Tensor Fascia Latae Pain
Table of Contents
What is a Tensor Fascia Latae Pain?
Pain in the tensor fasciae latae can manifest as a dull ache or sharp pain on the outer hip or the front of the thigh. This discomfort may be exacerbated by activities that involve hip movement, such as walking or climbing stairs.
Introduction
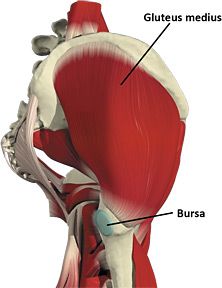
The tensor fasciae latae (TFL) is a hip muscle that connects to the lower leg via the IT band. It is located above the gluteus minimus and a portion of the medius.
The TFL muscle aids in the hip’s flexion, abduction, and medial rotation. It works to help the gluteus medius and minimus stabilise the pelvis by controlling movement rather than producing it.
Tensor fasciae latae trigger points and tightness can cause hip joint pain and anterolateral thigh pain that can extend to the knee. Walking or lying down on the affected side can aggravate the pain, which can feel like deep hip pain. Because the trigger point referral pattern goes over where the femur connects to the acetabulum in the hip at the greater trochanter, it can be confused with trochanteric bursitis.
Trigger points in the iliopsoas, rectus femoris, and TFL are common causes of hip flexor pain.
TFL tightness can cause muscle shortening, which pulls on the IT band. This can result in problems such as IT band syndrome and external snapping hip syndrome.
IT band syndrome is a common overuse injury that can occur during repetitive hip flexion activities such as running or cycling. IT band pain can be relieved in some cases by relaxing the TFL, gluteus maximus, and vastus lateralis muscles.
The term “external snapping hip syndrome” refers to a snapping or clicking sensation in the lateral hip caused by the IT band “snapping” over the greater trochanter. Easing tension in the TFL, gluteus maximus, and vastus lateralis can help with this problem because it relieves tension in the IT band, which prevents friction over the greater trochanter.
Origin, Insertion, and Nerve Supply of the Tensor Fascia Latae
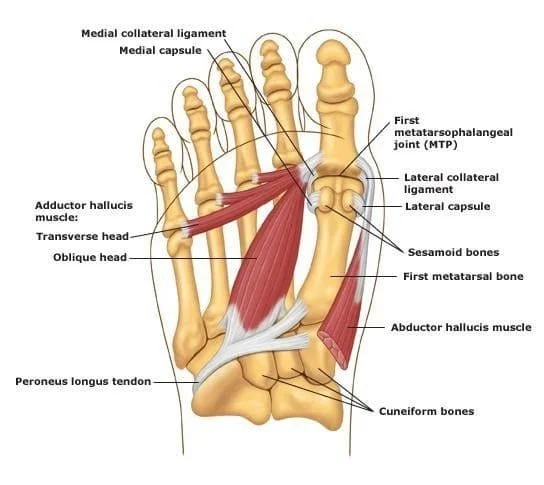
The anterior superior iliac spine (ASIS) and the anterior aspect of the iliac crest give rise to the TFL. It descends between and is attached to the IT band’s deep fascia and superficial fascia (5 cm width). The TFL runs superficially to the greater trochanter of the femur from the anterolateral aspect of the thigh.
It connects distally to the IT track/band, which is made up of the gluteus maximus fascial aponeurosis and the tensor fascia latae. The IT band then runs down the lateral side of the thigh, connecting to the lateral condyle of the tibia, specifically the Gerdy tubercle.
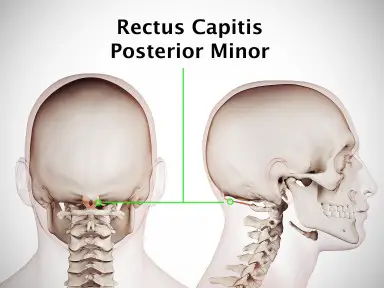
Innervation: The superior gluteal nerve, which arises from the roots of lumbar nerves 4, 5, and the first sacral nerve (L4-S1), innervates the Tensor fasciae latae. It also innervates the gluteus minimus and medius muscles before reaching the tensor fasciae latae muscle.
Function of the tensor fascia latae
Despite its small size, the TFL collaborates with several muscle groups to aid in hip and knee movement and stabilization:
Internally rotates and abducts the hip with the gluteus medius and gluteus minimus, and abducts the hip with the gluteus maximus via the IT band. It assists the rectus femoris in hip flexion.
