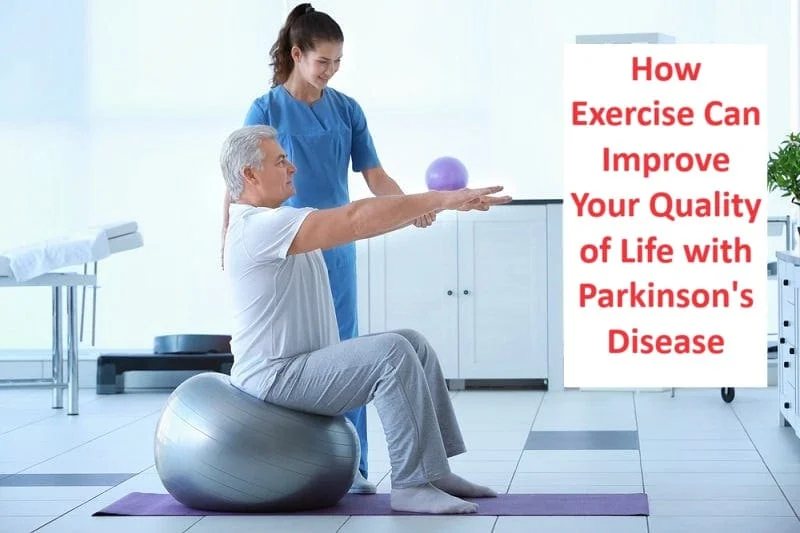
20 Best Exercises for Parkinson’s Disease
Exercises for Parkinson’s Disease play a crucial role in improving mobility, strength, and flexibility. Along with Medical Treatment, Exercise is also an important part of the overall treatment program for Parkinson’s Disease.
Table of Contents
Introduction
Parkinson’s disease (PD), or simply Parkinson’s disease, is a chronic degenerative disease of the central nervous system that affects both the motor and non-motor systems. Symptoms usually appear slowly, and non-motor symptoms become more common as the disease progresses.
Early symptoms include tremors, stiffness, slowness of movement, and difficulty walking. Problems with thinking, behavior, sleep, and sensory systems can also occur. Parkinson’s disease dementia is common and progressive.
The motor symptoms of the disease are caused by the death of neurons in the substantia nigra, an area of the midbrain that supplies dopamine to the basal ganglia. The reason for this cell death is poorly understood, but it involves the aggregation of alpha-synuclein protein into Lewy bodies in neurons.
The primary motor symptoms are collectively known as parkinsonism. Predisposing factors are a combination of genetic and environmental factors. Those who have an affected family member have a higher risk of developing the disease because certain genes are inherited risk factors.
Environmental risks include exposure to pesticides and previous head injuries; exposure to trichloroethylene is also suspected. The diagnosis of Parkinson’s disease is based mainly on symptoms that are usually related to movement. PD usually occurs in people over the age of 60, with about one percent affected.
In people under 50, this is called early-onset PD. The average life expectancy after diagnosis is 7 to 15 years. There is no known cure for PD, and treatment is aimed at relieving symptoms. Initial therapy usually includes L-DOPA, MAO-B inhibitors, or dopamine agonists.
As the disease progresses, these drugs weaken and cause a side effect characterized by involuntary muscle movements. Diet and certain forms of rehabilitation have been shown to be effective in relieving symptoms.
Surgery to implant microelectrodes for deep brain stimulation has been used to reduce severe motor symptoms when medications are ineffective. Evidence for the treatment of non-movement-related symptoms of PD, such as sleep disturbances and emotional problems is less strong.
Symptoms of Parkinson’s disease
The four primary symptoms of PD are:
- Tremor – Tremor (tremor) often starts in the hand, although sometimes it affects the leg or jaw first. The tremor associated with PD is characterized by a rhythmic, back-and-forth movement that can involve the thumb and index finger and feel “pill-like.” This is most obvious when your hand is in the resting position(resting tremor). This tremor usually disappears during sleep or improves with purposeful and purposeful movement.
- Rigidity – Rigidity (muscle stiffness) or resistance to movement affects most PD patients. The muscles are constantly stretched and contracted so that the person hurts or feels stiff. The rigidity becomes obvious when another person tries to move the individual and arm, which will move only in short, jerky movements known as “cogwheel” rigidity.
- Bradykinesia—This is a slowness of movement and automatic movement that can be particularly frustrating because it may convert a simple task into a difficult task. some easy activities take more time because of the bradykinesia. lack of facial expression. mostly seen the moon-like face of the patient.
- Postural instability—due to postural instability there is the risk of falls while walking. The rate of progression and specific symptoms vary from person to person. PD symptoms usually start on one side of the body. However, the disease eventually affects both sides, although symptoms are often less severe on one side than the other. People with PD often develop the so-called Parkinsonian course, which includes a tendency to lean forward, small, quick steps as if rushing (called a party) and reduced swing of one or both arms. They may have difficulty starting movements (initial hesitation) and may stop suddenly (freeze) while walking.
Other problems may accompany PD, such as:
- Depression – Some people lose motivation and become dependent on family members. Emotional changes – Some PD patients become fearful and insecure, while others may become irritable or unusually pessimistic.
- Difficulty swallowing and chewing – In the later stages of the disease, swallowing and chewing problems may occur. Food and saliva can build up in the mouth and back of the throat, causing choking or drooling. Getting enough nutrition can be difficult.
- Speech changes – About half of PD patients have speech difficulties, which can be characterized as speaking too softly or in a monotone. Some may hesitate to speak, be shy, or speak too quickly.
- Urinary tract problems or constipation – Bladder and bowel problems can occur due to dysfunction of the autonomic nervous system, which is responsible for regulating smooth muscle activity.
