath control. It comprises a vigorous breathing cycle as well as autogenic drainage.
Active cycle of breathing technique
Active cycle of breathing technique (ACBT) is a patient-performed active breathing method that may be used to mobilize and eliminate excess pulmonary secretions as well as enhance overall lung function. It is divided into three major stages: Controlled breathing, thoracic expansion, and forced expiratory technique
Autogenic drainage
Patients with respiratory disorders (e.g., cystic fibrosis, bronchiectasis) employ autogenic drainage, a diaphragmatic breathing pattern, to rid the lungs of mucus and other secretions.
Instrumental techniques
Noninvasive ventilation, for example, has been regarded as effective as an adjuvant treatment for airway clearing and respiratory support. The following are examples of common instrumental techniques:
Positive expiratory pressure (PEP):
Positive expiratory pressure devices, such as a mouthpiece or facemask, give resistance to expiration, followed by forced expirations. Inhalation is tidal volume, and expiration is slightly active against devices. These devices help in secretion removal by increasing functional residual capacity, which enhances collateral ventilation and secretion removal from collapsed airways. Flutter, Acapella, lung flute, and other devices are included.
Continuous Positive Airway Pressure:
Positive end-expiratory pressure (PEEP) is produced by exhalation against constant opening pressure. Commercially available pressure drivers can also provide continuous positive airway pressure. These are frequently accompanied by the use of nasal prongs or a CPAP face mask. Bubble CPAP is appropriate for use in low-resource settings and with youngsters. A nasal cannula interface, inspiratory and expiratory tubing, and an underwater bottle system are all part of it.
High-Frequency Chest Wall Oscillation (HFCWO):
External chest wall oscillations are administered to the chest using an inflatable garment that wraps around the chest as an airway-clearing procedure. These devices generate vibrations with varying frequencies and intensities, which aid in the loosening and separation of thin mucus from the airway walls.
HFCWO is made up of an inflated jacket coupled to a pulse generator through hoses, allowing it to function at various frequencies (5-25 Hz). The generator pumps air via the hose, causing the vest to rapidly inflate and deflate. HFCWO is made up of an inflated jacket coupled to a pulse generator through hoses, allowing it to function at various frequencies (5-25 Hz). During the 20- to 30-minute HFCWO therapy, it is often stopped every 5 minutes to cough out loosened mucus.
Intrapulmonary Percussive Ventilation (IPV):
developed to enhance bronchial secretion mobilization and increase breathing efficiency and distribution by providing intrathoracic percussion and vibration as well as an alternate technique for delivering positive pressure to the lungs. Each IPV session lasted fifteen minutes and was carried out twice a day (in the morning and afternoon). A nasal cannula interface, inspiratory and expiratory tubing, and an underwater bottle system are all part of it. A thumb button is used to alter the duration of each percussive cycle. The airway maintains constant PAP throughout the cycle. It also has a nebulizer for delivering the aerosol.
Contraindications of Conventional Techniques
- Positioning
All positions are contraindicated for:
Intracranial pressure (ICP) > 20 mm Hg
Head and neck injury until stabilized (Absolute)
Active hemorrhage with hemodynamic instability (Absolute)
Recent spinal surgery (for example, a laminectomy) or a recent spinal injury
Acute spinal injury or active hemoptysis
Empyema
Bronchopleural fistula
Pulmonary edema associated with congestive heart failure
Large pleural effusions
Pulmonary embolism
Patients who are elderly, disoriented, or nervous and cannot endure position changes
Rib fracture, with or without flail chest
Surgical wound or healing tissue
- Trendelenburg position is contraindicated for
Intracranial pressure (ICP) > 20 mm Hg
Patients who must avoid elevated intracranial pressure (e.g., neurosurgery, aneurysms, eye surgery)
Uncontrolled hypertension
Distended abdomen
Oesophageal surgery
Recent gross hemoptysis caused by a recent lung cancer that was treated surgically or with radiation treatment.
Uncontrolled airway susceptible to aspiration (tube feeding or recent meal)
In the presence of hypotension or vasoactive drugs, reverse Trendelenburg is contraindicated.
