Tidal Volume
Table of Contents
What is a Tidal Volume?
Tidal volume refers to the volume of air that is inspired or expired with each breath during normal, quiet breathing. In other words, it represents the amount of air that moves in and out of the lungs during a single breath cycle, without any additional effort or forceful inhalation or exhalation.
It is typically 500 mL in healthy adult males, compared to 400 mL in healthy females. It is an essential clinical parameter that enables appropriate breathing to occur. Oxygen from the environment enters the lungs as someone breathes in. In order to enter arterial circulation, it then diffuses over the alveolar-capillary contact.
As long as metabolism continues, carbon dioxide will continue to produce concurrently. Carbon dioxide is expelled during respiration to keep it from building up inside the body. Physiology refers to tidal volume as the amount of air that is inhaled and exhaled that contributes to maintaining constant levels of oxygen and carbon dioxide in the blood.
Tidal volume is a vital parameter because it provides valuable insights into the efficiency and health of the respiratory system. It is measured in milliliters (ml) or liters (L), depending on the context, and can vary among individuals based on factors such as age, sex, and overall lung health. Understanding tidal volume is essential for diagnosing and monitoring respiratory conditions, assessing lung capacity, and optimizing ventilation strategies in clinical settings.
In addition to its clinical significance, tidal volume also has relevance in activities such as exercise physiology, where it affects an individual’s ability to supply oxygen to working muscles and remove carbon dioxide, ultimately impacting physical performance.
Importance of Tidal Volume in Respiratory Physiology
Tidal volume is of paramount importance in respiratory physiology because it plays a pivotal role in ensuring proper lung function, and facilitating the exchange of oxygen (O2) and carbon dioxide (CO2) in the body. Here’s a detailed explanation of why tidal volume is crucial in this context:
Ventilation-Perfusion Matching: Tidal volume is directly linked to the ventilation of the alveoli, the tiny air sacs in the lungs where gas exchange occurs. Adequate tidal volume ensures that fresh oxygen-rich air is consistently delivered to the alveoli during inhalation. This, in turn, promotes efficient matching of ventilation (airflow) and perfusion (blood flow) in the lungs. When ventilation and perfusion are balanced, the oxygen in the air can efficiently diffuse into the bloodstream, and carbon dioxide can be removed from the blood.
Oxygen Exchange: During inhalation, air containing oxygen is drawn into the lungs. Tidal volume determines the amount of this oxygen-rich air that reaches the alveoli. Once in the alveoli, oxygen diffuses across the thin alveolar-capillary membrane into the surrounding blood vessels, binding to hemoglobin and being transported throughout the body. Adequate tidal volume ensures a sufficient supply of oxygen to meet the body’s metabolic demands, supporting energy production and overall cellular function.
Carbon Dioxide Removal: In addition to oxygen uptake, tidal volume is critical for the removal of carbon dioxide, a waste product of cellular metabolism. When we exhale, tidal volume determines the volume of air expelled from the lungs. This air carries carbon dioxide from the bloodstream into the alveoli. From there, it is expelled during exhalation. If tidal volume is insufficient, carbon dioxide may accumulate in the bloodstream, leading to respiratory acidosis and other health issues.
Measurement Methods of Tidal Volume
Measuring tidal volume is a fundamental aspect of respiratory assessment in clinical settings, and several methods are commonly employed to accomplish this task. One of the most widely used methods is spirometry. Here, I’ll explain spirometry and touch on other respiratory tests while highlighting the ease of measuring tidal volume in a clinical setting.
Spirometry:
Spirometry is a non-invasive pulmonary function test that measures various respiratory parameters, including tidal volume. It utilizes a spirometer, a specialized device equipped with sensors to record airflow.
Procedure: During a spirometry test, the patient breathes into the spirometer through a mouthpiece or a face mask. They perform a series of maneuvers, including a normal tidal breath followed by maximal inhalation and exhalation efforts. Tidal volume is determined by measuring the volume of air displaced by normal breathing.
Ease of Measurement: Spirometry is considered the gold standard for measuring tidal volume in clinical settings due to its ease of use, accuracy, and reliability. It provides immediate results and is suitable for routine screening and monitoring of respiratory conditions.
