Quadriplegia: Cause, Symptoms, Diagnosis, Physiotherapy Treatment and Exercise
Table of Contents
What is Quadriplegia or Tetraplegia?
Quadriplegia, also known as Tetraplegia, refers to a form of paralysis from the neck down, including the trunk, and all four limbs. Most patients with quadriplegia are completely unable to move, and many have significant paralysis below the neck.
The condition is generally caused by an injury to the spinal cord level that contains the nerves that transfer motor and sensory messages from the brain to parts of the body. The situation basically begins in the spinal cord or brain or both. The spinal cord is sent signals to and from the brain, while the brain reacts to them and sends out new signals through the spinal cord. So, a spinal cord injury prevents the brain from receiving and sending these signals, whereas a brain injury reduces the brain’s ability to process them.
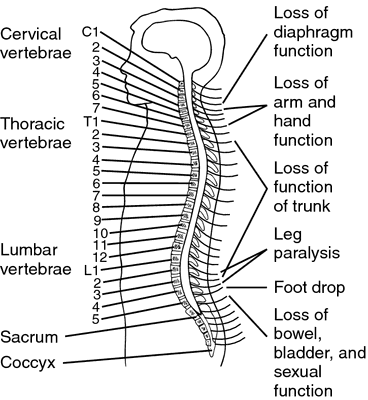
Quadriplegia is typically the result of damage at a high level in the spinal cord, generally in the cervical spine between C1-C7 levels. The higher the injury means the longer the damage will be. The spinal cord can not transmit messages below the affected area, which results in the loss of mobility in the legs and arms along with the loss of function in breathing, bladder, and bowel control.
Sometimes, spinal cord injuries to the C1 and C2 vertebral levels are frequent immediately fatal, or dangerous because of how they damage or disturb control over breathing and other critical functions. In some cases, a little movement can be regained by proper and effective intensive rehabilitation.
Symptoms of Quadriplegia
There are varying degrees of quadriplegia or tetraplegia, which include various levels of loss of control or muscle weakness, and symptoms vary from person to person.
Symptoms may include:
- The major symptom of quadriplegia is weakness or complete paralysis in all four limbs along with major muscles in the trunk. An individual with quadriplegia may have difficulty in controlling the muscles in the affected body parts.
- Numbness or loss of feeling sensation in the body, especially in the legs and arms
- Lack of firmness or Muscle limpness: It is called flaccid paralysis, muscles in a patient’s limbs can be soft or lack strength, but they can move easily or remain flexible
- Unusual muscle tightness or stiffness: It is called spastic paralysis or spastic quadriplegia, the muscles of a patient can appear unusually tight, stiff, and unable to move freely.
- Loss or lack of motor control: It is known as ataxia, in that a patient is unable to control the specific motions of his hands, arms, feet, or legs.
- Inability to walk: It is due to muscle weakness in the legs, walking may become challenging or difficult for a person with quadriplegia.
- Difficulty in breathing: It requires assisted breathing devices for quadriplegic patients
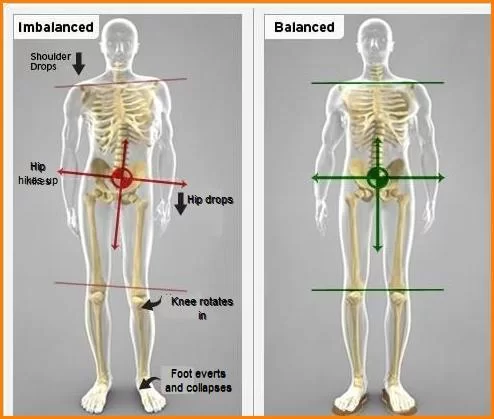
- Difficulty in sitting upright: It is because of an inability to balance
- Urinary retention or Loss of bladder control and bowel dysfunction: It is due to a lack of muscle control, loss of feeling and the closeness of the legs to the pelvis may affect the bladder.
- Reflex depression: It is because the nerves conducting messages from muscles to the brain are not functioning properly, the reflexes in the legs and arms may not be as quick or strong as they are typical.