- Skin problems – The skin on the face can become oily, especially on the forehead and sides of the nose. The scalp can also become oily, causing dandruff. In other cases, sometimes skin becomes dry.
- Sleep problems – Common sleep disturbances in PD include difficulty falling asleep at night, restless sleep, nightmares and emotional dreams, and falling asleep or falling asleep suddenly during the day. Another common problem is “REM behavior disorder,” in which people have dreams that may cause harm to themselves or their bed partners. Medications used to treat PD can affect some sleep disorders. Many of these problems respond to certain treatments.
- Dementia or other cognitive problems – Some people with PD develop a lack of memory problems and their thought processes become slow. Cognitive problems become more severe in the late stages of PD and some people are diagnosed with Parkinson’s disease dementia (PDD). Memory, social judgment, language, reasoning, or other mental abilities may change.
- Orthostatic hypotension – Orthostatic hypotension is a sudden drop in blood pressure when a person gets up from a lying or sitting position. It may cause dizziness, dizziness, in extreme cases loss of balance or fainting. Studies have shown that in PD, this problem causes a loss of nerve endings in the sympathetic nervous system, which controls heart rate, blood pressure, and other automatic body functions. Medications used to treat PD may also play a role.
- Muscle Cramps and Dystonia – The stiffness and lack of normal movement associated with PD often cause muscle cramps, especially in the legs and toes. PD can also be associated with dystonia – constant muscle contractions that cause a forced or twisted posture. PD dystonia is often caused by fluctuations in the body and levels of dopamine (a chemical in the brain that helps neurons communicate and is involved in movement).
- Pain – Muscles and joints may ache due to stiffness and abnormal posture often associated with the condition. Fatigue and loss of energy – Many people with PD are often tired, especially at the end of the day. Fatigue can be related to depression or sleep disorders, but it can also be caused by muscle stress or overactivity when the person is feeling well. Fatigue can also be caused by akinesia, which is difficulty starting or stopping movement.
- Sexual Dysfunction – Because PD affects nerve signals in the brain, it can cause sexual dysfunction. Depression associated with PD or the use of certain medications can also cause a decrease in sexual desire and other problems. Hallucinations, delusions, and other psychotic symptoms can be caused by medications prescribed to treat PD.
Stages of Parkinson’s disease
Serious effects of Parkinson’s disease can take years or even decades to appear. In 1967, two experts, Margaret Hoehn, and Melvin Yahr, created a staging system for Parkinson’s disease. This staging system is no longer widely used because staging the condition is less useful than identifying how it affects each person’s life individually and then treating them accordingly.
Part 1: Non-motor aspects of everyday life experiences. This section deals with non-motor (non-moving) symptoms such as dementia, depression, anxiety, and other mental capacity and mental health problems. They also ask about pain, constipation, urinary incontinence, fatigue, etc.
Part 2: Motor aspects of everyday life experiences. This section covers the effects on movement tasks and skills. This includes your ability to speak, eat, chew and swallow, dress and wash yourself when you have tremors, and more.
Part 3: Motor examination. healthcare examines the condition with movement of the limb. The criteria measure the effect on your speech, facial expressions, stiffness and rigidity, gait and speed, balance, speed of movement, tremors, etc.
Part 4: Motor complications. In this section, your provider will determine how much your Parkinson’s symptoms are affecting your life. This includes how long you experience certain symptoms each day, and whether these symptoms affect how you spend your time.
Exercise for the Parkinson’s disease
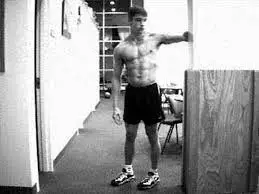
Biceps curl
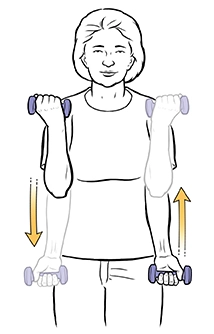
The bicep curl is a very recognizable strength training that works the muscles of the upper arm and, to a lesser extent, the forearm is a great visual exercise leading to strength and definition.
A variety of equipment and handles can be used for this exercise, including dumbbells, Kettlebells, bars, resistance bands, or cable machines. Curls are a typical exercise
upper body strength training routines.
- Start standing with your feet about hip-width apart. Maintain your abs committed Hold one dumbbell in each hand.
- Let the hands relax with the palms at the sides of the body facing forward.
- Keeping the upper arms stable and the shoulders relaxed, bend the elbows and lift the weights as the dumbbells approach your shoulders. Or the full range of motion when lifting dumbbells at eye or forehead level.
- Elbows should stay close to the body. Exhale as you lift.
- Lower the weights to the starting position. Do as many reps as you want, staying within 3-5 reps to complete failure.
Doing bicep curls consistently will help you develop upper arm strength and learn to use your arm muscles properly while supporting yourself with your core muscles. Curls work the biceps the muscles of the front part of the upper arm and the muscles of the arm – brachial and brachioradialis You use these muscles whenever you pick up something normal
all your daily life.
Other Variations of Biceps Curls
- Barbell Curl
- Reveres barbell curl
- hammer curl
Triceps curl

Triceps curls are a push-up exercise that targets the muscles in the back of the arms. tricep curls involve a simple movement pattern where you reach your hands behind your head and then return them to the starting position.
You won’t see the benefits of tricep curls if you’re not using the proper form. First, define your practice position with a dumbbell whose weight corresponds to your fitness level. Then run the next one below to do triceps curls correctly:
- Stand with your feet shoulder-width apart
- Hold a halter overhead with both hands, supporting it.
- Bend both elbows to reduce the weight behind your head.
- Keep your elbows to the sky. Focus on just moving your arms, reaching straight up to the ceiling, and returning to the starting position.
- Repeat as many times as you want.
Triceps curl modifications
One-arm variation: Unilateral exercises (ie on one side) are great to help understand your body’s muscle imbalances.
