Soft Tissue Injury: Symptoms, Grades, Types, and Treatment.
Table of Contents
What do you mean by soft tissue injury? or
Definition of soft tissue injuries:
In soft tissue injury, our body’s anatomical structures like Ligaments, muscles, capsules, and fascia, may get injured by the injury.
In our body anatomical structures like Ligaments, muscles, capsules, fascia, Or bursa all are considered soft tissues.
Due to some specific mechanism, these anatomical structures may get injured.
So the structures are impaired by the injury and they limit their routine or normal function.
What kind of symptoms are seen after soft tissue injury?
- Pain
- Swelling or edema was noted in the surrounding area.
- Visible bruising can be seen
- Limited movement of the affected joint.
- Muscular weakness noted.
- Muscle spasm is seen in the relevant area.
- Joint instability is seen in severe injuries
Which structures get impaired during soft tissue injury?
Following structures get commonly injured.
- Ligaments
- Muscles
- Tendons
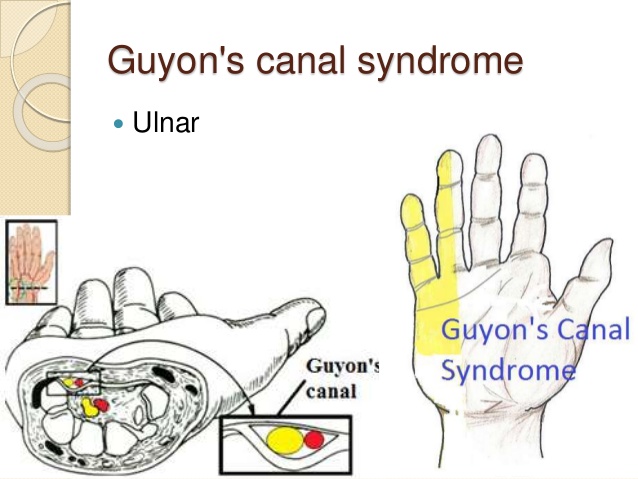
- Nerves
- Bones
- Cartilage
Classification of soft tissue injury:
They are classified according to the duration of an injury.
so basically they are divided into two :
Acute injuries
Overuse injuries
Both the types are described here in detail.
Acute injuries:
- Most commonly this kind of injury occurs suddenly.
- so it is called acute injuries.
- This type of injury occurs because of the following mechanisms.
- sudden trauma
- fall from height
- Twisting of body
- Blowing to any body part
- Few examples of this type of injury :
- Acute ankle sprains
- Muscular strains
- contusions
Overuse injuries:
- This type of injury occurs because of Frequent and repeated activities.
- So because of these repeated activities, the soft tissue does not get proper timing for healing.
- So it is called overuse injuries.
- Mostly the duration will be chronic because of overuse.
- Here are some examples of this type of injury:
- Bursitis
- Tendinitis
What are the Grades of the severity of soft tissue injuries?
The severity of soft tissue injuries is mainly divided into three Grades:
Grade-1 or First degree
Grade-2 or Second degree
Grade-3 or Third degree
Grade -1 :
- Characteristics of grade-1 are described here.
- The patient feels mild pain at the time of injury, or within the first 24 hours.
- A mild amount of swelling is seen.
- Tenderness is seen over the local area.
- The patient feels pain while doing movement of that soft tissue.
Grade-2:
- Characteristics of grade-2 are described here.
- The patient feels a moderate amount of pain.
- stressful activities increase the level of pain.
- Here, some fibers of soft tissue get torn because of injury.
Grade-3:
- Characteristics of grade-3 are described here.
- Complete tear or near-complete tear of soft tissue is seen with the help of investigations.
- the patient feels more or more severe pain.
- Sometimes avulsion of the tissue is also seen.
- So because of the complete tear of soft tissue, instability of joint is also commonly seen.
What are the different types of soft tissue injuries?
Here is the list of some types of soft tissue injuries, all are described below in detail.
- Muscular strains
- Ligament sprains
- Dislocation of joint
- Subluxation of joint
- Muscles or Tendons rupture or tear
- Tenosynovitis
- Tendinitis
- Tenovaganitis
- Tendinosis
- Synovitis
- Hemarthrosis
- Ganglion
- Bursitis
- Contusion
- Contractures
- Muscle guarding
- Muscular spasm
Muscular Strains:
- Definition:
- injury to the muscle or tendon is commonly called strain.