Causes of Quadriplegia
Quadriplegia or quadriparesis is caused by an interruption in the nerves that send signals along with the spine between your body and your brain. These sensory and motor nerves pass through the spinal column. When the nerves are disturbed or damaged, the signals are changed.
There are various reasons why this condition can happen. Many individuals are born with a condition that affects their nervous system. Many develop this condition due to an accident or another medical condition or illness that damages the spinal cord or nerves.
Bacteria and Viruses can cause inflammation or attack nerve tissues in the body that result in damage to the nerves.
Examples of infections that can cause quadriplegia includes:
- enterovirus
- poliomyelitis
- Lyme disease
- flavivirus
- dengue fever
- diphtheria
- West Nile virus
- HIV
- hepatitis C
- Epstein-Barr virus
- Toxins/drugs
Some individuals are born with a condition known as a congenital disease, that affects their muscles and causes quadriplegia, such as:
- cerebral palsy
- Multiple sclerosis
- muscular dystrophy
- other conditions
Quadriplegia can be a complication of another underlying medical condition, which includes:
- locked-in syndrome
- Guillain-Barré syndrome
- Lambert-Eaton syndrome
- myasthenia gravis
- diabetic ketoacidosis
- para-neoplastic syndromes of the nervous system
- vasculitic neuropathy
- electrolyte disturbances, Such as hyperkalemia means high potassium, hypokalemia means low potassium, and hypophosphatemia means low phosphate
- Injury or trauma to the spine
Quadriplegia may occur after trauma or injury, which damages the spinal cord. Any kind of injury to the head, neck, or back can cause quadriplegia or quadriparesis if the nerves are subjected to enough damage. Such damage or injury can occur from:
- gun shoot injury
- car or motorcycle accidents
- sports injuries like football or hockey, impact sports, and diving in shallow water
- slips and falls while riding a bike or horse
- surgery of the spine
- herniated or slipped disk
Nerve damage can also occur as a result of a poison or toxin, or as a side effect of some medications.
Examples include:
- chronic alcohol abuse or alcohol poisoning
- scorpion sting
- botulism
- heavy metal poisoning
- snake venom
- tick paralysis
- Congenital conditions
- Some chemotherapy treatments
Nutrient imbalance
A number of kinds of imbalances of nutrients or vitamins in the body can cause quadriplegia.
For example, hyperkalemia, which means too much potassium in the blood can cause symptoms of quadriplegia. However, this kind of case can frequently be reversed quickly and fully.
Types of Quadriplegia
Many individuals think that all quadriplegic patients are the same—that none of them are able to move their legs and arms at all. But, there are several types of quadriplegia—including complete, incomplete, and spastic, flaccid quadriplegia that have some key differences.
Incomplete Quadriplegia
- Incomplete or partial quadriplegia refers to weakness but not fully paralysis in the legs and arms. It is also known as quadriparesis.
- An incomplete quadriplegic is different from a complete paraplegic in that they may still retain sensation in their legs arms and/or some function. This is the case with incomplete or partial spinal cord injury, some inherited conditions, and some traumatic brain injuries that caused quadriplegia.
- Some people with incomplete or partial quadriplegia may see improvement in their ability to control their limbs with certain quadriplegia exercises and therapies, which depend on the cause of the condition. While some patients with incomplete quadriplegia progress into complete quadriplegia as their condition progresses.
Complete Quadriplegia
- Complete quadriplegia refers to the total loss of muscular control in the legs and arms. It is a near-total form of paralysis where a patient is totally unable to move their limbs aside from their head. Depending on the underlying cause, Quadriplegia can also be either permanent, which means the paralysis will not subside, or temporary, which means the muscle control returns eventually.
- While compare to incomplete vs complete quadriplegia, the complete type of the condition is generally more severe. Exercise and recovery will be more difficult for a complete quadriplegic than for an incomplete quadriplegic.