Plethysmography:
Plethysmography, or body plethysmography, is another method used to measure tidal volume and other lung volumes. It involves placing a patient in a sealed chamber.
Procedure: The patient breathes normally within the chamber while pressure and volume changes are recorded. By comparing the initial and final volumes in the chamber, tidal volume can be determined.
Ease of Measurement: While plethysmography is highly accurate, it is less commonly used for routine measurements due to the need for specialized equipment and facilities.
Tidal Breathing Flow-Volume Loops:
This graphical method involves plotting airflow (flow) against lung volume to create flow-volume loops.
Procedure: During tidal breathing, patients breathe into a device that records their flow and volume data in real-time. The area under the loop represents tidal volume.
Ease of Measurement: Flow-volume loops are often used in research and specialized clinical assessments, but they are not as common for routine measurements as spirometry.
Respiratory Inductance Plethysmography (RIP):
RIP is a non-invasive method that measures changes in chest and abdominal wall circumferences during breathing.
Procedure: Sensors are placed around the chest and abdomen, and changes in these measurements are used to calculate tidal volume.
Ease of Measurement: RIP can be useful in certain clinical scenarios, especially when spirometry is not feasible. It is relatively easy to set up and provides continuous tidal volume monitoring.
In summary, measuring tidal volume is a routine procedure in clinical settings, and the most common method is spirometry due to its ease of use and accuracy. It allows healthcare professionals to assess lung function, diagnose respiratory conditions, monitor disease progression, and guide treatment decisions. Other methods like plethysmography, flow-volume loops, and RIP have their applications but are generally reserved for more specialized situations or research purposes.
Normal tidal volume values can vary depending on several factors, including age, sex, body size, and overall health. However, there are typical ranges for tidal volume that can serve as a general reference for adults and children. Keep in mind that these values are approximate, and individual variations are common:
Tidal Volume in Adults:
Normal Range: In healthy adults, the typical tidal volume during quiet, resting breathing is around 500 milliliters (ml) to 700 ml.
Variability: Tidal volume can vary among individuals. Larger individuals may have slightly higher tidal volumes to accommodate their greater lung capacity, while smaller individuals may have slightly lower values.
Factors Affecting Tidal Volume: Factors such as age, sex, physical fitness, and underlying lung conditions can influence tidal volume. For example, athletes or individuals with strong respiratory muscles might have larger tidal volumes, while those with lung diseases may exhibit reduced values.
Tidal Volume in Children:
Infants and Toddlers: Tidal volume in infants and toddlers is considerably smaller than in adults, typically ranging from 6 ml/kg to 8 ml/kg of body weight. It’s important to note that these values are approximate and can vary among infants based on factors like prematurity and overall health.
School-Aged Children: As children grow, their tidal volume increases. For school-aged children, tidal volume may range from 7 ml/kg to 10 ml/kg.
Adolescents: As children transition into adolescence, their tidal volume continues to increase and approaches adult values. Tidal volume in adolescents may fall within the adult range of 500 ml to 700 ml.
It’s crucial to emphasize that individual variations are significant, and the values mentioned above are approximate averages. Clinicians often consider a person’s specific characteristics, including age, sex, and health status, when interpreting tidal volume measurements. Additionally, during physical activity or exercise, tidal volume can increase to meet the body’s increased oxygen demand, and this adaptive response is also subject to individual variability.
Clinical assessment of tidal volume, especially when compared to other lung volumes and capacities, helps healthcare professionals diagnose and monitor respiratory conditions and tailor treatment plans to individual needs. Therefore, any assessment of tidal volume should be interpreted in the context of the patient’s unique characteristics and medical history.
Clinical Applications
Tidal volume is a valuable parameter in diagnosing and monitoring various respiratory conditions, including asthma, chronic obstructive pulmonary disease (COPD), and restrictive lung diseases. It plays a crucial role in assessing lung function and the overall health of the respiratory system. Here’s how tidal volume is used in clinical applications for these conditions:
Diagnosis: Tidal volume measurement is an essential component of pulmonary function tests used in diagnosing asthma. Patients with asthma often exhibit reduced tidal volumes due to increased airway resistance and bronchoconstriction during an asthma attack.