Complications
Hypoxemia
Bronchospasm
Increased Intracranial Pressure
Acute Hypotension During Procedure
Pulmonary Hemorrhage
Muscle, rib, or spine pain or injury
Vomiting and Aspiration
Bronchospasm
Dysrhythmias
Instructions for CPT
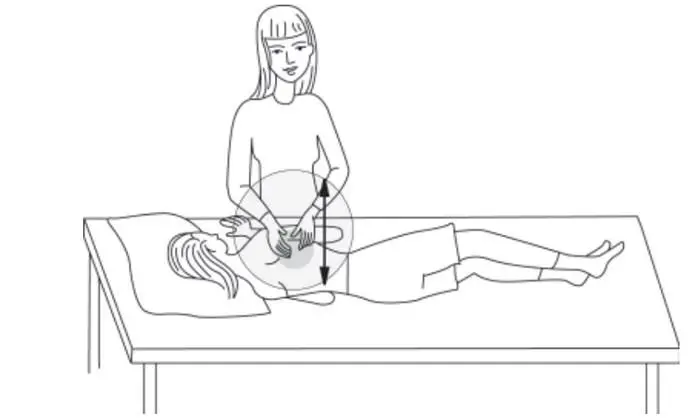
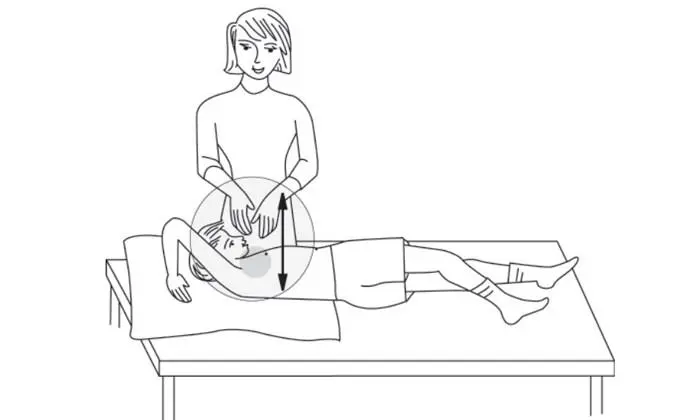
The positions for CPT are depicted in the diagrams below. Shaded regions in the illustrations indicate where the chest should be clapped or vibrated. As a refresher:
Pillows can be used to give extra comfort. The sequence of the positions can be changed if the person tires easily, but all parts of the chest should be percussed or clapped.
Please keep in mind to just clap and vibrate over the ribcage.
To avoid injuries to the spleen on the left, liver on the right, and kidneys in the lower back, avoid clapping and vibrating across the spine, breastbone, stomach, and lower ribs or back. On bare skin, do not clap or vibrate.
image)

Self-Percussion — Upper Lobes
Your child should sit up straight and clap over the muscle area between the collarbone and the top of the shoulder blade on the front of the chest. Repeat on the other side. If your child is able, he or she can also clap his or her own upper back.

This diagram depicts how to do chest percussion on a child’s upper front chest – upper lobes.
Upper Front Chest — Upper Lobes
Have your child sit upright. Clap across the muscle area between your collarbone and the top of your shoulder blade on both sides of your upper front chest.
This illustration shows how to do chest percussion on a child’s upper back chest – upper lobes.
Upper Back Chest — Upper Lobes
Allow your youngster to sit up and lean forward at a 30-degree angle on a cushion over the back of a sofa or soft chair. Clap both sides of your child’s upper back while standing or sitting behind them. Avoid clapping on your child’s backbone.
This diagram depicts how to do chest percussion on a child’s upper front chest – upper lobes.
Upper Front Chest — Upper Lobes
Place your child on his or her back, arms at his or her sides. Place your hand behind your child’s head. Clap your child’s chest between the collarbone and the nipple.

This diagram depicts how to do chest percussion on a child’s left side front chest.
Left Side Front Chest
Allow your youngster to lie on his or her left side with his or her left arm up overhead. Clap over the lower ribs on the front side of the left chest, right below the nipple region. You should not clap on your child’s stomach.
This diagram depicts how to do chest percussion on a child’s right side front chest.
Right Side Front Chest
Allow your youngster to lie on his or her right side with his or her right arm up overhead. Clap over the lower chest on the front side of the right chest, just below the nipple region. Avoid clapping your child’s lower ribs.
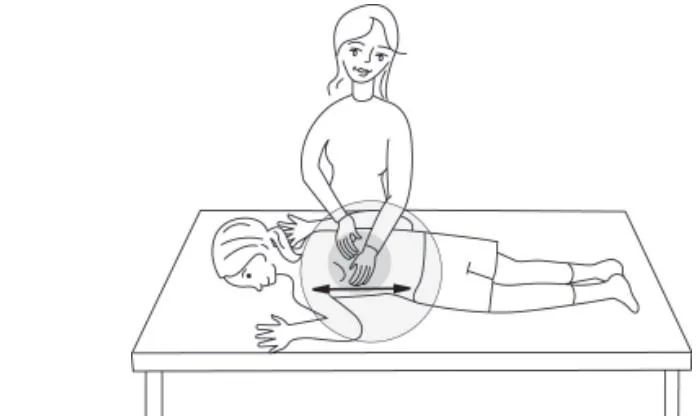
This diagram depicts how to do chest percussion on a child’s lower back chest – lower lobes.