Spastic quadriplegia
- Spastic hypertonia or Spasticity is a common side effect of brain and spinal cord injuries caused by disease or trauma. A spastic quadriplegic patient can not control their legs or arms consciously and may feel muscle spasms in their paralyzed limbs, increased tone, and jerking, especially when stretched. They may experience involuntary muscle tightness that makes it hard to move into a relaxed posture or hyperactive reflexes.
- Spasticity may be caused by cysts in the spinal cord that formed after spinal cord injury, other blockages, or, infections of the nervous system, so it is important to diagnose the cause of the quadriplegia by a qualified doctor and recommend an appropriate therapy protocol.
Flaccid Quadriplegia
- Flaccid Hypotonia or flaccidity causes muscles to lose their tone and become atrophied and flabby. It is also known as lack of firmness or Muscle limpness, in that muscles in a patient’s limbs can be soft or lack strength, but they can move easily or remain flexible.
Levels of Quadriplegia
Vertebrae Damage
Injury to the spinal cord is one of the most common factors, which cause quadriplegia. Generally, quadriplegia is the result of damage to the cervical portion of the spinal cord. Damage to the lower portion of the spine like the lumbar or thoracic spinal column typically results in paraplegia instead of quadriplegia. While the level of injury is higher up on the cervical spine, the more severe the effects are.
Here, are some brief knowledge of damage to various cervical spine vertebrae:
C1, C2, C3 level vertebral damage
- Highly severe the spinal cord injury levels
- Damage to nearest the skull is more likely to be fatal than damage lower on the spinal column. C1 and C2 level injuries are considered more severe because they are often fatal and affect respiratory function.
- Near-total paralysis in arms, hands, legs, and trunk
- A patient may not be able to breathe on her or his own, cough, which requires specialized devices to allow the injured person to breathe.
- Inability to control bladder or bowel movements.
- Speak ability is sometimes reduced or impaired
- Requires personal care 24-hour-a-day
C4 level vertebral damage
- Loss of diaphragm control, which requires breathing aids like a ventilator
- Paralysis or limited range of motion of the arms, legs, and torso
- Difficulty in bladder and bowel control
- Requires complete assistance with daily living activities, such as eating, bathing, dressing, and getting in or out of bed.
- Patients may be able to use powered wheelchairs with special controls to move around on their own
- Patients can not be able to drive a car on their own
C5 level vertebral damage
- Damage to the C5 vertebra may affect the vocal cords and may have talking problems
- They may be able to breathe unassisted but breathing can be weakened.
- Patients have some or total paralysis of hands, wrists, trunk, and legs but a person can raise his or her arms and bend elbows
- Patients need assistance with most daily living activities but in a power wheelchair, and can move from one place to another independently.
C6 level vertebral damage
- Injury to the C6 level spinal cord and below is less likely to cause total loss of the function of the arms.
- Paralysis in hands, legs, and trunk
- Little or no voluntary control of their bowel or bladder, but can be able to manage on their own with special devices
- A patient can speak and use the diaphragm, but breathing will be weakened
- Affection in wrist extension but a patient should be able to bend wrists back.
- A patient can be able to drive an adapted vehicle
- A patient can move in and out of a bed and wheelchair with assistive equipment
C7 level vertebral damage
- C7 level injury damage rarely results in quadriplegia except for other complicating factors.
- C7 spinal cord injury survivors may experience a burning pain in their shoulders, arms, back, and/or become paraplegic.
- Difficulty in finger extension and elbow extension.
- Most patients can straighten their arms and have normal shoulders movement.
- Patients can do most of the daily living activities on their own, but they may need assistance with more difficult tasks
- Patients can be able to drive an adapted vehicle.
- Patients have little or no voluntary control of the bladder or bowel, but may be able to manage on their own with special devices.
C8 level vertebral injury
- The patient has difficulty with some hand movements.
- The patient should be able to grasp and release things
Risk factors of Quadriplegia
It is essential to understand that a risk factor is different from a cause. It may not directly take part in the development of a Quadriplegia. A risk factor is that make circumstances that allow someone to suffer a quadriplegia-causing injury or make it possible or easier for a condition like quadriplegia to develop.