Monitoring: Tidal volume monitoring can track changes in lung function over time, helping healthcare providers assess the effectiveness of asthma medications and interventions. A decrease in tidal volume may signal worsening asthma control, while an improvement suggests a positive response to treatment.
Chronic Obstructive Pulmonary Disease (COPD):
Diagnosis: Tidal volume assessment, combined with other lung function tests like forced expiratory volume in one second (FEV1) and forced vital capacity (FVC), aids in the diagnosis of COPD. In COPD, tidal volume may be normal or increased, but the ability to exhale air is significantly impaired.
Monitoring: Regular monitoring of tidal volume is essential in managing COPD patients. It helps healthcare providers assess disease progression and the impact of therapies, such as bronchodilators and pulmonary rehabilitation. Changes in tidal volume can indicate worsening or improving lung function.
Restrictive Lung Diseases:
Diagnosis: Tidal volume measurements are vital for diagnosing restrictive lung diseases, such as pulmonary fibrosis and chest wall deformities. In these conditions, the ability of the lungs to expand and accommodate a normal tidal volume is impaired, resulting in reduced tidal volumes.
Monitoring: Tidal volume monitoring is crucial for tracking disease progression and response to treatment in patients with restrictive lung diseases. An increase in tidal volume may suggest an improvement in lung compliance, while a persistent reduction indicates ongoing restrictive pathology.
Assessing Lung Capacity:
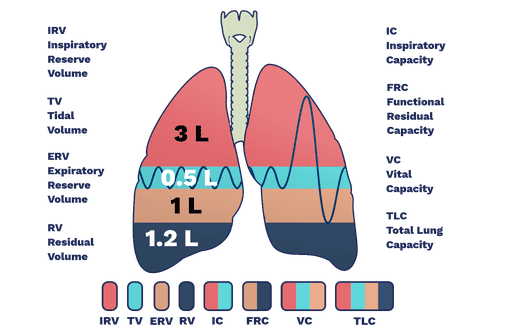
Tidal volume is a fundamental component of various lung capacity measurements, including vital capacity (VC) and inspiratory capacity (IC). These measurements provide insights into overall lung function.
VC: Vital capacity is the maximum amount of air that can be exhaled forcefully after a maximal inhalation. It includes tidal volume and additional volumes (inspiratory reserve volume and expiratory reserve volume). Changes in tidal volume can affect VC.
IC: Inspiratory capacity is the maximum volume of air that can be inhaled after a normal exhalation. Tidal volume is a key component of IC and helps assess a person’s ability to take in additional air during exertion or deep breathing.
In summary, tidal volume serves as a valuable clinical tool for diagnosing, monitoring, and managing respiratory conditions, including asthma, COPD, and restrictive lung diseases. It aids in assessing lung function, tracking disease progression, and evaluating treatment responses.
Ventilation Strategies
Understanding tidal volume is indeed crucial in optimizing mechanical ventilation, especially in intensive care units (ICUs) and during surgical procedures where patients may require respiratory support. Mechanical ventilation involves the use of ventilators to assist or control a patient’s breathing, and tidal volume plays a central role in this context. Here’s how an understanding of tidal volume is vital for these ventilation strategies:
Lung Protection and Ventilator-Induced Lung Injury (VILI) Prevention:
Tidal volume is a key factor in lung protection strategies. The use of excessively high tidal volumes during mechanical ventilation can lead to a condition called ventilator-induced lung injury (VILI), which may exacerbate existing lung conditions or cause new problems.
Low tidal volume ventilation strategies, often referred to as lung-protective ventilation, involve using smaller tidal volumes to reduce the risk of VILI. Understanding the appropriate tidal volume for a patient’s condition and needs is essential to minimize lung damage and inflammation.
Individualized Care:
Every patient’s respiratory needs vary, and their tidal volume requirements may differ based on factors like lung compliance, airway resistance, and underlying lung conditions.
Understanding a patient’s ideal tidal volume allows healthcare providers to tailor mechanical ventilation settings to meet their specific needs. This personalized approach can improve patient outcomes and reduce the risk of complications.