Acts on the tibia via the IT band’s attachment to the lateral tibial Gerdy tubercle. The TFL is an accessory knee flexor, but its action is not visible until the knee is flexed past 30 degrees. Furthermore, it collaborates with the IT band to stabilize the knee in full extension. It also participates in lateral tibial rotation via the IT band. When kicking a football, the hip may be in abduction and medial rotation, allowing for this lateral rotation.
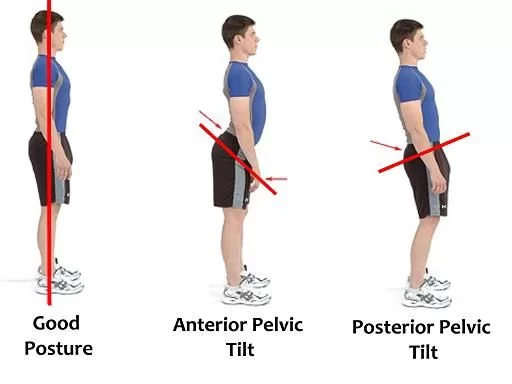
Clinically, the TFL’s primary function is to aid in walking. The TFL accomplishes this by inferiorly pulling the ilium on the weight-bearing side, causing the contralateral hip to rise. During the swing phase of the gait, the rise in the non-weight-bearing hip allows the leg to swing through without hitting the ground.
What causes pain in the Tensor Fasciae Latae?
TFL pain can occur as a result of overuse or when this muscle attempts to compensate for weaker surrounding muscles. Muscle pain can occur when your muscles work unusually hard. Surrounding muscles that are dysfunctional can also cause severe pain. TFL injury can result from the repetition of the following activities:
- Cycling, Swimming, and Kayaking
- Running and walking
- Long periods of sitting
- Long kicking and driving
- Standing tall with a swaying back
- Frequently wearing high heels
- Taking a nap in the foetal position
- Meditation with crossed legs
The 3-Step AER System is a Better Strategy for TFL Pain.
Instead of focusing solely on the TFL, I recommend taking a broader view of the hips. Which foundational hip movements do you struggle with? How can we assist you in improving this movement? What type of exercise does your body prefer?
There is no one-size-fits-all solution. Each suffering from TFL and hip pain will be weak in different movements. Individual responses to various exercise strategies will also differ.
This is why I advocate for the AER 3-Step-System, which stands for Assess, Execute, and Reflect. The premise of AER is that every person’s body is unique. As a result, different strategies will be required for each individual to get moving and feel better.
Step 1: Asses Your Hip Limitations
The first step is to evaluate. Determine your physical limitations. Before making any conclusions, it is critical to test all six foundational hip movements. When I work with clients, I go through all six assessments, even if the first few movements are problematic.
For two reasons, we’ll concentrate on hip flexion and hip internal rotation in this tutorial. To begin, pain in the TFL area indicates that these two movements may be weak. Second, if we went through each of the six major hip movements, this tutorial would be 10,000+ words long. It is critical to identify your low-hanging fruit. This allows you to focus your efforts on the most important movements.
These are only two introductory assessments. To get a better picture of your hip function, I recommend testing the other four main hip movements. You may also require more advanced evaluations. The result will set it off to an ideal start.
Want new exercises delivered to your inbox every week? Sign up for my movement journal below to get started on the path to healthier hips and more consistent movement practice.
Step 2: Execute an Effective Training Plan
The second step is to devise and carry out a training plan that is tailored to your specific needs. The majority of active people participate in sports or have some experience with popular exercise modalities. Strength training, conditioning, and yoga are all beneficial, but I’m talking about something else.
I’m referring to a smart training plan that focuses on improving your movement. This type of training aims to loosen up movement patterns. It is not to gain muscle, lose weight, or improve athletic performance. These are fantastic goals, but they are not the same as movement improvement.
Assume you perform poorly on both the hip flexion and hip internal rotation assessments shown above. Your exercise programme would then include exercises aimed at improving internal rotation and hip flexion. Here are two exercises that I frequently assign to beginner clients who are weak in these movements:
A training programme can last from 4 to 8 weeks. I usually give beginners four weeks to get a feel for training in these types of structured phases. People are also tempted to give up too quickly. When we don’t see results, it’s easy to become discouraged and abandon ship.
However, progress takes time. We must determine what works and what does not. Trial and error is a part of the process, and what works well for one person may be useless for another.
The exercises listed above have proven to be beneficial to many of my clients. They do not, however, assist everyone. This is why the third step is so critical: reflect and reassess.
Step 3: Reflect and Reassess
Reflection on the training plan necessitates a two-pronged approach.
We begin by assessing your subjective experience with the training plan. What aspects of the training plan did you think worked well? Where do you believe you have made the most progress? Where do you believe you received the most bang for your buck? What were your difficulties? What seemed to be a waste of your time?