To exemplify the difference between a risk factor and a cause, consider a person falling off a tall ladder. On impact, the person breaks their cervical spine and loses feeling in their legs and arms, and becomes a quadriplegic. In this example, being on a tall ladder was the risk factor that most contributed to the fall, but the fall was the cause of quadriplegia.
certain risk factors that may predispose to the occurrence of spinal cord injuries and traumatic brain injuries leading to the development of quadriplegia, including:
Gender.
Men are more likely to suffer spinal cord injury which leads to quadriplegia than Women.
Age.
The particular age group at which risk for spinal cord injury or Traumatic brain injury is greatest has shifted over the years. People between the ages of 16 and 30 have more than half of spinal cord injuries occur. As people become aged, between 65 and older, they become more susceptible to severe Quadriplegia because they suffer from osteoporosis or other conditions that impact bone health, which leads to SCI and TBIs. In older adults, falls are the main reason to cause the condition.
Risky Behaviors.
Doing things like diving into too-shallow water, driving dangerously without wearing the proper safety gear, or taking proper precautions, such as without wearing seat belts or helmets.
Playing certain high-contact sports, such as rugby, wrestling, football, diving, gymnastics, ice hockey, surfing, and downhill skiing all leads to the risk of suffering a brain injury or spinal cord that leads to full-body paralysis.
Career Choice.
Some fields like construction workers, police officers, and professional athletes in high-contact sports all have an increased risk of injury from accidents or violence on the job. So, it puts them at a higher than average risk of becoming a quadriplegic.
Family Health History.
If a condition like ALS, Lou Gehrig’s Disease, runs in family, there is a risk of developing the same condition and losing control of legs and arms.
History of cancer also leads to pressure on the spinal cord
Diagnosis of Quadriplegia
A doctor can diagnose quadriplegia from the symptoms and perform a physical examination.
A patient may be referred to a neurologist for further testing.
Examination
The initial assessment of a person with acute quadriplegia should include a complete family and medical history, evaluate all of the symptoms of the person, neurological and physical examination to identify the level of injury as accurately as possible. It may conduct tests to assess nerve or muscle function along with an evaluation of the effectiveness of cough and breathing patterns. Isolated diaphragmatic breathing with chest wall retraction during inspiration is the most commonly seen abnormal breathing pattern.
More specific the sensory and motor neurological examinations of quadriplegia include:
It could be used for the assessment of sensation and muscles strength.
For the assessment of the upper limb in quadriplegia, the below-given tests are useful instruments. At least, one or a combination of these tools should be used for the assessment of the upper limb function and to plan treatment.
- Capabilities of the Upper Extremity instrument (CUE)
- The Sollerman hand function test
- The Quadriplegia Hand Activity Questionnaire
- The Motor Capacity Scale
Other tools include:
- Spinal Cord Injury Measure
- Functional Independence Measure
- Quadriplegia Index of Function
- Walking Index for Spinal Cord Injury
- Timed Up & Go
- Modified Barthel Index
- 6-min walk test
- 10-m walk test
Doctors may use various methods to diagnose causes of quadriplegia, which includes:
- Electrophysiological measures: strength-duration (SD) curve testing, evoked-potential testing, stimulated muscle testing, dynamic and needle electromyography (EMG) testing, and nerve conduction velocity (NCV) testing
- Electromyography (EMG) Tests are useful to identify nerve function to help differentiate between muscle and nerve disorders, which read electrical activity from the muscles.
- Nerve conduction velocity (NCV) studies to see how well muscles and nerves respond to small electrical pulses
- MRI scan of the brain and spine is used, to check if a patient has a brain tumor, herniated disk, or cysts in the spinal cord that may be disconnected signals from the brain.
- Spinal Taps or Lumbar Punctures. Doctors may need to collect some cerebrospinal fluid(CSF) from the spinal column to analyze it and check spinal health.
