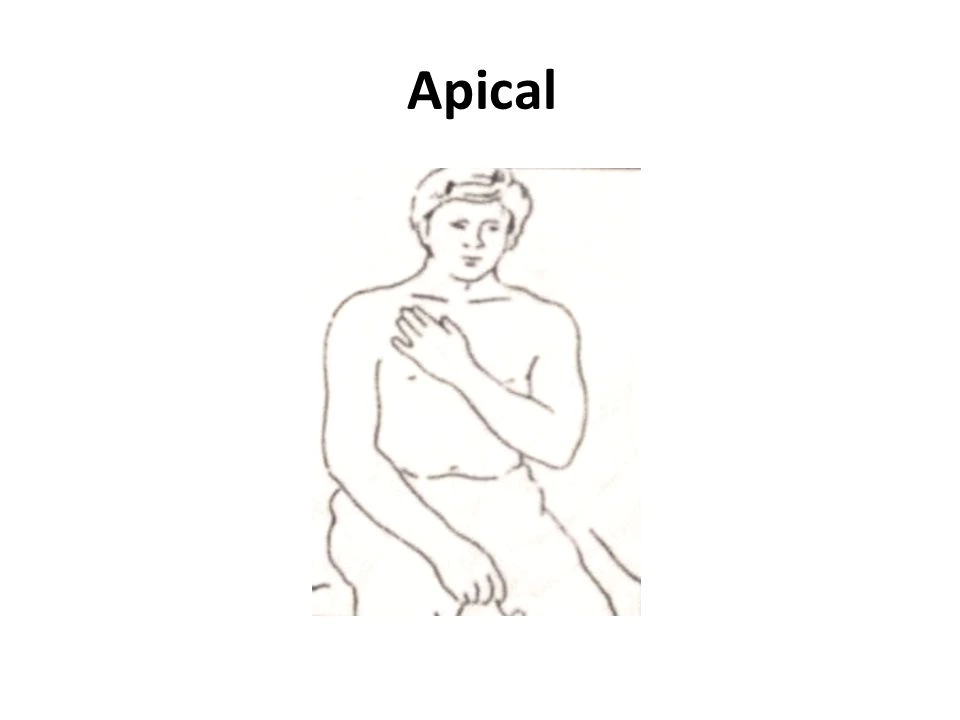
Apical Breathing Exercise
Table of Contents
What is an Apical Breathing Exercise?
Apical breathing exercise is a practice of breathing that includes most movement to the upper chest.
Apical expansion
The therapist’s hand in bed should be below the collarbone if the patient is seated in a chair.
Apply pressure with the palm or fingertip just below the collarbone while the patient exhales; this procedure is used in patients who have had surgery and have a pneumothorax.
Indication
cystic fibrosis
bronchiectasis
lung abscess
chronic obstructive pulmonary dialed
neuromuscular diseases
atelectasis
acute or chronic lung disease
airway obstruction
pneumonia
any condition involving the lungs
postoperative pain
shortness of breath
cough and sputum in the lungs
Contraindications
pain and discomfort due to injury increased intracranial pressure
head and neck injury
hypertension
Any type of fracture around the chest
If the patient has an abdominal incision
recent breast surgery
airway obstruction
weakness of the diaphragm and intercostal muscles
Symptoms of Breathlessness
Apical breathing frequently causes people to be out of breath when engaging in strenuous exercise. It can also cause headaches, upper back stress, neck discomfort, shoulder pain, and numbness.
- Why is that an issue?
Apical breathing requires the use of fewer muscles than diaphragmatic breathing. While some may argue that less is more, this is not the case. An example Breathing Breathless breathing frequently requires the use of additional muscles in the neck and shoulders, whereas diaphragmatic breathing involves the use of the diaphragm as well as muscles in the neck, chest, and between the ribs to help you take a deep, even breath.
This shows that the shoulder and neck muscles of the apical breather are working hard without the advantage of a deep breath.
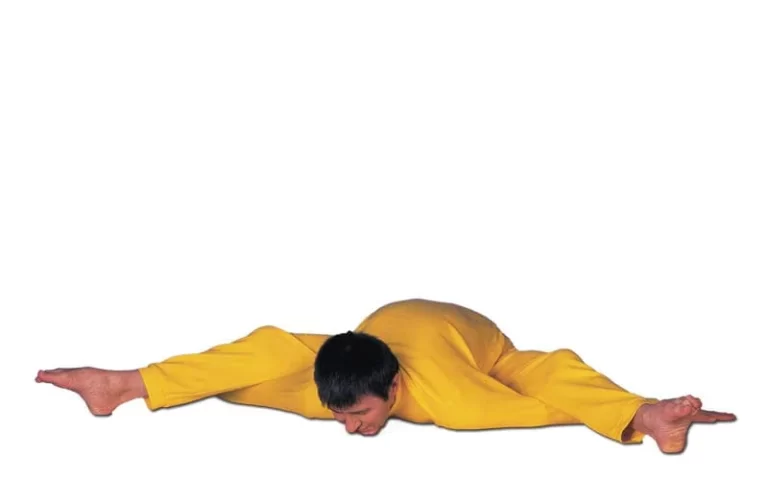
Classification of Breathing Pattern Disorders
There are other classifications of BPDs,(Breathing Pattern Disorders) but six core dysfunctions identified in the literature have established the cornerstone of the BPD evaluation. Diaphragmatic or belly breathing is a natural breathing style.6 Although this is a normal breathing pattern, it should be emphasized that a “normal” breathing pattern seen in patients is not the optimal functioning breathing pattern. There are a few dysfunctional variants of an abdominal breath, such as asymmetrical with restricted action on one side of the belly; anterior movement only, with no lateral or posterior movement; and adequate anterior and lateral movement, but no posterior movement.