- Mechanism of injury:
- The most common mechanism is overstretching overexertion, and overuse of soft tissue.
- Causes:
- sudden unusual action may tear the muscle fiber.
- direct trauma to the muscle.
- repeated trauma or minor degree.
- Types:
- Acute muscular strains:
- occurs because of sudden force or direct trauma to the muscle.
- Chronic muscular strains:
- it occurs because of injury existing for a prolonged period.
- here, muscular fibrosis and ischemia occur because of the prolonged period of injury.
- Grades of muscular strains:
- Grade-1:
- the patient is having pain.
- Grade-2:
- the patient is having pain and muscular weakness.
- Grade-3:
- the patient is having to complain of pain, muscular weakness, and loss of function.
Muscle or Tendon Pathologies:
It includes muscular or tendon tears or ruptures.
- There are 2 conditions :
If partial tear or rupture occurs :
Pain will be felt during resisted activity. - If a complete or full tear or rupture occurs :
The movement will not occur.
Muscle fibers are not able to pull against resistance.
Pathologies of Tendons:
- Tenosynovitis :
- Inflammation of synovial membrane which is the covering or the tendon.
- Tendinitis :
- Inflammation of a tendon.
- Tenovaganitis :
- Inflammation with thickening of the tendon sheath.
- Tendinosis :
- Degeneration of tendon due to repetitive microtrauma.
- It occurs because of the aging process.
Ligament sprain:
- Introduction:
- ligaments are made up of collagen fibers.
- They are arranged in longitudinal directions.
- The vascularity of ligaments is very poor, so they always heal by replacement of scar tissue.
- so injury to the ligament is commonly termed as Sprain.
- The function of the ligament:
- it provides support, stability, and protection to the joint.
- Types of Ligament Sprain:
- there are mainly three types of ligament sprain.
- Grade-1
- Grade-2
- Grade-3
- All grades are described below in detail.
- Grade-1 Ligament sprain:
- Characteristic:
- the patient is having to complain of slight pain over the site of injury.
- A mild amount of tenderness is seen.
- mild swelling present.
- slight over-stretching and small tears are present.
- Grade-2 Ligament sprain:
- Characteristic:
- Large but incomplete tears are present.
- most commonly the ligament may be found partially torn.
- more amount of swelling is present.
- more pain and tenderness are seen.
- loss of normal joint function.
- weight-bearing of an adjacent joint becomes affected.
- Grade-3 Ligament sprain:
- Characteristic:
- occurs because of severe violence.
- the gross amount of swelling present.
- more severe pain and tenderness.
- joint become totally unstable so a total loss of function.
- so it is defined as a complete rupture of the ligament.
Synovitis:
- Definition:
- Inflammation of the synovium is called synovitis.
- Basic anatomy of synovium and its functions:
- Synovium is the covering of the joint capsule or tendon sheaths.
- it has to reach the blood supply and nerve supply.
- it produces a fluid called as Synovial fluid
- functions of synovial fluid:
- it provides smooth and frictionless movement to the joint.
- it also helps in the nourishment of cartilages.
- Types of Synovitis:
- mainly two types are seen:
- Acute synovitis
- Chronic synovitis
- Acute synovitis:
- Mostly occurs because of trauma.
- Pain is present over injured structures.
- Swelling of the joint is seen.
- There will be the presence of temperature rise and redness.
- Chronic synovitis:
- firm swelling is present.
- mild pain but ligaments become lax as compared before.
- instability of joint is seen.
- Muscle atrophy is present.
Bursitis:
- Definition:
- Inflammation of the bursa is called Bursitis.
- Basic anatomy:
- Bursa is the membranous sac lined with a synovial membrane situated at the ends of bones where tendons pass over them.
- Functions of bursa:
- prevent friction between two structures.
- prevents wear and tear of muscles and tendons.
- it protects structures from pressure and injury.
- Causes of bursitis:
- following is the list of possible causes of bursitis.
- Trauma
- Infection
- Metabolic disorder
- Abnormal external pressure
- Inflammatory disorder
- Common sites for bursitis:
- in the upper limb:
- subacromial
- olecranon
- in lower limb:
- prepatellar
- tendoachillies
- medial great toe
- the lateral side of the little toe
- Clinical features:
- The patient is having to complain of pain.
- Swelling is present over the site.
- The movement of the joint is very painful.
- Tenderness is also sometimes present.
Tenosynovitis:
- Definition:
- Inflammation of the synovial sheath surrounding the tendon is defined as tenosynovitis.