- Nerve or muscle biopsies, in that a small sample of nerve or muscle is removed for further testing in a laboratory
- Blood Tests. To check for deficiencies of vitamins, electrolyte imbalances, and diabetes, or to check for genetic markers that could indicate that a congenital condition that causes quadriplegia was inherited.
Treatment of Quadriplegia
The goals of quadriplegia treatment include reduction of immediate threats or problems to the quadriplegia patient’s health and life, improvement of the long-term prognosis, and teaching the spinal cord and brain how to work around the injury.
Non-surgical treatment options for quadriplegia include medicines to relax muscle spasms, the use of medical devices such as wheelchairs, braces, walkers, etc; physical therapy, occupational therapy, and speech or language therapy.
Members of the rehabilitation team
Taking care or treating patients with quadriplegia is subject to the nature and severity of the patient’s condition and it involves addressing functional loss and feeling in particular areas of the body and may include organ function loss or impairment.
Neurologists: make a diagnosis and treats diseases related to paraplegia, quadriplegia, and other conditions related to the brain, spinal cord, spinal column, peripheral nerves, and nervous system.
Physiotherapist: works to maintain and improve activity in the muscles and keep them strong. Even if the case is extreme, the dormant muscles still need exercise for support of the body.
Occupational Therapists: They have trained and have the education and skill required to perform the task of taking care of quadriplegic patients. They arrange meetings to facilitate achievement by goal setting while taking into context social, occupational, and physical factors; provide care, which initiates from the ICU through to acute hospitalization.
Psychologists: They deal with SCI can be devastating for the patients as well as family members. A psychologist helps the patient handle behavioral and emotional issues.
Nurses: They help to rehabilitate patients by working with them on problems related to bladder or bowel dysfunction including the managing of pressure ulcers.
Speech/language pathologist: a licensed therapist helps the patient management issues with speech, communication, language disorders, and swallowing problems.
Social workers and case managers: interface between the patient and family members, payer source, and the rehabilitation team.
All members of the rehabilitation team are supervised by a physician and although each member has an assigned primary role, a properly functioning team usually has interdisciplinary members who can take part in resolving problems. Therapy continues in outpatient settings, allowing patients to venture into new challenges, improve on their newly acquired skills; and increase participation in every aspect of life.
Therapy options:
- Medication to reduce the risk of infection along with that other drugs, like blood pressure medicines or blood thinners.
- Spinal cord and brain surgeries to reduce bleeding, relieve obstructions, and manage any swelling.
- Family education and support.
- Education about quadriplegia, along with that training on the rights of patients under the Americans With Disabilities Act and other relevant laws.
- Physiotherapy help patients regain functioning and keep their bodies in optimal health.
- Occupational skills training.
- Speech and language therapy to help patients regain or maintain their ability to speak.
- Psychotherapy helps patients deal with the psychological and social effects of quadriplegia. Drugs such as antidepressants might also recommend.
- Participation in support groups and social groups.
Surgical Management
When conservative treatments fail to reduce pain and spasticity, at that time only surgery is recommended.
Intrathecal Baclofen Therapy
A tiny pump filled with Baclofen which is a muscle relaxant is placed in the abdominal wall and the drug is pumped into the spastic muscles of the limbs.
Dorsal Rhizotomy
It is a surgical procedure to reduce spasticity and improve muscle movements, that involves cutting a few nerves at the roots where they divide from the spinal cord.
Tendon Transfer Surgery
This procedure is performed to restore hand function after quadriplegia. The origin of the functional hand muscle is detached and reinserted into a different tendon or bone to improve function.
Procedures such as the transfer of biceps to triceps for elbow extension and the teres minor motor branch for triceps reinnervation can give the patient a functional improvement.
Respiratory Management
- Patients who have lost their ability to breathe on their own are ventilated through a tracheotomy and are more likely to get a respiratory disease and/or infection. For that, the use of expiratory flow devices is advisable, and secretion removal techniques and the improvement of various components of cough such as flow rate, vital capacity, and maximum respiratory pressures are recommended.