Seated Triceps Curls: Standing triceps curls add momentum to help movement By sitting, you reduce the temptation to squeeze your legs, which further isolates your work on the triceps.
Incline Triceps Curls: Using an incline bench increases stability and takes time away from the work of its nuclear stabilizers.
Skull Crushers: Although the name suggests that this is a completely different exercise, it is still a triple loop A variation is that you lie down.
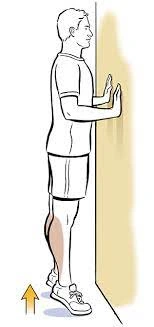
Single leg balance

It is important to stand on one leg. When you walk, you spend about 40% of your time with one leg on the ground while the other leg is in the air. One Leg Pose is a simple but very effective exercise to improve balance. Improving your balance can help improve your athletic performance and prevent falls that can cause serious injuries.
Before you begin balance training, your physical therapist may want to obtain a baseline measurement of your balance to monitor your progress. Balance tests, such as the Functional Range Test or the One Leg Test, can give you an idea of how well your body and balance system are working. To perform the one-leg balance exercises:
- Stand tall with your feet together.
- Keep a stable object around you for safety, such as a chair or kitchen table,(for hold when you feel uncomfortable in between the exercises.
- Lift one leg off the ground. you should take care of the leg do not touch the ground for stability.
- now note the duration of how many times you can hold the leg(keep the clock around you).
- If the duration is 60 seconds or more then you should try the one-leg stand on a soft surface such as a soft pillow.
- hold the chair for support.
- Lift one leg off the ground, slowly.
- You should stand on one leg for five to ten seconds.
- back to the original position and do three to five repetitions.
- Try to increase the duration of holding.
- Do it on the opposite leg.
Heel raise
The heel raise, additionally called heel lifts or eccentric calf increases, is an easy bodyweight workout. Doing it often will make your calves stronger. It also can result in nicer-looking, better-toned calves. Heel increases are an easy and handy manner to hold your calf muscular
tissues in top shape. You can do them nearly anywhere. You can do the heel raise workout as a standalone workout or combine it into your workouts.
The heel increases paintings of the gastrocnemius and soleus muscular tissues inside the calf area. Your frame is based on those muscular tissues on every occasion you stand or walk. A great location to do heel increases is on a flat, non-slippery surface. Use a wall, table, countertop, or the again of a chair for assistance. You can integrate squats with heel increases in a squat with the heel-enhanced workout.
- Start with toes a touch wider than hips. Squat after which raise your legs in order that your heels are off the ground.
- Place your toes flat on the ground. Your toes have to be beneath your shoulders.
- Place one or each arm at the assist to constant yourself.
- Raise each of your heels with a gradual motion in order that you’re status to your toes.
- Maintain the raised role for a minimum of one second.
- Lower your heels slowly again to the ground with a managed motion.
- Repeat eight to fifteen times.
Variations to Heel Raises
Double heel enhanced with weights
Single-leg heel enhances workout
Weighted single-leg heel raise
Tandem walking
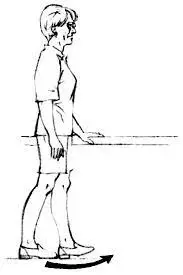
Tandem walking, also known as heel-to-toe, is a balance exercise where you walk in a straight line with the heel of one foot directly in front of the toes of the opposite foot. Tandem walking improves balance, coordination, and proprioception (awareness of body position in space). It strengthens the muscles of the lower body, including the legs, ankles, and core, and can also improve overall stability and posture.
- Stand up straight and make sure there is a clear path behind you. Imagine a straight line on the floor extending away from you, or place a straight line of tape across the floor.
- Walk backward along this line on the floor as if you were walking on a tightrope.
- Place one foot behind the other so that the toes touch the heel.
- Try to keep your balance and keep your feet in the middle of the line.
- Make sure you don’t let your posture drop.
Do this exercise in a hallway or other place where you can walk at least 10 feet without obstruction. It is ideal to use a solid floor, such as a floor without carpet or a low-level carpet.
Side walking
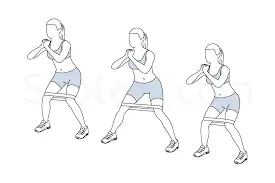
Sidewalks can help improve posture by strengthening the lower body muscles that support the spine and pelvis. Lateral band walks work on the multiple muscle groups of the thigh, including the glutes, and hamstrings, making them powerful and increasing the lower body strength.
- Stand with your feet wide apart and squat into an athletic position.
- Take a step to the right with your right foot until your feet are shoulder-width apart.
- Take a step to the right with your left foot until your feet are hip-width apart.
- Continue with small steps to the right and then repeat on the left side.
Keep your chest up, and back straight and stay down. Take a deep breath as you raise your legs to the sides, keep your glutes tight, and move slowly. The side lunge fully engages your glutes and hip abductors and also strengthens all the major muscles in your hips, thighs, and calves. This Take 10-12 steps to each side or switch sides for 30-60 seconds. For an extra challenge, put a rubber band around each thigh and walk with a side band instead.
Biceps stretching
The biceps stretch has many different variations and can easily be incorporated into your biceps stretching. The following instructions will guide you through the seated biceps stretch:
Sit on the floor exercise mat with your head, neck, and back aligned.
Avoid bending over or around your back during the stretch.
Bend your knees and keep your feet on the floor in front of your hips.
Place your palms on the floor behind you, fingers away from your body.
Adjust your weight evenly between your legs, glutes, and arms.
Exhale without moving your arms and slowly slide your back forward towards your legs until
you feel tension in your biceps (you also feel tension in your shoulders/chest).
Avoid throbbing or tightening pain.
Hold the stretch for about 30 seconds. Return to the starting position
Repeat a certain number of timed stretches.