Surgical Ventilation:
During surgery, especially procedures that require general anesthesia, mechanical ventilation is often employed to maintain adequate oxygenation and carbon dioxide removal. Tidal volume settings are crucial in this context.
Careful control of tidal volume ensures that the patient’s oxygen and carbon dioxide levels remain within a safe and optimal range throughout the surgical procedure. This prevents hypoxia (low oxygen levels) and hypercapnia (elevated carbon dioxide levels).
Positive End-Expiratory Pressure (PEEP):
PEEP is a common component of mechanical ventilation in ICUs and during surgery. It involves maintaining a positive pressure in the airways at the end of exhalation to prevent lung collapse and improve oxygenation.
Tidal volume settings need to be coordinated with PEEP to optimize lung recruitment and prevent overdistension. Understanding the patient’s tidal volume requirements helps strike the right balance between lung recruitment and avoiding lung injury.
Weaning from Mechanical Ventilation:
As patients recover, it becomes essential to gradually reduce their reliance on mechanical ventilation. Tidal volume measurements play a role in determining when a patient is ready for weaning.
Monitoring changes in tidal volume, respiratory rate, and other parameters can help healthcare providers assess a patient’s ability to breathe independently and make informed decisions regarding the weaning process.
In conclusion, understanding tidal volume is a critical component of mechanical ventilation management in ICUs and during surgical procedures. It ensures that ventilation strategies are tailored to each patient’s unique needs, helps prevent VILI, and plays a key role in optimizing oxygenation and ventilation while minimizing the risk of complications associated with artificial ventilation.
Exercise Physiology
Tidal volume plays a significant role in exercise physiology and has a direct impact on physical performance, particularly in terms of oxygen delivery during exercise and endurance activities. Here’s an exploration of the connection between tidal volume and physical performance:
Increased Oxygen Demand:
During physical activity and exercise, the body’s oxygen demand rises significantly to support increased muscle activity and energy production. Tidal volume plays a crucial role in meeting this elevated oxygen demand.
As exercise intensity increases, individuals need to breathe more deeply and rapidly to take in more oxygen. Tidal volume is a critical component of this increased ventilation.
Enhanced Oxygen Uptake:
Tidal volume directly influences the amount of oxygen entering the lungs with each breath. A larger tidal volume allows for more oxygen to be brought into the lungs.
With a greater tidal volume, more oxygen can diffuse across the alveolar-capillary membrane into the bloodstream, leading to improved oxygen uptake. This enhances the oxygen-carrying capacity of the blood and, subsequently, the delivery of oxygen to working muscles.
Improved Oxygen Transport:
Tidal volume, when combined with an increased respiratory rate during exercise, ensures a continuous supply of oxygen to the blood. The oxygen-rich blood is then pumped by the heart to various tissues and muscles throughout the body.
Adequate tidal volume helps optimize oxygen transport, ensuring that muscles have a sufficient supply of oxygen to support aerobic energy production. This is particularly crucial for endurance activities where sustained effort is required.
Carbon Dioxide Removal:
As exercise generates carbon dioxide (CO2) as a metabolic byproduct, tidal volume also facilitates efficient CO2 removal from the body.
A well-regulated tidal volume ensures that excess CO2 is efficiently exhaled, preventing the buildup of carbon dioxide in the bloodstream. This is essential for maintaining the body’s acid-base balance and overall exercise performance.
Endurance Training and Adaptations:
Endurance training, such as long-distance running or cycling, can lead to adaptations in tidal volume and respiratory muscle strength. Athletes who engage in regular endurance training often exhibit increased tidal volumes and more efficient breathing patterns.
These adaptations allow endurance athletes to sustain higher levels of effort over prolonged periods, as they can take in more oxygen and remove CO2 more effectively, ultimately enhancing their endurance and performance.
Limitations and Constraints:
Tidal volume has its limits, and in very strenuous exercise or at high altitudes, individuals may reach a point where their tidal volume can no longer meet the oxygen demand. In such cases, other factors like the respiratory rate and the efficiency of oxygen utilization by muscles become crucial.
In summary, tidal volume is a critical factor in exercise physiology, impacting the delivery of oxygen to working muscles and the removal of metabolic waste products like carbon dioxide. A well-balanced tidal volume, in conjunction with other respiratory parameters, ensures efficient oxygen transport and contributes to optimal physical performance, especially during endurance activities where sustained effort is required.