- To prevent atelectasis or as a treatment, Intermittent positive pressure breathing (IPPB) can be used. A diaphragm pacing system is a better technique, which electrically stimulates the phrenic nerve to pace the diaphragm. Inspiratory muscle training at low loads with a threshold trainer increases the respiratory muscles strength of the quadriplegic patients.
Physiotherapy treatment
The aim of the physiotherapy treatment is functional recovery. Exercises for quadriplegia patients can be useful for limiting muscular atrophy because of inactivity, reducing the occurrence of sores, and pain relief from spastic muscles. It can also help to promote mental well-being and cardiovascular health. Apart from exercises, some therapists suggest lifestyle modifications that may be important for a patient’s health, fitness and wellness.
If the physician and surgeon decide to do surgery, the task of the physiotherapist will be to reinforce the muscle and teach the patient to control his muscle individually.
Treatment start with passive movement, followed by active-assisted movement, active movement, and resisted movement of all four limbs.
Passive Range of Motion Exercises for Quadriplegic patients
Physiotherapists give stretching to the patient’s limbs to restore movement after spinal cord injury.
All patients with quadriplegia can practice passive range of motion exercises that requires no exertion of energy from the patient. Instead, a physiotherapist, trained caregiver, or occupational therapist will facilitate the patient’s movements to make sure that the patient’s joints move to their full range.
Additional benefits include improved flexibility, blood flow, and reduced pain after spinal cord injury. It provides a perfect opportunity for the therapist or caregiver to check for any skin integrity issues that may be developed.
Generally, each exercise should be done on each side of the body, ideally multiple times a day. Mainly, a slow stretching motion with 15-20 second hold at the end range of motion is most effective.
Upper limb rehabilitation
The ability to use the upper limbs is considered essential to regain the independence of the patient like independent transfers, the use of a wheelchair, pressure relief maneuvers, etc. So, a physiotherapist should set personal goals for each patient and use a specific suitable training program to gain success. Functional electrical stimulation with task-specific training is ideal to improve the hand function if the grasp function is too weak.
Often, patients with quadriplegia and their rehabilitation teams mainly focus on improving upper-body mobility. so, a patient can essentially improve their independence with daily living activities and use their hands and arms to assist with mobility of the lower body.
Some additional quadriplegic exercises focus on developing upper-body mobility and strength.
Neck Tilts: Tilt the patient’s neck so that the left ear moves towards their left shoulder and then do the same for the right side. Important note: if patients wear a neck brace of any kind or have been told to have “cervical spinal precautions,” do NOT perform this exercise and talk to a physiotherapist and/or doctor about when a patient can try it.
Side to Side Head Shake: Turn the head from side to side look like saying ‘no’; the eyes should stay level the entire time.
Shoulder Raises: Shrug shoulders up towards ears and then bring them back down.
Shoulder Rolls: Roll shoulders backward and forward
Arm Rows: Put both arms straight in front of the patient and bend their elbows back.
Arm Across Body: Bring one arm out across the chest and use the other arms to hold it there.
Arm Raises: Raise arm towards the ceiling as high as a patient can. But, if a patient has cervical spinal precautions, do not raise arms any higher than shoulder height.
Arm Circles: Raise arms to the side so that patient’s body makes a “T” shape and moves them in little circles forward and backward.
Hallelujahs: Lift both arms out towards the sky.
Arm Flaps: Make a “T” shape with the patient’s arms raised to the sides and move them up and down.
Elbow Flexion and Extension: Bend the elbow so the hand touches the shoulder. Then extend it so the arm is straight.
Wrist Flicks: Move the hand forward so the palm moves towards the inner arm and makes a 90° angle. Then, move the hand back in the opposite way. If the patient has some hand movement and is working on the use of a “tenodesis grasp” in therapy, then keep their fingers curled in instead of fully extended while performing this wrist exercise.
Palm Flips: Put arm out straight in front of a patient with their palm facing down and then flip it so that palm faces up. This can also be done with the elbow bent at the patient’s side.