The biceps stretch targets the biceps (biceps), but can also open the chest and shoulders
muscles This stretch, like all stretches, helps relieve muscle tension and stress by practicing stress or other daily activities.
Modification of the biceps stretching
Alternate Seated Bicep Stretch
Standing Bicep Stretch
Wall Bicep Stretch
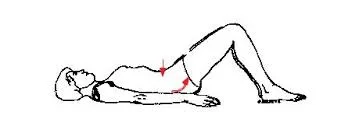
Bridging exercise

Gluteal bridge exercises are a great way to train the posterior chain – the muscles are all down the back of your body. Doing these exercises will isolate and strengthen your glutes(buttocks) muscles – gluteus maximus, medius, and minimus – and hamstrings and quads, pelvis, and core.
- start with a supine lying position on the plinth or mat. Bend your knees and plant your feet firmly mat, making sure they are hip-width apart and your back is in a neutral position. to allow hands on the mat by your sides. This is your starting point.
- Press your heels toward the surface of the plinth and lift your hips off the surface, give contraction through your glutes until your body forms one straight line from chin to knee resting on your shoulders.
- A straight body is key, not pushing your hips as high as possible, which often happens
- to lead to a bent back, pain, or injury. Breathe in.
- lower your hips on the plinth(back to the original position)
Pillow press
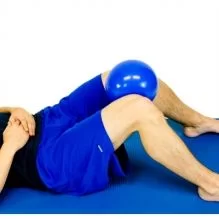
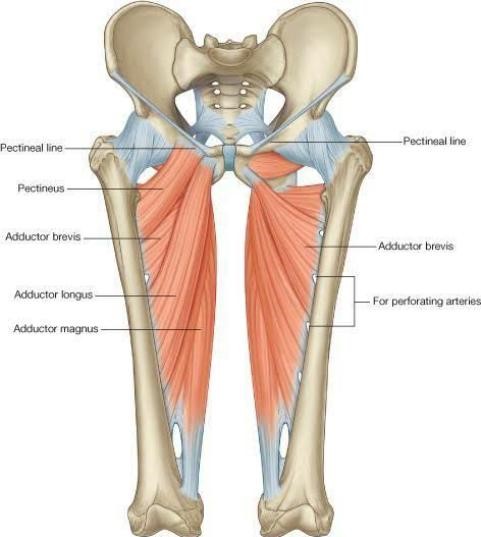
You required a soft cushion for the exercise. This simple exercise can be done anywhere, even in your living room or balcony. It works on the inner thigh muscles, so helps strengthen the knees and prevent knee pain.
The benefit of the pillow press is to strengthen the inner thigh muscles, which helps strengthen the knees and prevent knee pain. Strong inner thighs, also called adductors, help secure the hip joints in their sockets.
- Start with the supine lying position on the plinth or mat. now an extension of the knee joint and hip in flexion. The hand should be placed at the sides of the body, palms up down Relax your neck and shoulders. keep the soft pillow in between the knees.
- You can take support for upper body,so you place a small cushion under your head. This is your starting position. now give pressure on the pillow with the help of the adductor muscle of the hips. Hold for 10 seconds.
- Relax and repeat 10-20 times.
- Never allow your back to arch or allow tension in your neck, shoulders, or back.
- make sure you stabilize the whole body and only move your knees.
Chair squats

Chair squats are a great exercise to increase the strength of the hip muscles(increases the strength of the hip flexors muscles). The chair presents assistance as you figure out your glutes, hamstrings, and quads.
- Stand simply in the front of your chair, going through far from it. Your feet need to be shoulder-width apart, with feet pointing immediately ahead.
- Keep your backbone impartial and your head and chest raised. Engage your center as you bend your knees and decrease your hips down and back. You can elevate your fingers out in the front for added stability at the same time as you decrease yourself down.
- Squeeze glutes and hamstrings to power your hips ahead and up, returning to the beginning position.
- Try doing three units of 10 reps.
Lunges

Lunges are a powerful exercise that allows you to shape and strengthen almost any muscle
lower body Learn how to squat with good form and this lower body workout can become a valuable part of strength training or circuit training.
- Stand in a split stance with your right foot about 2-3 feet in front of your left foot. Your body is straight, shoulders back and down, heart closed and arms relaxed your hips.
- flexion of your hip joint and slight knee flexion so it is slightly toward the floor. at the bottom of the movement, the front thigh is parallel to the ground, the back knee is directed to the floor and your body weight is evenly distributed between both feet.
- keep your whole weight in front of your foot when you back to the starting position.
Other Variations of the Lunges
Assisted Lunge
Half Lunge
Front Foot Elevated Lunge
Dumbbell Lunge
Forward Lunge
Praying position stretches

- While standing, place your palms in a prayer position.
- Let your elbows touch each other.
- Your hands should touch each other from the fingertips to the elbows.
- With your palms together, slowly spread your elbows. Do this by lowering your arms to waist level. Stop when your hands are in front of your belly or you feel tension.
- stop the end range of movement around 10-20 seconds which is necessary.
- Keep your palm on the floor.
- Release your wrists so that your fingers point down.
- With your free hand, gently take the fingers and pull them back towards the body.
- Hold for 10-30 seconds.
Wrist exercise(stretching)

Wrist flexors and wrist extensors can be performed in the wrist stretch. this stretching exercise improves wrist movement and wrist muscle flexibility.
- Wrist Flexor Stretch Stand with your hands on a table, palms up, fingers facing your body, and elbows straight. Lean away from the table. Stay in this position for 15-30 seconds. you can do this stretch three to five times per session.
- Hold a soup can or hit dumbbells in your hand, palm up. Bend your wrists up. Lower the weight slowly and return to the starting position. do 20 repetitions each session and gradually you can increase the repetition of the exercise.