A chest or apical breather has a considerable movement of the sternum and shoulder girdles towards the skull during inhaling and limited belly movement. Paradoxical breathing occurs when the chest expands during inhalation and the abdomen is dragged inside, and then the abdomen is pushed outwards during expiration. The authors of this commentary suggest a new BPD categorization that is connected with a startle reaction. A startle reflex occurs when a patient’s right or left 1st and 2nd ribs, anterior 7th and 8th ribs, and 11th and 12th ribs initiate a withdrawal response when palpated. this series will offer three patient stories demonstrating the short-term impact of treating a startle reflex BPD.
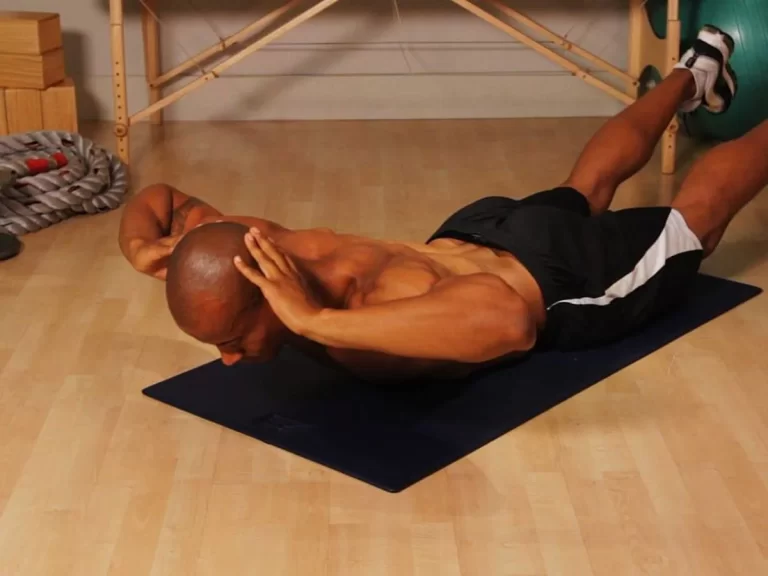
Assessment of Breathing Patterns
When a patient visits the clinic, his or her breathing pattern is evaluated. The patient is unaware that they are being studied during this period, which decreases the potential of conscious alterations in breathing patterns. The patient’s posture should also be evaluated since a slumped or stooped posture might impede the diaphragm’s capacity to fully expand. The doctor can begin a detailed breathing examination after the initial observational breathing pattern evaluation and full patient history.
Breathing is often examined in a comfortable, supine posture. Still, it can also be monitored in more difficult situations such as sitting, standing, or positions that cause pain or suffering. During the Hi-Lo test, the patient is instructed to lay one palm on their chest and the other on their belly. The patient is not given any more instructions once in this posture, however, the doctor may ask him or her questions about their history. Unless the patient has received previous instruction in abdominal breathing, the patient should breathe normally and not be cued to take a deep breath during the examination, as a prompted breath will often result in chest movement.
Clinical Advantage
Breathing is an automatic function that is considered to be essential for posture and core stability. Restoring normal respiratory mechanics and motor control can lead to less discomfort, better patient outcomes, and overall better patient health.6,8 Breathing pattern analysis is a simple clinical procedure to master. In the rehabilitation clinic, treating BPD takes little to no equipment, and intervention approaches supplied by the physician can be arranged as a home exercise program in five minutes or less.
Summary
BPD examination and categorization are critical because normal and abnormal breathing patterns impact mobility. Finding suitable exercises for muscular relaxation, re-education of motor control patterns, and normal breathing patterns at rest and during activities may assist restore normal and physiologically balanced breathing if a respiratory disorder is identified.6 Breathing pattern examinations and treatments may enhance patient quality of life, physical function, and reduced breathing signs and symptoms during everyday activities and exercise.
FAQs
Thoracic dominant breathing or apical breathing occurs when there is the predominant use of the upper thorax with a lack of lateral costal expansion. Thoracic dominant breathers with high Nijmegen questionnaire scores had higher levels of dyspnea.
Apical Breathing Explained: Headaches, Neck Pain…
What options are there? Lots! A massage therapist can assist relieve stress in the overused neck and shoulder muscles, reducing the frequency of headaches and numbness. Your massage therapist can also assist you in developing new breathing patterns that will allow you to breathe from the diaphragm.
Contraindications
Patients are not breathing on their own.
The patient is unconscious.
Patients that are incapable of following directions.
Agitated or perplexed.
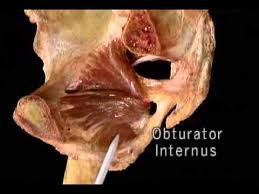
Apical hypertrophic cardiomyopathy (AHCM) is a rare medical condition that was discovered in 1976. It is a heart disease characterized by negative T-waves on electrocardiography and related to left ventricle apical enlargement.
Apical pulse readings are often taken while seated or lying down. The doctor will place a stethoscope on the apex of the heart on the left side of the breastbone. They can also detect the apical pulse at the peak of the impulse.