Finger Clenches: Make a fist and clench all fingers together. Then, open the hand and stretch out fingers as much as the patient can.
Fists: Curl the fingers inward towards the palm, make a fist, and extend them back so that the patients are straight. Keep the wrists neutral or straight while doing this.
O’s: Touch the tip of the thumb to the tip of the each finger
Finger Splits: Separate two adjacent fingers away from each other and then bring them back together
Lower limb rehabilitation
Advance techniques like the use of functional electrical stimulation lower extremities treadmill gait, cycling, and electrical stimulation during gait are used to maintain or regain muscle mass in the legs, strengthen the bones, and achieve many other benefits from physical activity.
The below-given hip and knee passive range of motion exercises should be performed in a lying down position.
Hip Circles: Bend one knee so the thigh is perpendicular to the bed and make a 90° angle with the knee. After this rotate the hip in circles by moving and holding the thigh.
Foot Claps: The legs are in a straight position. Pull one leg to the side, creating separation between the feet until the patient feels slight resistance. Then, bring your feet back together.
Knees to Chest: With one hand on the upper leg just above the knee and the other on the foot, bend one knee so it reaches towards the chest. After that, bring the foot back to the other leg and straighten the knee.
Ankle Rotations: Put one hand above the ankle to stabilize the leg and the other hand on the foot. Then move or rotate the foot in circular motions.
Toe Curls: Bend the toes in towards the sole and bring them back out to normal, which can be done in a supine or sitting position.
Torso Twist: Gently twist the patient’s upper body to one side while keeping their lower body still in the same. If patients wear a neck brace or back brace of any kind or have been told that they have “spinal precautions,” do NOT perform this exercise and talk to a physiotherapist and/or doctor about when they can try it.
Cardiovascular rehabilitation
Hypotension and orthostatic hypotension is frequently seen in quadriplegic patients; a patient should be instructed to get up from a seated position or a lying slowly and gradually. Before standing up, circulatory exercises can be helpful in the blood flow stimulation.
For the respiratory issues, which come with quadriplegia:
Use of expiratory flow devices, and secretion removal techniques are recommended and the improvement of various components of cough such as Vital capacity, flow rate, and maximum respiratory pressures are recommended.
Intermittent positive pressure breathing (IPPB) can be used to prevent atelectasis or as a treatment.
Inspiratory muscle training at low loads with a threshold trainer increases the strength of the respiratory muscles in quadriplegic patients.
Bed mobility and transfer activity
Bed mobility and transfers are important functional activities that patients with a spinal cord injury need to master in order to independent mobility and QoL.
When retraining functional activities include strength training, practice frequently, practice sub-tasks, and making sub-tasks progressively harder with appropriate instructions and sufficient feedback, demonstrations, and manual guidance.
Importance of mobility exercises
- Pressure Relief
- Transferring to Sitting
- Dressing
- Changing Position in Bed
- Prep for transferring to a wheelchair
- Functional activities with Upper limbs
- Transferring from bed or chair to the wheelchair.
- Transferring from wheelchair to chair/ car/ toilet etc.
Rolling
Swinging the UL towards the opposite direction of the roll, while lifting and rotating the head.
Mobilizing from Supine to Long Sitting
Roll to side-lying and lift the trunk off the bed by pushing through one or bilateral UL. Then, Straight UL and transfer the Center of gravity over the hips.
Unsupported Sitting
Unsupported sitting can either belong to sitting with legs straight or short sitting with legs over the edge of the bed.
Vertical Lift
Position hands near to the body, then lift by extending the elbows, depress, and adduct shoulders.
Transfers
Horizontal Transfers
Move to the front sitting surface and position the wheelchair near, place the palms on the lower back and push the pelvis forwards, legs up with elbow flexion hook, One hand on the wheelchair wheel and the other on the bed. Shift and lift across the bed
Vertical Transfer
Position the legs of the patient, then position the hands with the lead hand forward and away from the trunk and the trail hand close to the hip, Lift and rotate the body, position the buttocks in the wheelchair and move into an upright position.






4 Comments