- There are mainly two types of tenosynovitis is seen.
- Irritative and Infective
- Irritative:
- It occurs because of abnormal or excessive frictional force applied over the tendon and its the surrounding sheath.
- clinical symptoms:
- pain present over the site of injury.
- tenderness is also seen.
- crepitus present on palpation.
- Infective:
- most commonly occurs because of the acute or chronic type of infection.
- EX: Acute infections like acute pyogenic infections
- Chronic infections like TB.
Contusions:
- Definition:
- Brushing resulting from mechanisms like a direct blow will result in rupture of capillary, bleeding, and edema.
- and inflammatory response is seen during this type of soft tissue injury.
- Symptoms:
- the patient is having to complain of pain.
- swelling is present.
- limitation of joint movement.
- discoloration of skin mostly bluish type discoloration is seen.
- Muscular Weakness
- Causes:
- The contusions usually result from a direct blow from a person or firm contact with equipment in collision sports, such as football, basketball & hockey.
- The blow causes local muscular damage so bleeding occurs.
- The most common site of muscle contusions is over the quadriceps muscle.
- This injury is known as a ‘cork thigh’ or ‘Charley horse’.
Ganglion:
- Definition:
- Ballooning of the wall of the tendon sheath or joint capsule is known as a ganglion.
- Another name: Bible cyst
- Overview:
- It is the swelling that often appears on or around joints and tendons in the hand or foot.
- The size of the ganglion cyst varies sometimes.
- The most common site is found around the Dorsum of the wrist and on the fingers.
- it may also arise after trauma, and is sometimes seen in the cases of rheumatoid arthritis.
Dislocation and Subluxation:
- Definition:
- Dislocation: It is the place where two or more bones attach together is called a joint.
- When the bones in a joint become separated or come out of their normal positions, then dislocation occurs.
- Any joint in the body can be dislocated via certain mechanisms.
- Subluxation:
- If the joint is dislocated partially, it is defined as a subluxation.
- Symptoms:
- The patient is having a severe amount of pain if the joint is totally dislocated from its anatomical position.
- Swelling surrounding the site
- Bruising present
- The affected joint becomes unstable.
- Loss of normal movements of joint
- The visible deformity is present.
Hemarthrosis:
- Another name: Articular bleeding
- Definition:
- Bleeding occurs in the joint cavity.
- Symptoms:
- Mostly tingling or aching type of painful sensation present in the joint
- Tenderness present
- Marked amount of swelling
- redness seen
- warmth and hot on palpation
- stiffness present
- More bruising was seen near the affected joint
- Affected joint range of motion
- Overview:
- It can occur after an injury to the Joints.
- it causes pain and swelling of the joint.
- If not treated early, can lead to permanent damage to the joint.
Tendinitis:
- Definition:
- The Tendon is the thick and fibrous cord that attaches muscle to bone.
- Tendinitis is defined as an inflammation of the tendon itself.
- Symptoms:
- The patient is having dull aching type of pain.
- Tenderness is present over the site of injury.
- Mild swelling is seen surrounding the injured site.
What is the Treatment plan for soft tissue injuries?
The Treatment plan for soft tissue injury depends on the duration of an injury.
It is mainly classified into Three Stages:
Acute stage
Subacute stage
Chronic stage
All the stages of tissue healing are described below in detail.
Goals and Treatment plan during an Acute stage:
Overview:
An acute stage lasts up to 4 to 6 days after an occurrence of soft tissue injury.
It is also called an Inflammatory stage of tissue healing.
Tissue response during inflammatory stage:
- During this stage cellular, vascular, and chemical responses in the tissue.
- During the first 48 hours after injury to soft tissue, vascular changes occur.
- Exudation or emission of fluid of cells from the blood vessels occurs.
- Formation of clot occurs.
- During this period, the following activities begin to place.
- Neutralization of the present chemical irritants
- Phagocytosis of dead tissues
- The fibroblastic activity of soft tissue begins.
- Formation of the new capillary.
- These physiological processes serve as a protective mechanism as well as a stimulus for subsequent healing and repair.
- Usually, this stage lasts 4 to 6 days.
Common clinical symptoms are seen during an Acute stage:
- Pain
- Inflammation,
- Edema
- Muscular spasm
- Impaired joint movement
- Joint effusion
- Decrease use of associated area
Goals of Treatment:
- To educate the patient about the condition.
