Bone Tissue
Table of Contents
Introduction
Bone tissue is constantly remodelled by the coordinated actions of bone cells, including bone resorption by osteoclasts and bone formation by osteoblasts, with osteocytes acting as mechanosensors and orchestrators of the bone remodelling process.
This process is governed by both local (e.g., growth factors and cytokines) and systemic (e.g., calcitonin and oestrogens) factors, which all work together to maintain bone homeostasis. An imbalance in bone resorption and formation can lead to bone diseases such as osteoporosis. It has recently been discovered that bone cells communicate intricately during bone remodelling.
For example, the interaction of osteoclasts and osteoblasts facilitates the transition from bone resorption to bone formation. Furthermore, osteocytes produce factors that influence osteoblast and osteoclast activity, and apoptosis is followed by osteoclastic bone resorption. Growing understanding of the structure and functions of bone cells has contributed to a better understanding of bone biology.
It has been proposed that bone cells communicate with other organs in a complex manner, indicating the dynamic nature of bone tissue. In this review, we will look at the most recent research on the structure and functions of bone cells, as well as the factors that influence bone remodelling.
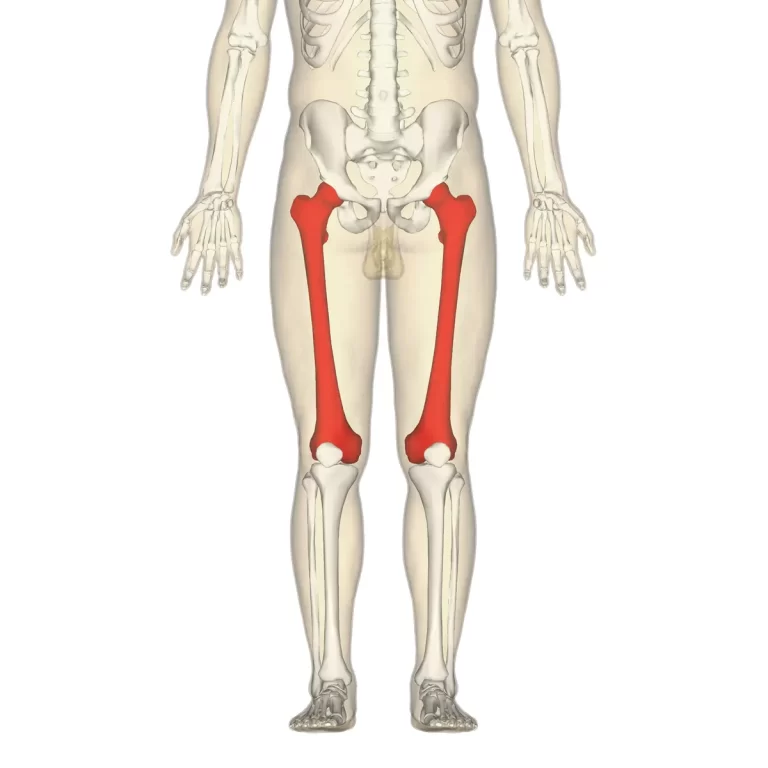
Bone Tissue Structure
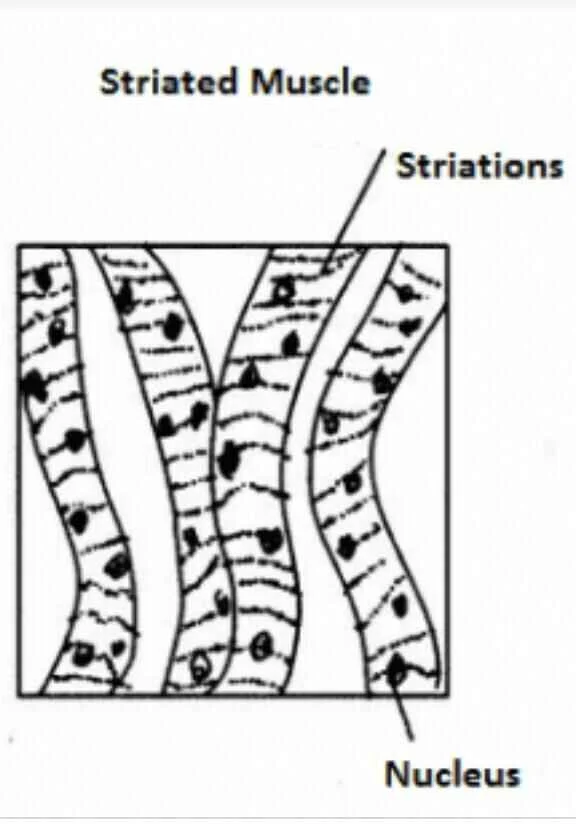
Bone tissue is classified into two types: compact and spongy. The names imply that the density, or how tightly the tissue is packed together, differs between the two types. Three types of cells help to maintain bone homeostasis.