Lower Back Chest — Lower Lobes
Allow your youngster to lie down on his or her stomach. Clap both sides at the bottom of his or her chest, right above the ribs. Clap over the backbone and not the lower ribs.
This diagram explains how to do chest percussion on a child’s left lower side rear chest – lower lobes.
Back Chest — Lower Lobe — Left Lower Side
Allow your child to lie on their left side and roll towards you a quarter turn so you can reach their back. Clap on the lower left side of his or her chest, right over the ribcage’s bottom line.
This diagram shows how to do chest percussion on a child’s right lower side back – lower lobes.
Right Lower Side Back — Lower Lobe
Allow your child to lie on their left side and roll towards you a quarter turn so you can reach their back. Clap on the lower right side of his or her chest, just over the ribs.
Children were shown without shirts to better illustrate the PD&P approach.
Lower Back Chest — Lower Lobes
Allow your youngster to lie down on his or her stomach. Clap both sides at the bottom of his or her chest, right above the ribs. Clap over the backbone and not the lower ribs.
This diagram shows how to do chest percussion on a child’s right lower side back – lower lobes.
Right Lower Side Back — Lower Lobe
Allow your child to lie on their left side and roll a quarter turn towards you so that you can reach their back. Clap on his or her bottom right side of the chest, just over the ribcage.
Children were shown without shirts to better illustrate the PD&P approach. The photographs are from the CF Family Education Programme.
Making CPT More Enjoyable
Consider one of the following to make CPT more enjoyable:
Schedule CPT is almost a favorite TV show.
Play famous songs or recorded stories.
Spend time before, during, and after CPT playing, conversing, or singing.
Encourage blowing or coughing activities for children during CPT, such as blowing pinwheels or coughing the deepest cough. Ask helpful and capable relatives, buddies, brothers, and sisters to do CPT.
This might be a nice diversion from the daily grind.
Minimize interruptions. Finding ways that make CPT more enjoyable can help you keep a routine and get maximum health benefits.
Doing CPT Comfortably and Carefully
During CPT, both the individual with CF and the carer should be at ease. Before beginning, the individual should remove any restrictive clothes, jewelry, buttons, or zippers around the neck, chest, and waist. Wear light, soft clothes, such as a T-shirt. CPT should never be done on exposed skin. The caretaker should remove rings and other bulky jewelry, such as watches or bracelets. Keep tissues or a place to cough up mucus nearby.
To preserve his or her back, the caretaker should not lean forward when doing drums. The surface on which the person with CF lies should be at a comfortable height for the caretaker.
When employing CPT, many families find that using pillows, couch cushions, or bundles of newspapers beneath pillows, as well as cribs with adjustable mattress heights/tilts, foam wedges, or bean bag chairs, is effective. With or without cushions, infants can be put in the caregiver’s lap.
Summary
Patients with a range of medical respiratory diseases should be administered physiotherapy with the goal of managing dyspnea and symptom control, improving or maintaining mobility and function, and improving or supporting airway clearing and coughing. Rehabilitation, exercise testing (including ambulatory oxygen assessment), exercise prescription, airway clearance, and posture and breathing methods are among the strategies and techniques used.
Physiotherapy may be beneficial in the treatment of postural and/or muscular dysfunction and discomfort, as well as in the improvement of continence, particularly during coughing and forceful expiratory movements. Physiotherapists are often crucial to the administration of pulmonary rehabilitation and may be helpful in the provision of non-invasive ventilation. Physiotherapists are commonly engaged in the supply of oxygen and some nebulized medications, as well as crucial monitoring of things like ventilatory function and heart rate.
FAQs
Chest physical therapy is typically used in combination with other therapies to clear secretions from the airways and avoid lung infections.
Performing CPT
Percussion is applied to various locations of the chest wall to assist in loosening and transporting mucus toward the center of the chest. Percussion is practiced for two minutes in each position. If the youngster is old enough, two to three huff coughs are performed between each posture.
How to Go About It. Postural drainage involves lying or sitting in various postures such that the area of the lung to be drained is as high as feasible. Percussion, vibration, and gravity are then used to empty that portion of the lung. These positions may be tailored to your or your child’s requirements by your care team.
You should have your chest lower than your hips, which you may do by laying on a sloped surface or raising your hips 18 to 20 inches with cushions or another item. This is the ideal position for emptying the bottom and front portions of your lungs.
The following are all relevant contraindications to chest physiotherapy: Bleeding diathesis (including anticoagulant therapy) Physical discomfort caused by physical postures or manipulations. Intracranial pressure is elevated.