- To control pain edema and muscle spasm.
- To Maintain joint integrity and mobility.
- To reduce the level of present joint swelling.
- To Maintain integrity and function of associated areas also.
It is described below in detail.
To educate the patient about the condition:
Inform patient about recovery time and how to protect the part while maintaining appropriate functional activities.
To control pain edema and muscle spasm:
Use RICE protocol to control pain and edema.
Avoid positions of stress to the injured part.
Immobilize the injured part.
so use PRICE protocol as an initial treatment tool.
PRICE stands for:
- P stands for : Protection
- R stands for : Rest
- I stands for : Ice
- C stands for : Compression
- E stands for : Elevation
Protection:
- Protecting the injured area from further injury is a key to treatment.
- In this phase, the use of support is recommended.
- Ex: By using crutches to protect the lower limb from injuries.
- It is important to protect the injured area to avoid further tissue damage.
- For an example :
- If you hurt your knee while playing cricket, so you need to stop playing cricket to protect your injured area.
- Protection also helps to give an appropriate amount of rest for the healing process.
Rest:
- It is recommended to avoid or stop the use of injured or affected body parts.
- Here are a few benefits of resting position:
- Because of the resting position, the injured or affected body part will remain in the immobilization position.
- So it will prevent further injuries.
- And it will also provide time for early recovery or healing process of damaged soft tissue.
- How can give the resting position to the affected area?
- With the help of the following devices, you can give a resting position.
- Braces
- Canes
- Crutches
- According to the area involved you can prescribe the device.
- For an example:
- Splints are used for upper limb injuries.
- Braces are used to immobilize the knee joint and surrounding structures.
- Canes are also used to immobilize your forearm region while walking at a shorter distance.
- Crutches are used to support your upper limb.
- It is remembered to avoid movements of the body part and keep the weight off from the affected area.
Ice:
- It is also known as ‘ Cryotherapy ‘
- Application of cold will reduce pain by making the affected area numb.
- What type of physiological effects can be seen after the application of cold?
- Cold reduces Tissue metabolism.
- So by this phenomenon, there will be constriction of the blood vessels.
- The application of ice will also decrease the nociceptive propagation of stimulus to the brain.
- Which will reduce pain sensations.
- It will also help to reduce muscle spasms occurred because of soft tissue injury.
- You can apply ice with the help of the following:
- Ice packs
- Ice bags
- Before application of ice packs or ice bags, wrap them in a cloth or towel whatever is available.
- It will help to prevent frostbite. so before applying make sure it does not touch the skin directly.
- In emergency situations, you can also use ice bags of frozen vegetables.
- What is the procedure for the application of ice?
- Apply ice over the injured area for approximately 10 to 15 minutes.
- or for 4 to 8 times in a while day.
- It will definitely help if you will apply it within the first 3 to 4 days of injury.
- Always remember that never allow the ice packs or bags to directly touch the skin.
- What will happen if you apply ice for a prolonged duration?
- It may reduce or decrease excessive blood flow into the applied area.
- It will cause skin burns because the nerves present under the area will get damaged.
- In which conditions you can not apply ice therapy?
- or Contraindications of ice therapy:
- The patient was diagnosed with Raynaud’s syndrome.
- Diabetic patients
- Patients having urticaria from the cold application.
- Paroxysmal cold hemoglobinuria
- Circulatory insufficiency is already present.
- Hypersensitivity from cold.
Compression:
- It is given with the help of elastic bandages, by wrapping the bandage around the injured area.
- Elastic bandages should provide comfortable compression force without causing pain and constriction of blood vessels.
- It should not be too loose or too tight.
- It is important to wrap it from the distal to the affected area and then move in a proximal direction.
- Method of application:
- The figure of the eight methods.
- If you find that skin below the wrapped area changes its color like blue or you feel cold, numb, or tingling kind of sensations in your affected extremity so you need to lose your bandage immediately.
- If symptoms do not get normal, then take medical help.
- Because when it will be too tight, it will interrupt your normal blood flow.
- What are the benefits of compression?
- It will keep the swelling or edema under control by the pressure of elastic bandages.
- It will also help to provide support to the affected extremity or area.
- It will help to reduce the loss of blood flow from the damaged tissue.
- Will also reduce the further accumulation of the swelling or edema in surrounding structures as well as the affected areas.
- Procedure:
- After injury giving compression for at least one week will be more effective to reduce the amount of swelling.