Osteoblasts are cells that form bone, osteoclasts are cells that resorb bone, and osteocytes are mature bone cells. Bone tissue is controlled by the balance between osteoblasts and osteoclasts.
Compact bone
Compact bone is made up of closely packed osteons, also known as haversian systems. The osteon is made up of a central canal called the osteonic (haversian) canal that is surrounded by concentric rings of matrix (lamellae). The bone cells (osteocytes) are located in spaces called lacunae between the matrix rings.
To provide passageways through the hard matrix, small channels (canaliculi) radiate from the lacunae to the osteogenic (haversian) canal. The haversian systems in compact bone are compressed closely together to produce what comes to be a solid mass. In the osteonic canals, blood vessels run parallel to the long axis of the bone. Perforating canals connect these blood vessels to vessels on the bone’s surface.
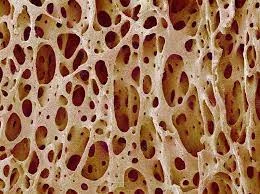
Bone Spongy (Cancellous)
Spongy (cancellous) bone is less dense and lighter than compact bone. Spongy bone is made up of plates (trabeculae) and bars of bone that are connected by small, irregular cavities containing red bone marrow. Instead of a central haversian canal, the canaliculi receive their blood supply from the adjacent cavities. The trabeculae may appear haphazardly arranged, but they are organised to provide maximum strength, similar to braces used to support a building. Spongy bone trabeculae follow stress lines and can realign if the direction of stress changes.
Bone Cells
Bone is a metabolically active tissue made up of various cell types. These cells include osteoblasts, which are responsible for bone tissue formation and mineralization, osteocytes, and osteoclasts, which are responsible for bone tissue reabsorption.
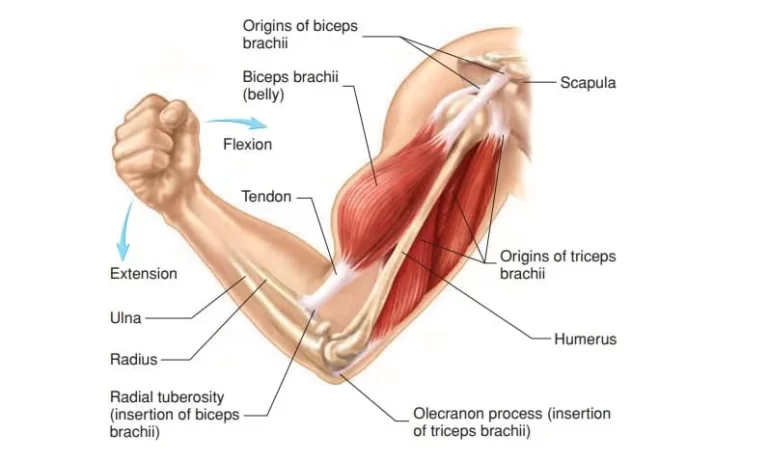
Osteoblasts
Osteoblasts are mononucleate bone-forming cells. They live on the surface of osteon seams and produce osteoid, a protein mixture that mineralizes to form bone. The osteoid seam is a narrow region of a newly formed organic matrix on the surface of a bone that has not yet mineralized. Type I collagen makes up the majority of osteoidOsteoblasts additionally create the hormones that act on the bone, including prostaglandins. The osteoblast builds around itself to create and repair new bone.