Factors Affecting Tidal Volume
Tidal volume, the volume of air inspired or expired during a single breath cycle at rest, can be influenced by various factors. These factors affect the body’s respiratory response and how much air is moved in and out of the lungs. Here are some key factors that can influence tidal volume:
Exercise Intensity:
Exercise Demand: Tidal volume increases with exercise intensity. When physical activity becomes more strenuous, the body requires more oxygen to meet the increased metabolic demands of muscles.
Ventilatory Response: To supply more oxygen and remove additional carbon dioxide produced during exercise, the body responds by increasing both tidal volume and respiratory rate. This allows for more air exchange in the lungs.
Altitude:
Lower Oxygen Levels: At higher altitudes, the partial pressure of oxygen in the air is lower, which means less oxygen is available for inhalation.
Increased Tidal Volume: To compensate for the reduced oxygen pressure, individuals at higher altitudes typically breathe more deeply, leading to an increase in tidal volume and respiratory rate. This helps maintain adequate oxygen intake.
Respiratory Muscle Strength:
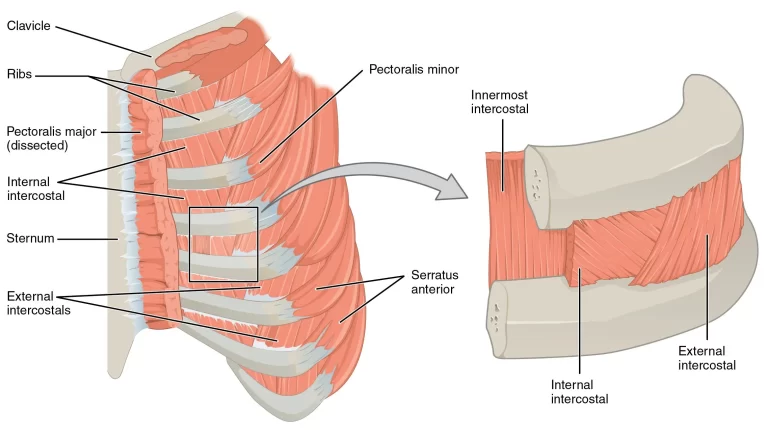
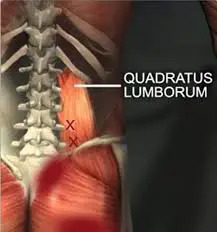
Respiratory Muscle Function: The strength and endurance of the respiratory muscles, including the diaphragm and intercostal muscles, play a crucial role in determining tidal volume.
Weakness or Fatigue: Weak or fatigued respiratory muscles may limit a person’s ability to generate sufficient tidal volume. This can occur in conditions such as respiratory muscle weakness or neuromuscular diseases.
Lung Compliance and Elasticity:
Lung Properties: The compliance and elasticity of the lungs affect how easily they can expand and contract.
Reduced Compliance: Conditions that reduce lung compliance, such as pulmonary fibrosis or lung stiffness, can limit the ability to achieve a normal tidal volume, leading to reduced lung function.
Body Size and Gender:
Body Size: Larger individuals typically have larger lung volumes, including tidal volume, to accommodate their greater lung capacity.
Gender Differences: On average, males tend to have slightly larger lung volumes compared to females, which can also affect tidal volume.
Age:
Effects of Aging: Tidal volume may decrease with age due to changes in lung elasticity and muscle strength. This can result in a reduced ability to generate the same tidal volume as in younger individuals.
Respiratory Conditions:
Obstructive Lung Diseases: Conditions like chronic obstructive pulmonary disease (COPD) can limit the ability to achieve a normal tidal volume due to airway obstruction and increased airway resistance.
Restrictive Lung Diseases: Restrictive lung diseases, such as pulmonary fibrosis, can restrict lung expansion, reducing tidal volume.
Psychological Factors:
Anxiety and Stress: Emotional states like anxiety and stress can influence tidal volume. In response to emotional distress, individuals may exhibit shallow breathing and reduced tidal volume.