- Wrist Extensor Stretch Stand behind a table with palms down, fingers flat and elbows bent directly Lean your body weight forward. Hold this position for 15 seconds. Repeat 3 times.
- Hold a can of soup or a pound of dumbbells, palm down. Slowly bend your wrist upwards. gradually back to the starting position. Do 3 sets of 10.
Clamshell exercise
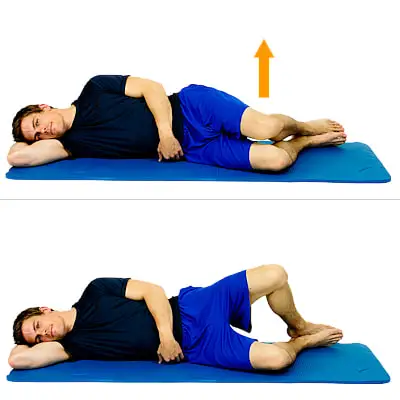
The clamshell exercise focused on the hips and glutes, helping to stabilize and correct the hips and pelvis.
- Lie on your right side, legs, and hips on top of each other, knees bent 90 degrees and
- head rests on your right hand. Put the left hand on your left hip to keep it from tipping back. This is your starting point. Keeping your abs closed and your legs together, lift your left knee as you can without it rotating the pelvis or lifting the right knee off the floor. Hold for 1 second, squeezing the glutes at the top of the movement before slowly lowering to
- the left. keep the knee in the starting position. Continue for a total of 20 repetitions, then repeat on the other side.
- Make it harder: Attach the resistance band around both thighs, just above the knees.
Heel slide

Heel slides are easy leg exercises that involve extending your leg far from your body, bending your knee, and sliding your heel in the direction of your buttocks. You can do heel slides with the use of a bed, floor, or wall.
The motive of heel slides is to increase the strength of the knee muscles. They additionally assist to reinforce and stretch the tissues across the knee and leg muscles. This is a vital part of the healing manner and enables you to save yourself in addition to injuries.
you’ll need to consider some thoughts in mind while doing this exercise:
Slide your heel as near your buttocks as you can. Only bend your knee to an area that is comfortable. You can also additionally experience moderate stress or a sensation in or around your knee, however, it shouldn’t be painful. For every exercise, do 1 to three units of 10 repetitions. Rest for up to at least one minute among units. Do those physical activities as a minimum instance in step with the day.
- You can test together along with your toe placement. Point your toe or draw your feet returned in the direction of your shin. Or flip your feet to both sides.
- Lie in your returned together along with your legs prolonged and your feet barely apart.
- Slide your affected leg as near your buttocks as you can.
- Hold this function for five seconds.
- Slide your heel to return to the beginning function.
Variations of the heel slide
Abduction and adduction heel slides
Seated heel slides
Chair heel slides
Wall heel slides
Shoulder blade squeeze

the rhomboid muscles located on your upper back and below the trapezius muscle play a major role in posture. This is especially true if you have overdeveloped pectoral muscles or your shoulders are hunched forward. The rhomboids are diamond-shaped and used to contract the shoulder blades.
- start with the sitting position on a plinth or chair.
- Shift your body weight slightly forward so you don’t turn your back. keep your whole body relaxed and keep your ears and shoulders aligned.
- Raise your arms to shoulder height, elbows bent and palms facing forward.
- Move your arms back, squeezing your shoulders. Hold for 10 seconds. Return to the starting position.
- Repeat three to five times.
Doorway Pectoralis stretching
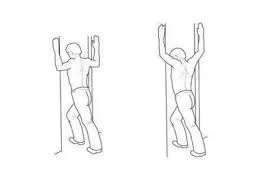
Pectoral stretch is an important exercise to improve the flexibility of your chest muscles mainly the Pectoralis major and Pectoralis minor muscles. this exercise improves posture and provides the relaxation of the pectoralis muscle stretch.
- Take a standing position in the corner of the room and look at the wall.
- Place your palms and forearms against the wall at about shoulder level.
- Place your feet about one foot from the corner.
- Keeping the arms and palms still and the body straight, bend into the corner of the body. Just bend over until you feel a stretch in your chest, but not so much that it causes discomfort or pain.
- Hold for 5-10 seconds. Move your hands further up against the wall, keep the same position of your hands and palms against the wall, and repeat the bend and hold. Return your hands to the starting position at shoulder level and repeat.
Prone leg raise
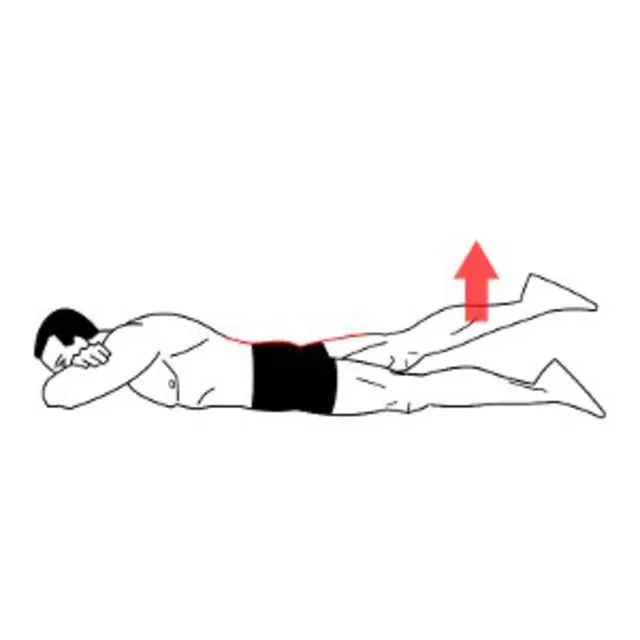
The prone leg raises exercise increases the strength of the thigh muscles. your lower lower back muscle tissue and your hips. This can assist in enhancing the manner you stroll or may also useful resource in achieving and preserving the right posture.