- Wrap your bandage tight enough only to support your injured area.
- Apply it from distal to proximal direction.
- Apply it like that it should stop the blood flow from injured blood vessels.
Elevation:
- Here you need to elevate your injured area.
- Keeping the affected area elevated, will reduce the amount of swelling or edema for sure.
- For upper limb injuries, you need to elevate your affected extremity above the level of your heart.
- For lower limb injuries, you need to elevate your affected extremity above the level of the pelvis.
- What are the Physiological effects of elevation?
- It will prevent further swelling by increasing the venous return.
- It will also help to reduce hydrostatic pressure.
- It will increase the amount of removal of waste materials from the site of injury.
- Will also help to reduce pain and discomfort associated with soft tissue injuries.
- What are the uses of elevation?
- By elevation of the injured area, it will make the difficulty for blood to reach up to that area.
- So there will be a reduction in loss of blood flow.
- After the injury, it is best to elevate the area for 2 to 3 hours a day.
- Gentle (grade I) joint oscillations with a joint in a pain-free position.
- Indication:
- Lower-grade joint oscillations are used to reduce pain and irritability of soft tissue.
To Maintain joint integrity and mobility:
- Begin to do Passive movements within the limit of pain.
- It is done specifically to the structure involved.
To reduce the level of present joint swelling.
- Provide appropriate protection to reduce the amount of swelling.
- Protecting the injured area from further injury is a key to treatment.
- In this phase, the use of support is recommended.
- Ex: By using crutches to protect the lower limb from injuries.
- It is important to protect the injured area to avoid further tissue damage.
- For an example :
- If you hurt your knee while playing cricket, so you need to stop playing cricket to protect your injured area.
- Protection also helps to give the appropriate amount of rest for the healing process.
- Rest is recommended to avoid or stop the use of injured or affected body parts.
- Here are a few benefits of resting position:
- Because of the resting position, the injured or affected body part will remain in the immobilization position.
- So it will prevent further injuries.
- And it will also provide time for early recovery or healing process of damaged soft tissue.
- How can give the resting position to the affected area?
- With the help of the following devices, you can give a resting position.
- Braces and Splint
- Canes
- Crutches
- According to the area involved you can prescribe the device.
- For an example:
- Splints are used for upper limb injuries.
- Braces are used to immobilize the knee joint and surrounding structures.
- Canes are also used to immobilize your forearm region while walking at a shorter distance.
- Crutches are used to support your upper limb.
- It is remembered to avoid movements of the body part and keep the weight off from the affected area.
To Maintain integrity and function of associated areas:
- Active-assisted range of motion exercises of associated joints.
- It totally depends on proximity to associated areas and the effect on the previously injured area.
What to avoid during the treatment of the acute stage of healing of soft tissue injury?
- The proper dosage of rest and movement must be used during this stage.
- Too many movements can increase the level of pain and inflammation.
What you should not perform during the acute stage of soft tissue injury?
- Stretching and resistance exercises should not be performed at the site of the inflamed tissue.
Goals and Treatment plan during the Subacute stage:
Overview:
- It lasts up to 14 to 21 days.
Tissue response during Subacute stage of soft tissue healing :
- During the second to fourth days after tissue injury, the inflammatory process begins to decrease.
- The clot has now started resolving.
- The injured site begins to heal.
- This usually lasts for an additional 10 to 17 days and14 to 21 days after the onset of the injury.
- It may last up to 6 weeks sometimes.
- Fibroblasts are present from the fourth day after injury and continue for 21 days.
- Wound closure occurs 5 to 8 days in muscle and skin and 3 to 6 weeks in tendons and ligaments.
Common clinical symptoms are seen during a Subacute stage:
- During the subacute stage, the signs of inflammation progressively decrease and eventually become absent.
- The patient may experience pain and tissue resistance at the end of the available ROM.
- Pain occurs only when tight tissue is stressed.
Goals of Treatment:
- To Promote healing of injured tissues.
- To Restore soft tissue, muscle, and/or joint mobility
- To Develop neuromuscular control, muscle endurance, and strength in the affected and surrounding adjacent muscle groups.
- To Maintain joint integrity and function of associated in nearer areas.
It is described below in detail.
To Promote healing of injured tissues:
- Monitor response of tissue to exercise progression.
- Decrease intensity of exercises, if inflammation increases.
- Protect healing tissue with assistive devices like splints, tape, or wrap.
- Progressively increase the amount of time the joint is free to move each day.