Position and Posture:
Body Position: Tidal volume can be affected by body position. For instance, lying flat or in a prone position may alter tidal volume compared to an upright posture.
In summary, tidal volume is influenced by a range of factors, including exercise intensity, altitude, respiratory muscle strength, lung properties, body size, gender, age, respiratory conditions, psychological factors, and body position. Understanding how these factors interact and affect tidal volume is essential in clinical assessments, especially when evaluating respiratory health and performance in various contexts.
Respiratory Disorders that Affect the Tidal Volume
Tidal volume, the volume of air inhaled or exhaled during a normal breath, can be significantly affected in various respiratory disorders, including pneumonia, bronchitis, and pulmonary fibrosis. These conditions can lead to alterations in tidal volume, which, in turn, impact patients’ well-being in different ways. Here’s an overview of these effects:
Pneumonia:
Effect on Tidal Volume: In pneumonia, the air sacs (alveoli) in the lungs become filled with pus and other inflammatory substances. This reduces the available space for air exchange and, consequently, the ability to achieve a normal tidal volume.
Impact on Well-being: Reduced tidal volume in pneumonia can result in shallow and rapid breathing as patients struggle to maintain adequate oxygenation. This leads to increased respiratory effort and a feeling of breathlessness. Pneumonia can also cause chest pain and discomfort during breathing.
Bronchitis:
Effect on Tidal Volume: Acute bronchitis is characterized by inflammation of the bronchial tubes, which can lead to increased mucus production and narrowing of the airways. This constriction can reduce the ability to achieve a normal tidal volume.
Impact on Well-being: Reduced tidal volume in bronchitis can result in coughing, wheezing, and shortness of breath. Patients often experience difficulty in clearing mucus from their airways, further compromising their ability to breathe comfortably.
Pulmonary Fibrosis:
Effect on Tidal Volume: Pulmonary fibrosis is a progressive lung disease characterized by the scarring (fibrosis) of lung tissue. This scarring reduces lung compliance, making it difficult for the lungs to expand fully during inhalation, thereby limiting tidal volume.
Impact on Well-being: Decreased tidal volume in pulmonary fibrosis can lead to a persistent feeling of breathlessness, even at rest. Patients may have to work harder to breathe, resulting in fatigue and reduced exercise tolerance. Over time, this condition can severely impact a person’s quality of life.
Chronic Obstructive Pulmonary Disease (COPD):
Effect on Tidal Volume: COPD encompasses conditions like chronic bronchitis and emphysema, which lead to airway obstruction and reduced lung function. Tidal volume can be affected due to increased airway resistance and reduced lung compliance.
Impact on Well-being: Reduced tidal volume in COPD contributes to chronic shortness of breath, especially during physical activity. Patients may experience frequent exacerbations, which further impair tidal volume and overall lung function. COPD can significantly limit daily activities and decrease overall well-being.
In all of these respiratory disorders, the impaired ability to achieve a normal tidal volume results in inadequate oxygen exchange and increased work of breathing. This leads to symptoms such as shortness of breath, fatigue, and decreased physical endurance. Additionally, these conditions can have a profound impact on a patient’s overall quality of life, affecting their ability to perform daily activities and leading to emotional distress.
Effective management and treatment of these respiratory disorders often involve strategies to improve tidal volume and alleviate symptoms. These may include medications, pulmonary rehabilitation, oxygen therapy, and lifestyle modifications, all aimed at optimizing lung function and enhancing patients’ well-being.
Pediatric Considerations
Tidal volume can indeed vary significantly in children and infants compared to adults, and healthcare providers pay special attention to this when caring for pediatric patients. Understanding these variations is essential for assessing respiratory health and providing appropriate medical care to children of different ages. Here’s why tidal volume considerations are crucial in pediatric care:
Age-Dependent Variations:
Pediatric patients encompass a wide age range, from neonates to adolescents. Tidal volume varies significantly among these age groups.
Neonates and infants typically have smaller lung volumes and, consequently, smaller tidal volumes compared to older children and adults. As children grow, their lung capacity and tidal volume increase.
Developmental Stages:
Tidal volume is influenced by the stage of lung development in pediatric patients. Premature infants, for example, may have limited lung maturity and reduced tidal volumes.