The osteoblast begins by forming collagen fibres. These collagen fibres serve as a framework for the work of the osteoblasts. The osteoblast then deposits calcium phosphates that are hardened by the presence of hydroxide and bicarbonate ions. The osteoblast produces new bone, which is known as osteoid. Once the osteoblast has completed its work, it becomes trapped inside the bone as it hardens.
When an osteoblast becomes trapped within a space (lacuna), it is referred to as an osteocyte. Other osteoblasts, known as lining cells, remain on the top of the new bone and are used to protect the underlying bone.
Osteocytes
Osteocytes are primarily dormant osteoblasts. Osteocytes are formed when osteoblasts migrate into and become trapped and surrounded by bone matrix that they produce. Lacunae are the empty spaces they occupy.
Osteocytes communicate by connecting to osteoblasts and other osteocytes. Osteocytes communicate with other bone cells via gap junctions, which are cell-to-cell attachments specialised for cell-to-cell communication that pass through small channels in the bone matrix called canaliculi.
Osteoclasts
Osteoclasts are multinucleate cells that are responsible for bone resorption, or the breakdown of bones. The osteoblasts then form new bone. Bone is constantly remodelled by osteoclast resorption and created by osteoblasts. Because osteoclasts are derived from a monocyte stem-cell lineage, they have phagocytic-like mechanisms similar to those found in circulating macrophages.
Osteoclasts develop and/or migrate to specific bone surfaces. Active enzymes, such as tartrate-resistant acid phosphatase, are secreted against the mineral substrate upon arrival. The reabsorption of bone by osteoclasts contributes to calcium homeostasis.
Extracellular Matrix
Living cells are embedded in a mineralized organic matrix to form bones. This matrix is made up of organic components, primarily type I collagen – “organic” refers to materials produced by the human body – and inorganic components, primarily hydroxyapatite and other calcium and phosphate salts.
Organic components account for more than 30% of the acellular portion of bone, with salts accounting for the remaining 70%. The tensile strength of bone is provided by collagen fibres, while the compressive strength is provided by interspersed crystals of hydroxyapatite. These effects work in concert.
The inorganic composition of bone (bone mineral) is primarily composed of calcium and phosphate salts, with hydroxyapatite (Ca10(PO4)6(OH)2 being the most abundant. The exact composition of the matrix may change over time due to nutrition and biomineralization, with the calcium-to-phosphate ratio varying between 1.3 and 2.0 (per weight), and trace minerals such as magnesium, sodium, potassium, and carbonate also present.
The organic matrix is composed of 90-95% type I collagen, with the remainder being a homogeneous liquid called ground substance, which contains proteoglycans such as hyaluronic acid and chondroitin sulphate, Non-collagenous proteins including osteocalcin, osteopontin, and bone sialoprotein, Collagen is made up of strands of repeating units that give bone tensile strength and are arranged overlappingly to prevent shear stress.
Functions of the Bone Tissue
In addition to locomotion, the classical functions of bone tissue include soft tissue support and protection, calcium and phosphate storage, and bone marrow harbouring. Additionally, recent investigations have focused on bone endocrine functions, which can have an impact on other organs. The osteocalcin produced by osteoblasts, for example, has been shown to act in other organs.
There are two types of osteocalcin: carboxylated and undercarboxylated. The carboxylated form has a high affinity for hydroxyapatite crystals and thus remains in the bone matrix during mineralization. Because of the acidification of the bone matrix during osteoclast bone resorption, the undercarboxylated form has a lower affinity for minerals and is transported by the bloodstream to other organs.
Undercarboxylated osteocalcin has been shown to have effects on the pancreas, adipose tissue, testis, and nervous system. In the pancreas, osteocalcin acts as a positive regulator of pancreatic insulin secretion and sensitivity, as well as pancreatic cell proliferation.