- Decrease use of the assistive device as strength improves in supporting adjacent muscles start improving.
To Restore soft tissue, muscle, and/or joint mobility:
- Do progression in your previous treatment protocol.
- Progress from initial passive movements to an active-assisted range of motion.
- Perform active ROM within limits of pain if possible.
- Gradually increase the mobility of scar tissues.
- Progressively increase the mobility of tight structures.
- Use appropriate techniques specific according to the tight structure.
To Develop neuromuscular control, muscle endurance, and strength in affected and surrounding adjacent muscle groups:
- Initially, progress exercise protocol with the help of multiple-angle isometric exercises according to the patient’s tolerance.
- Begin always with a mild amount of resistance.
- Then Initiate an Active range of motion with protected weight-bearing and stabilization exercises.
- As healing and functional joint range improve, progress isotonic exercises with an increase in the number of repetitions of movements.
- Emphasize control and proper biomechanics.
- Progress the amount of resistance later in this stage.
To Maintain joint integrity and function of associated in nearer areas:
- Apply progressive strengthening and stabilizing exercises.
- Start low-intensity functional activities involving the healing tissue without exacerbation of the symptoms.
What to avoid during the treatment of the Subacute stage of healing of soft tissue injury?
- The signs of inflammation are normally found to decrease early in this stage.
- Some discomfort will occur as the activity level is progressed, but it should not last longer than several hours.
- Signs of too much motion or activity are the following:
- Resting pain
- Fatigue
- Increased muscular weakness
- muscular spasm
Goals and Treatment plan during Chronic stage:
An Overview:
- It lasts up to 21 to 60 days.
- Another name: Remodeling stage
- Tissue response during maturation and remodeling stage:
- Scar retraction from the activity of the myofibroblasts is usually complete by the 21st day and the scar stops increasing in its size.
- From day 21 to day 60 there is a predominance activity level of fibroblasts so they are easily remodeled.
- This whole process begins during the late subacute stage and continues for more than several months.
- The remodeling stage is developed by factors that affect the density and activity of the fibroblast.
- It includes the amount of following:
- Duration of immobilization.
- The stress placed on the tissue,
- Location of the lesion
- Vascular supply to the tissue.
- Common clinical symptoms are seen during this stage of tissue healing:
- No signs of inflammation were seen during the chronic stage.
- There may be the formation of contractures that limit the range of motion.
- Muscle weakness limits normal function.
- The patient feels stretch type of pain when testing tight structures at the end of their available range.
- Routine functions of the patient are limited because of present Muscular weakness, poor endurance, or poor neuromuscular control.
Following are the goals of this stage:
- To Educate the patient.
- To Increase the level of mobility of soft tissue, muscle, and joint
- To Improve neuromuscular control, strength, and endurance
- To Progress in the level of functional activities.
To Educate the patient:
- Instruct your patient on safe progressions of exercises and stretching.
- Monitor understanding and compliance.
- Teach ways to avoid reinjuring the part.
- Teach safe body mechanics.
- Provide ergonomic counseling to the patient.
To Increase the level of mobility of soft tissue, muscle, and joint :
- Stretching techniques specific to tight tissue are indicated.
- Progression in specific joint mobilization techniques.
- To break adhesions of Ligaments and tendons use the cross-fiber massage technique.
- Progressive flexibility exercises specific to the joint.
To Improve neuromuscular control, strength, and endurance:
- Progress in previous exercise protocol:
- Give Submaximal to maximal resistance.
- concentric and eccentric exercises,
- From Single plane motion to multiplane motions.
- Emphasize movements that simulate functional activities.
- Teach Safe biomechanics.
- Increase the duration of progression and complexity gradually.
To Progress in the level of functional activities:
- Continue to use your assistive devices until the ROM has become functional and strength in supporting muscles is adequate.
- Progress level of functional training by the activities from protected and controlled movements to unprotected and variable movements.
- Continue progressive strengthening exercises.
- Advanced training activities until the muscles are strong enough and able to respond to the required functional demands.
What to avoid during the treatment of the Chronic stage of healing of soft tissue injury?
- There should be no signs of inflammation.
- The patient will feel Some amount of discomfort as the activity level is progressed, but it should not last more than a couple of hours.
- Signs of activities progressing too quickly or with an increase in dosage are joint swelling and pain which lasts more than 4 to 5 hours or that requires medication for relief.
- So do progression gradually.






One Comment