We then objectively assess your progress by reassessing the movements we are attempting to improve. In our example, we’d retest your hip flexion and internal rotation after 4 weeks of working through the exercises.
Things are unlikely to change after just one training phase, but they may after two or three. The goal is to have recorded videos of the target ranges of motion and notice a gradual improvement in them. We use both of these metrics to decide which exercise strategies to keep and which to drop.
Consider an example of how this might work. In a 4-week training phase, you perform the reverse clamshell twice a week. You mentioned in the reflection stage that the exercise was awkward and uncomfortable. This is your personal experience.
After that, we reassess and discover that your internal rotation has improved. It’s possible that the discomfort you felt during training was necessary to get you moving more efficiently. Perhaps there was nothing to fear at all.
Treatment for the tensor fasciae latae pain
Overall, the treatment of TFL pain is similar to that of tendinopathy.
To begin, we recommend reducing or avoiding activities that aggravate your hip pain. Hiking and running are two common examples of these activities. To maintain fitness, you can then cross-train with cycling and swimming. Finally, as the pain improves, you can incorporate a progressive running programme to keep pain levels low.
TFL workouts
TFL enthesopathy is commonly associated with pelvic muscle weakness. As a result, you should work closely with a therapist to improve weaknesses. Hamstring bridges, crab walks with a band, and step-ups are examples of exercises. We generally recommend exercising every 2-3 days.
As previously stated, identifying and treating the underlying cause of TFL pain is critical. Rest, ice, stretching, and strengthening exercises from physiotherapy can frequently help relieve pain. Most of the time, consulting with a physiotherapist is required to develop an appropriate treatment plan and ensure a proper diagnosis. They can also advise on how to avoid future TFL pain.
Foam roller self-myofascial release:
- Lie on your side with the foam roller horizontally placed just below your hip on the outer thigh, close to the gluteus maximus and lateral side.
- Support your upper body with your forearm and stabilize with your other leg.
- Roll slowly along the outer thigh, from just below the hip to just above the knee, through the TFL trigger points.
- When you find a tender spot (trigger point), pause for 20-30 seconds and apply gentle pressure to allow the muscle to relax.
- Continue rolling and pausing on other sensitive areas.
Self-myofascial release with a massage ball:
- Alternatively, you can apply more targeted pressure to specific areas with a massage or tennis ball.
- Position the ball between your hip and a firm surface (such as the floor or a wall).
- To locate trigger points, apply pressure to the ball and roll it over the TFL area.
- When you find a tender spot, apply pressure to it for 20-30 seconds to allow the muscle to relax.
Stretching the TFL
- Place your feet shoulder-width apart.
- Cross one leg behind the other and lean to the opposite side slightly.
- Maintain a straight crossed leg and a flat foot on the ground.
- You should notice a stretch on the outside of your hip.
- maintain the stretch for 20-30 seconds before switching to the other side.
Stretching the hip flexors
Because the hip flexors and TFL are interconnected, stretching the hip flexors before exercise can indirectly release tension in the TFL.
- Kneel on one knee and step forward into a lunge position with the other foot.
- Tuck your pelvis in and push your hips forward gently.
- A stretch should be felt in the front of your hip on the side of the kneeling leg.
- maintain the stretch for 20-30 seconds before switching to the other side.
Dry Needling or TFL Massage
Seeking the assistance of a Sports Physiotherapist who can specifically target the TFL and surrounding areas can provide a more targeted and thorough release.
It is critical to use gentle pressure when performing these techniques. Before attempting these self-release techniques, consult with a healthcare professional or a Melbourne Physiotherapist if you have any underlying injuries or medical conditions. They can offer tailored advice and ensure that the exercises are safe and appropriate for your needs.
Other tensor fasciae latae pain treatments
TFL pain can persist even after a period of reduced activity and exercise. In these cases, we add treatments to help but not harm the tendon. Overall, we recommend non-invasive treatments first because the risks are lower.
Tendonitis GTN patch
Nitric oxide is present in GTN patches. We know that nitric oxide plays an important role in tendon healing. Nitric oxide is transferred to the swollen TFL tendon by placing the patch on the skin over it.
Recent research suggests that nitric oxide patches can help with tendinopathy pain. We generally recommend using these patches for 2-3 months.
Shockwave treatment
We believe that TFL pain responds better to shockwave therapy than other tendons. As a result, we recommend five sessions spread out over five weeks (one session per week) in addition to exercise.