Osteocalcin stimulates adiponectin gene expression in adipose tissue, which improves insulin sensitivity. In the testis, osteocalcin can bind to a specific receptor in Leydig cells, increasing testosterone synthesis and, as a result, fertility. Osteocalcin also stimulates the synthesis of monoamine neurotransmitters in the hippocampus while inhibiting the synthesis of gamma-aminobutyric acid (GABA), which improves learning and memory.
Osteocytes promote another endocrine function of bone tissue. These cells can regulate phosphate metabolism by producing FGF23, which acts on other organs such as the parathyroid gland and the kidneys to reduce phosphate levels in the blood.
Osteocytes also have an impact on the immune system by altering the microenvironment in primary lymphoid organs, influencing lymphopoiesis. Not only osteocytes but also osteoblasts and osteoclasts, are known to have an impact on the immune system, primarily through bone inflammatory destruction. The discovery of the communication interplay between the skeletal and immune systems gave rise to a new field of study known as osteoimmunology.
Summary
Bone tissue is constantly remodelled by coordinated actions of bone cells, including bone resorption by osteoclasts and bone formation by osteoblasts. Osteocytes act as mechanosensors and orchestrators of the bone remodelling process, which is governed by both local and systemic factors. An imbalance in bone resorption and formation can lead to bone diseases such as osteoporosis. Bone cells communicate intricately during bone remodelling, such as the interaction of osteoclasts and osteoblasts facilitating the transition from bone resorption to bone formation.
Bone tissue is classified into compact and spongy types, with compact bone consisting of closely packed osteons and osteocytes located in spaces called lacunae between the matrix rings. Osteoblasts are cells that form bone, osteoclasts resorb bone, and osteocytes are mature bone cells. Bone tissue is controlled by the balance between osteoblasts and osteoclasts.
Osteoblasts are mononucleate bone-forming cells that live on the surface of osteon seams and produce osteoid, a protein mixture that mineralizes to form bone. Osteocytes are primarily dormant osteoblasts that migrate into and become trapped and surrounded by the bone matrix they produce. Osteoclasts are multinucleate cells responsible for bone resorption and reabsorption, contributing to calcium homeostasis.
The extracellular matrix of bone is composed of organic components, primarily type I collagen, and inorganic components, primarily hydroxyapatite and other calcium and phosphate salts. The tensile strength of bone is provided by collagen fibres, while the compressive strength is provided by interspersed crystals of hydroxyapatite.
Bone tissue functions for locomotion, soft tissue support, calcium and phosphate storage, and bone marrow harbouring. Recent research focuses on bone endocrine functions, such as osteocalcin produced by osteoblasts, which affects organs like the pancreas, adipose tissue, testis, and nervous system. Osteocytes regulate phosphate metabolism and impact the immune system, leading to osteoimmunology.
FAQs
This hard outer layer, also known as cortical bone, is strong and dense.
Compact bone tissue (also known as hard or cortical bone) and spongy bone tissue (also known as cancellous or trabecular bone) are the two types of osseous tissue.
The shape of bone cells can also change. Their shapes can be flat, round, cubical and columnar, stellar, or pancake-like. The most common bone cells found in bone tissue have protoplasmic projections and lacunae or small chambers.
Bone is made up of four types of cells: osteoblasts, osteocytes, osteoclasts, and bone lining cells. On bone surfaces, osteoblasts, bone lining cells, and osteoclasts are present and are derived from progenitor cells, which are local mesenchymal cells.
By increasing their resorptive activity, osteoclasts degrade bone to initiate normal bone remodelling and mediate bone loss in pathologic conditions.
References
- Structure of Bone Tissue | SEER Training. (n.d.). https://training.seer.cancer.gov/anatomy/skeletal/tissue.html
- Florêncio-Silva, R., Da Silva Sasso, G. R., Sasso-Cerri, E., De Jesus Simões, M., & Cerri, P. S. (2015, January 1). Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. BioMed Research International. https://doi.org/10.1155/2015/421746
- L. (2021, May 18). 5: Bone Tissue and Skeletal System. Medicine LibreTexts. https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Human_Anatomy_(OERI)/05%3A_Bone_Tissue_and_Skeletal_System
- Bone. (n.d.). Physiopedia. https://www.physio-pedia.com/Bone

One Comment