- Lie face down (prone position) on the floor.
- Gently tighten your center muscle tissue by maintaining your stomach muscle tissue engaged. You need to nevertheless be capable of breathing even as doing this.
- Keeping your abs engaged and your knees instantly, slowly carry one leg up backward. You need to hold your knee instantly as your thigh lifts from the floor.
- Hold your instant leg up inside the air for 2 seconds, after which slowly decrease your leg lower back to the floor. Be certain you no longer rotate your lower back or your pelvis even as you lift your leg.
- Perform the workout slowly for 10 to fifteen repetitions, after which repeat the workout for the alternative leg.
Hand exercise
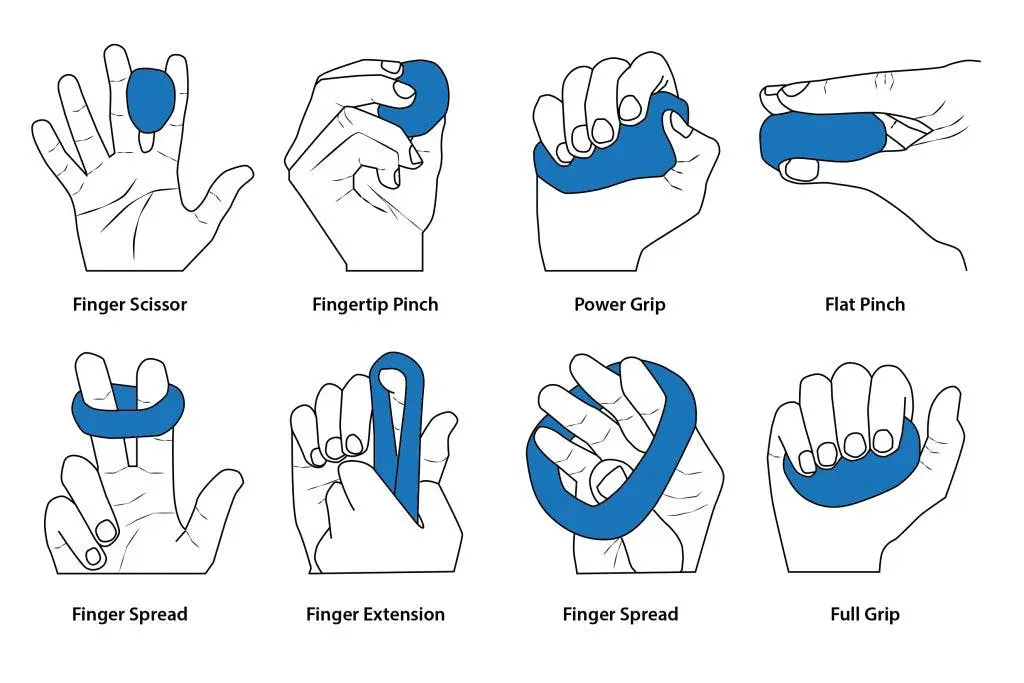
Hand therapy balls are a great tool for developing hand strength and fine motor skills. If you
If you have a neurological condition or are recovering from a stroke or surgery, these 5 simple handball exercises are for you.
- Squeeze the therapy ball with your hand and fingers as if you were making a fist. Then release it and open your arms as wide as possible. This improves hand strength for picking objects up. Squeeze the therapy ball with your thumb. and each end of the other finger. By doing this you train different muscles both internally and externally.
- Press the therapy ball onto the thumb with all fingers. This exercise gets stronger muscles that help you bend your fingers. It’s all about timing and skill.
- Place the therapy ball between two fingers. Press your fingers together and then release. It will also help to grasp objects. Place the therapy ball on the table, place your hands on it, and try to roll the ball sideways, up and down. This will help you practice with the right pressure on the ball.
Pelvic rotation
Pelvic tilt is an exercise that consists of very subtle movements of the spine that strengthen it
support the lower back, especially the abdominal muscles. They are good preliminary work
exercises for those looking for lower back pain and feel great because they give the back a
little massage.
- You can do hip flexion lying on the floor (hip flexion to a lying position), standing with your back against the wall, sitting on all fours, or on an exercise ball. All of these ways to bend your hips help strengthen deep muscles.
- Reclining the backrest is fine for most people, including those who are after birth When tilting your pelvis, you can lie on a firm bed, exercise mat, or floor if possible.
- This is the whole procedure of pelvic tilt. pelvic rotation increases mobility and improves core strength.
- start with the supine position and keep your spine neutral position.
- The natural curvature of the lumbar spine lifts the lower back slightly off the floor.
- now do expiration and take your hip towards your head.
- When you do this, you will feel your lower back press the floor. Stay here for a few breaths. When finished, inhale and return to neutral position.
- Do 5-10 repetitions.
Risk factors for Parkinson’s disease
Several environmental factors can increase the risk of Parkinson’s disease.
They include:
- Post-traumatic brain injury Reliable source: For example, head injuries from contact sports can increase the risk of the disease.
- Gender: Men are 50% more likely to develop the disease than women, although one 2016 study suggests that women’s risk may increase with age.
- Age: the disease often manifests itself from the age of 60.
- Some medications and drugs: Some medications can cause parkinsonism, where a person has tremors with any other symptoms of parkinsonism but does not have Parkinson’s disease. However, 5 to 10 percent of people with the disease have early-onset Parkinson’s disease, which begins before age 50.
Prevention
Parkinson’s disease cannot be prevented, but some lifelong habits can help reduce the risk.
- Avoiding toxins
If possible, individuals should take the following steps:
unnecessary use of pesticides and herbicides.
using alternatives to products that contain known toxins such as paraquat.
taking precautions, such as wearing protective clothing, if they cannot be avoided.