Injections for pain in the tensor fasciae latae
In general, injection therapy is more invasive and unpredictable than alternative treatments. However, injections are occasionally used to treat TFL pain that has not responded to other treatments.
Low-dose cortisone is our first-line injection treatment. The cortisone is then directed just above and below the area of thickening using ultrasound. As a result, the injection is more effective and has fewer side effects. Skin atrophy and depigmentation are two common side effects of TFL injections. In general, using ultrasound reduces the likelihood of these cortisol side effects.
Needle tenotomy and PRP are two other injection options. However, there is no proof that these injections help with TFL pain. NSAIDs should be avoided for at least two weeks following needle tenotomy or PRP. If you’ve recently received a cortisone injection, you should wait at least a month before undergoing a needle tenotomy or PRP injection.
Summary
The Tensor Fasciae Latae (TFL) is a hip muscle that aids in hip flexion, abduction, and medial rotation. It works to stabilize the pelvis by controlling movement rather than producing it. TFL trigger points and tightness can cause hip joint pain and anterolateral thigh pain that can extend to the knee. TFL tightness can cause muscle shortening, which pulls on the IT band, resulting in problems such as IT band syndrome and external snapping hip syndrome.
IT band syndrome is a common overuse injury that can occur during repetitive hip flexion activities. TFL pain can result from repetitive activities such as cycling, swimming, kayaking, running, walking, long periods of sitting, long kicking and driving, standing tall with a swaying back, frequently wearing high heels, taking a nap in the foetal position, and meditation with crossed legs. To address TFL pain, it is recommended to take a broader view of the hips, assess hip limitations, and execute an effective training plan tailored to individual needs.
A training program lasting 4-8 weeks can benefit many clients, but progress takes time, and trial and error is essential. Reflecting and reassessing the training plan is crucial, as it helps determine which exercise strategies to keep and which to drop.
Treatment for tensor fasciae latae pain is similar to tendinopathy and includes reducing activities that aggravate hip pain, incorporating progressive running programs, and working with a therapist to improve weaknesses.
Non-invasive treatments like nitric oxide patches, shockwave therapy, and injections are recommended, with low-dose cortisone being the first-line treatment. However, NSAIDs should be avoided for at least two weeks following injections, and patients should wait at least a month before undergoing a needle tenotomy or PRP injection.
FAQs
The tensor fasciae latae (TFL) is a muscle in the proximal anterolateral thigh that connects the superficial and deep iliotibial (IT) band. The length of the muscle belly varies greatly, but in most patients, the TFL muscle belly ends before the greater trochanter of the femur.
This muscle’s primary function is to produce leg extension and lateral rotation at the knee joint. It also helps with thigh movements by acting as a relatively weak abductor and medial rotator on the hip joint.
The superior gluteal nerve, L4, L5, and S1 supply their TFL. The superior gluteal nerve arises from the anterior rami of L4-S1 and runs superior to the piriformis before exiting the pelvis through the greater sciatic foramen with the superior gluteal artery and vein.
TFL serves as a secondary hip flexor, abductor, and internal rotator. It applies force directly to the hip and indirectly to the knee via its insertion into the ITB.
The use of a spikey massage ball to target the TFL is an excellent way to self-manage tightness and provide relief. If your muscles are too sensitive, you can perform this self-massage while lying face down or standing.
References:
- Tensor Fascia Lata. (n.d.). Physiopedia. https://www.physio-pedia.com/Tensor_Fascia_Lata
- Levarda, T. (2023, September 24). Acupuncture for Tensor Fasciae Latae Pain — Morningside Acupuncture NYC. Morningside Acupuncture NYC. https://www.morningsideacupuncturenyc.com/blog/acupuncture-for-tensor-fasciae-latae-pain
- 3 Steps for Eliminating Tensor Fascia Latae Pain. (n.d.). https://www.maksreznik.com/blog/3-steps-for-eliminating-tensor-fascia-latae-pain
- S. (2023, December 7). Everything You Need to Know About TFL Injury – Find All Information. Southgate physio. https://www.southgatephysio.co.uk/everything-you-need-to-know-about-tfl-injury/
- D. (2021, August 27). Tensor Fasciae Latae Pain | How To Eliminate Nagging Hip Pain. Back Muscle Solutions. https://backmusclesolutions.com/blogs/the-ql-blawg/tensor-fasciae-latae-pain
- The team, E. P. (2023, November 14). Why do I have Tensor Fasciae Latae pain? — Evolutio Melbourne. Melbourne Sports Physio | Sports Medicine | Richmond Physiotherapy Clinic – Evolutio. https://www.evolutio.com.au/blog/2014/9/16/3-reasons-the-tfl-muscle-affects-your-squat