Healthcare providers closely monitor respiratory parameters, including tidal volume, in premature infants to assess lung function and the need for interventions like respiratory support.
Clinical Assessment:
Tidal volume measurements are a routine part of respiratory assessments in pediatric care. Healthcare providers use various techniques, such as spirometry, to measure tidal volume and assess lung function.
These assessments help diagnose and monitor respiratory conditions in children, such as asthma, bronchiolitis, and congenital lung disorders. Deviations from expected tidal volume values can indicate potential problems.
Treatment and Intervention:
Knowledge of age-appropriate tidal volume values informs treatment decisions in pediatric care. For example, mechanical ventilation settings are carefully adjusted to match a child’s tidal volume needs and respiratory patterns.
In cases of respiratory distress or respiratory diseases, healthcare providers may provide therapies tailored to the child’s unique physiology to optimize tidal volume and oxygenation.
Preventive Care:
Pediatric care also emphasizes preventive measures to promote respiratory health. Providers may recommend vaccination to prevent respiratory infections, which can affect tidal volume and overall lung function in children.
Parent and caregiver education is essential to identify signs of respiratory distress in infants and young children, allowing for early intervention.
In summary, tidal volume is a critical parameter in pediatric care, as it varies significantly with age and developmental stage in children and infants.
Future Trends
Emerging technologies and research trends related to tidal volume measurement and its clinical applications are poised to advance respiratory assessment and patient care. Here are a few notable developments:
Advanced Monitoring Devices: Innovative wearable devices and portable spirometers are being developed for continuous, real-time monitoring of tidal volume and other respiratory parameters. These technologies enable remote patient monitoring, enhancing the management of chronic respiratory conditions and early detection of changes in lung function.
Artificial Intelligence (AI): AI and machine learning are being harnessed to analyze complex respiratory data. AI algorithms can help predict exacerbations of respiratory diseases, optimize ventilation settings, and provide personalized treatment recommendations based on tidal volume measurements and other clinical data.
Telemedicine and Telehealth: Telemedicine platforms are integrating respiratory assessments, including tidal volume measurement, into virtual healthcare encounters. This facilitates remote consultations, reduces the need for in-person visits, and enhances access to respiratory care, especially in underserved areas.
Personalized Medicine: Research into genetics and genomics is uncovering how genetic variations influence respiratory function and responses to treatment. Tidal volume measurements, combined with genetic data, may guide personalized treatment plans for respiratory conditions.
3D Printing and Customized Ventilation: 3D printing technology is enabling the creation of customized respiratory devices, including patient-specific ventilator components. This has the potential to improve ventilation strategies and optimize tidal volume delivery for individual patients.
Ventilation Strategies in Critical Care: Research into mechanical ventilation strategies is ongoing, with a focus on minimizing ventilator-induced lung injury while optimizing tidal volume. Lung-protective ventilation approaches continue to evolve, emphasizing patient-specific approaches.
Biofeedback and Respiratory Rehabilitation: Biofeedback systems are being explored for respiratory rehabilitation. These systems use real-time tidal volume data to guide patients in breathing exercises and help improve lung function.
Point-of-Care Testing: Advances in point-of-care testing devices are making it easier to measure tidal volume and other lung parameters quickly and accurately, facilitating faster clinical assessments and decision-making.
These emerging trends and technologies hold the potential to enhance the precision and efficiency of tidal volume measurements in clinical settings, leading to improved respiratory care and better outcomes for patients with various respiratory conditions. As research in respiratory physiology and technology continues to progress, the field of respiratory medicine is likely to witness exciting developments in the coming years.
Issues of Concern
Respiratory Rate Regulation: Tidal volume, in conjunction with respiratory rate, determines minute ventilation (the total volume of air moved into and out of the lungs per minute). The body can adjust both tidal volume and respiratory rate to maintain an appropriate level of oxygen and carbon dioxide in the blood. This regulatory mechanism ensures that oxygen supply matches metabolic demand and that excess carbon dioxide is effectively eliminated.
Adaptation to Exercise: During physical activity or exercise, the body’s oxygen demand increases. Tidal volume can increase to meet this demand, allowing for enhanced oxygen uptake and improved removal of carbon dioxide. This adaptive response is crucial for athletes and individuals engaged in strenuous activities.