- Protect from head injuries
People can protect themselves from traumatic brain injury by:
with protective headgear during contact sports.
Use of a helmet while riding a bicycle or motorcycle.
Wear your seat belt when you traveling by car.
see a doctor if you have a concussion and avoid future risks until your doctor says it’s safe.
- Exercises
According to a 2018 review, regular physical exercise can help prevent or treat Parkinson’s disease.
- Nutritional factors
Certain food choices can also help reduce the risk of Parkinson’s disease and other diseases. Research has shown that the following remedies can help:
Turmeric: A mild spice that people can add to curries, soups, tea, and other foods. It contains curcumin, which is an antioxidant ingredient. some research has proven that it reduces the risk of having Parkinson’s disease by preventing oxidative stress and the aggregation of alpha-synuclein protein. Flavonoids: Studies show that this antioxidant can reduce the risk of Parkinson’s disease.
- Avoiding Aldehydes
Heating and recycling some cooking oils, such as sunflower oil, can cause the formation of aldehydes, which are toxic chemicals linked to Parkinson’s disease and other illnesses. A 2020 study suggests that potatoes fried in previously used cooking oil may have high levels of aldehydes.
Diagnosis and Tests
Diagnosing Parkinson’s disease is mostly a clinical process, which means it depends a lot on your doctor examining your symptoms, asking you questions, and reviewing your medical history. Some diagnostic and laboratory tests are possible, but they are usually needed to rule out other diseases or specific causes. However, most lab tests are not necessary unless you are responding to treatment for Parkinson’s disease and disease, which may indicate another disease.
What tests are used to diagnose this condition?
When healthcare providers suspect Parkinson’s disease or need to rule out other conditions, a variety of imaging and diagnostic tests are available. They include:
Blood tests.
Computed tomography (CT) scan.
Genetic testing.
Magnetic resonance imaging (MRI).
Positron emission tomography (PET).
New laboratory studies are possible
Researchers have found possible ways to test for possible indicators of Parkinson’s disease. Both new tests involve the alpha-synuclein protein but test it in new, unusual ways. Although these tests cannot tell you what diseases you have due to misfolded alpha-synuclein proteins, the information can still help your provider make a diagnosis.
The two tests use the following methods.
Spinal tap. One of these tests looks for misfolded alpha-synuclein proteins in the cerebrospinal fluid, which is the fluid that surrounds the brain and spinal cord. This test involves a spinal tap (lumbar puncture), in which a healthcare provider inserts a needle into the spinal cord to collect cerebrospinal fluid for testing.
Skin biopsy. Another possible test involves a biopsy of the superficial nerve tissue. A biopsy involves collecting a small sample of your skin, including the nerves in the skin. The samples come from one place on your back and two places on your leg. Analyzing the samples can help determine if there is a type of dysfunction in your alpha-synuclein that may increase your risk of Parkinson’s disease.
Management and Treatment
How is it managed or cured?
There is currently no cure for Parkinson’s disease, but its symptoms can be controlled in a number of ways. Treatment can also vary from person to person, depending on their specific symptoms and how well certain treatments work. medications are a great alternative way to manage this condition.
A secondary treatment option is surgery to implant a device that delivers a weak electrical current to part of the brain (called deep stimulation). There are also some experimental options, such as stem cell-based therapies, but their availability often varies and many are not options for people with Parkinson’s disease.
What drugs and treatments are used?
Medications for Parkinson’s disease are in two categories: direct treatment and symptomatic treatment. Direct treatments target Parkinson’s disease itself. Symptomatic treatment treats only the consequences of a certain disease.
Medicines
Medicines used to treat Parkinson’s disease do this in several ways. Therefore, drugs that do one or more of the following are most likely to:
Adding dopamine.
Medicines like levodopa can increase dopamine levels in your brain. This medication is almost always effective, and when it doesn’t work, it’s usually a sign of Parkinsonism in addition to Parkinson’s disease. Long-term use of levodopa eventually causes side effects that weaken its effectiveness.
Simulates dopamine.
Dopamine agonists are drugs that have dopamine-like effects. Dopamine is a neurotransmitter that causes cells to act in a certain way when they attach to a dopamine molecule. Dopamine agonists can bind and make cells behave the same way. They occur more often in younger patients to delay initiation of levodopa therapy.
Dopamine metabolism inhibitors.
Your body has natural processes that break down neurotransmitters like dopamine. Medications that prevent your body from breaking down dopamine make more dopamine available to the brain. They are particularly useful in the early stages and can also help with levodopa in the later stages of Parkinson’s disease and disease.
Inhibitors of levodopa metabolism.
These drugs slow down your body’s processing of levodopa, which helps it last longer. These drugs may need to be used with care because they can have toxic effects and can damage your liver. Most often, they are used as an aid when the effectiveness of levodopa decreases.
Blockers of adenosine.
Medicines that block certain cells from using adenosine (a molecule used in different forms throughout the body) can have a supportive effect when used with levodopa.
Several medications treat certain symptoms of Parkinson’s disease. Treatable symptoms often include:
1. Erectile and sexual disorders.
2. Fatigue or sleepiness. Constipation Sleep disorders.
3. Depression.
4. Dementia.
5. Anxiety hallucinations and other symptoms of psychosis.
Deep brain stimulation
In earlier years, surgery was an alternative to intentionally damaging and scarring the dysfunction caused by Parkinson’s disease. Today, the same effect is possible with deep brain stimulation, which uses an implanted device to deliver a weak electrical current to the same areas.
The main advantage is that deep brain stimulation is reversible, whereas intentional scarring is not. This treatment is almost always possible in the later stages of Parkinson’s disease when levodopa therapy wears off, and in people who have tremors that don’t seem to respond to standard medications.