When it comes to configuring the ventilator in critically ill patients, tidal volume is crucial. Delivering a tidal volume that is both large enough to sustain proper breathing and small enough to prevent lung trauma is the objective. Tidal volumes of at least 10 mL/kg of the ideal body weight were formerly required for mechanical ventilation. Reducing hypoxemia, avoiding airway closure, and boosting functional residual capacity were the goals.
However, because of the repeated opening of collapsed alveoli and alveolar overdistension, ventilation with enormous tidal volumes results in volutrauma. As a result, a chain of events known as an inflammatory cascade is started, which is characterized by pulmonary edoema, altered surfactant, increased lung permeability, and lung-damaging cytokines. When Webb and Tierney showed that rats developed pulmonary edoema after being exposed to high inflation pressures, it wasn’t until 1974 that they first used the term “volutrauma” to characterize this event.
Ventilating with large tidal volumes in healthy lungs can result in lung harm during mechanical ventilation, as can ventilating with lower tidal volumes in injured lungs.
Large tidal volumes of ventilation may also result in barotrauma, a condition marked by alveolar rupture and subsequent air buildup in the mediastinum or pleural cavity. Monitoring plateau pressure in patients who are mechanically ventilated is an accurate technique for assessing the likelihood of barotrauma. When mechanical ventilation is used, the tiny airways and alveoli are subjected to plateau pressure.
Tidal volume and compliance are the major determinants. The risk of barotrauma increases as plateau pressure rises and compliance falls. Therefore, a rise in plateau pressure requires a reduction in tidal volume in order to lessen the chance of alveolar rupture. Today’s standard practice is to use tidal volumes of 6 mL/kg of anticipated body weight due to ongoing research on lung-protective mechanical ventilation.
Organ Systems Involved
Delivering a tidal volume capable of ensuring adequate ventilation is the responsibility of the lungs. However, accurate tidal volume production requires precise brain-muscle coordination between the respiratory center and the breathing muscles. The respiratory pacemaker in the brainstem regulates both the depth and rate of breathing.
The brainstem receives information from central and peripheral chemoreceptors to adjust the pacemaker’s firing rate and pattern in response to variations in blood oxygen and carbon dioxide levels. Tidal volume and respiratory rate are modified in response by the diaphragm and other inspiratory muscles. The objective is to keep the blood’s levels of carbon dioxide and oxygen at a healthy level. For instance, oxygen consumption rises and carbon dioxide builds up during exercise. As a result, to accommodate the growing demand, respiratory rate and tidal volume increase.
Conclusion
In conclusion, tidal volume is a fundamental respiratory parameter with far-reaching implications in both clinical and physiological contexts. Its importance in respiratory physiology cannot be overstated, as it plays a pivotal role in oxygen exchange, carbon dioxide removal, and maintaining acid-base balance. Tidal volume measurements are crucial for diagnosing, monitoring, and managing a range of respiratory conditions, from asthma and COPD to restrictive lung diseases.
In intensive care units and surgical settings, an understanding of tidal volume is essential for optimizing mechanical ventilation strategies, protecting lung health, and ensuring patient safety. Tidal volume’s adaptability during exercise and endurance activities is critical for meeting the increased oxygen demand of the body during physical exertion.
Moreover, tidal volume is not a one-size-fits-all parameter; it varies based on factors such as age, sex, body size, and health status. This underscores the need for individualized care and tailored respiratory assessments.
In pediatrics, the significance of tidal volume takes on additional importance, given the age-dependent variations in lung capacity and development. Healthcare providers pay special attention to tidal volume in pediatric care to ensure accurate assessments and appropriate interventions.
Looking ahead, emerging technologies, such as wearable devices, AI-driven analysis, and telehealth integration, are poised to revolutionize tidal volume measurement and its clinical applications. These innovations hold the promise of advancing respiratory care, enhancing patient outcomes, and promoting personalized medicine.
In a world where respiratory health is increasingly important, a comprehensive understanding of tidal volume remains central to improving the lives of individuals affected by respiratory conditions and optimizing the respiratory care they receive.