Experimental treatments
Researchers are investigating other possible treatments that could help Parkinson’s disease. Although not widely available, they offer hope to people with the condition. Some experimental treatments include:
Stem cell transplantation.
They add new dopamine-using neurons to your brain to take over the damaged neurons. Treatments that repair neurons. These treatments attempt to repair damaged neurons and encourage the formation of new neurons. Gene therapies and gene-based treatments. Some also increase the effectiveness of levodopa or other treatments.
Complications or side effects are possible with the treatment
Complications and side effects of Parkinson’s disease treatment depend on the treatment itself, the severity of the condition, your other health problems, and more. Your healthcare provider is the best person to tell you more about possible side effects and complications. They can also tell you what you can do to minimize the impact these side effects or complications have on your life.
More about levodopa
The most common and effective form of treatment for Parkinson’s disease is levodopa. Although this drug has greatly improved the treatment of Parkinson’s disease, providers use it cautiously because it works. They usually also prescribe other medications that make levodopa more effective or help with side effects and some symptoms.
Levodopa is often combined with other medications to prevent your body from processing it before it reaches your brain. This helps prevent other side effects of dopamine, especially nausea, vomiting, and low blood pressure when standing (orthostatic hypotension).
Increasing the dose can help with this, but it increases the potential and severity of side effects, and the dose can only go so high before it reaches toxic levels.
Exercise Tips
- The best way to see the benefits is through consistent practice. People with PD who participated in exercise programs lasting more than six months, regardless of exercise intensity, showed significant improvements in functional balance and mobility compared to two- or 10-week programs.
- For exercise and PD, higher intensity may be of greater benefit. Experts recommend that people with PD, especially those who are young or in the early stages, exercise vigorously for as long as possible and as often as possible.
- intense exercise can increase the heart rate of the body. Research has focused on running and cycling, but experts believe that other high-intensity exercises such as swimming should provide the same benefits.
- Regardless of your fitness level, always stretch, warm up, and cool down properly. exercise is the last and great option for the condition. Know your limits. Many support groups, therapists, and exercise programs can help with PD-safe exercises or help you create your own program.
Training challenges
- People in the early stages of PD are usually as strong and physically fit as healthy people of the same age. The progression of Parkinson’s disease. it can lead to the following changes:
- Lack of muscle flexibility affects the balance of the body.
- Loss of muscle strength or rehabilitation can affect walking and the ability to rise from a sitting position.
- Decreased cardiovascular fitness, which affects endurance.
FAQ
Parkinson’s disease does not directly kill people, but the condition can put a lot of stress on the body and make some people more susceptible to serious and life-threatening infections. But thanks to advances in treatment, most people with Parkinson’s disease now have a normal or near-normal life expectancy.
Some studies have shown that regular aerobic exercise can reduce the risk of Parkinson’s disease and disease. Some other studies have shown that people who consume caffeine — found in coffee, tea, and cola are less likely to develop Parkinson’s disease than those who don’t.
Tremors, muscle stiffness, and slowness of movement are all common early symptoms of Parkinson’s disease, but there are other signs to look out for. Sleep and night problems are Parkinson’s disease and People with Parkinson’s disease are more likely to experience insomnia because of certain symptoms that can disrupt sleep.
Types of Parkinson’s disease and disease
Three main types of PD: idiopathic, early onset, and hereditary. Some conditions have similar symptoms and signs to PD but are caused by something else, such as a drug, stroke, or other neurological process.
there is a list of foods that are avoided if the patient is suffering from Parkinson’s disease.
Foods high in saturated fats.
Processed foods.
Large amounts of protein.
High citrus juices like orange juice.
Sugary foods and drinks.
Large amounts of alcohol.
References
- Parkinson’s disease. (2023, December 3). Wikipedia. https://en.wikipedia.org/wiki/Parkinson%27s_disease
- Parkinson’s Disease. (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/parkinsons-disease
- Brazier, Y. (2018, October 26). The signs and symptoms of Parkinson’s disease. https://www.medicalnewstoday.com/articles/323409
- Professional, C. C. M. (n.d.). Parkinson’s Disease. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/8525-parkinsons-disease-an-overview
- Exercise. (n.d.). Parkinson’s Foundation. https://www.parkinson.org/living-with-parkinsons/treatment/exercise
- Rogers, P. (2022, November 7). How to Do Biceps Curls: Proper Form, Variations, and Common Mistakes. Verywell Fit. https://www.verywellfit.com/how-to-do-the-biceps-arm-curl-3498604
- Pt, L. I. (2021, July 5). How to Do a Single Leg Stance. Verywell Fit. https://www.verywellfit.com/single-leg-stance-exercise-for-better-balance-2696233
- Zibutis, C. (2023, October 12). Benefits of the Heel Raise Exercise and How to Do It. Joggo. https://joggo.run/blog/benefits-of-the-heel-raise-exercise-and-how-to-do-it/
- Physiotherapy Exercise. (n.d.). https://www.physitrack.com/exercise-library/how-to-perform-the-tandem-walking-exercise
- No squeeze on the knees. (2012, July). British Dental Journal, 213(2), 85–85. https://doi.org/10.1038/sj.bdj.2012.644
- Cpt, P. W. (2022, November 25). How to Do Lunges: Proper Form, Variations, and Common Mistakes. Verywell Fit. https://www.verywellfit.com/how-to-lunge-variations-modifications-and-mistakes-1231320
- Cronkleton, E. (2020, November 24). How to Do Heel Slide Exercises. Healthline. https://www.healthline.com/health/exercise-fitness/heel-slides#how-to-do-it
- Pt, B. S. (2022, February 20). How to Perform the Prone Straight Leg Raise Exercise. Verywell Health. https://www.verywellhealth.com/the-prone-straight-leg-raise-exercise-2696522