Home Treatment For Trigeminal Neuralgia
Table of Contents
What is a Trigeminal Neuralgia?
Trigeminal neuralgia is a chronic pain condition affecting the trigeminal nerve, which is responsible for transmitting sensations from the face to the brain. Characterized by sudden, severe, and stabbing facial pain, trigeminal neuralgia can significantly impact a person’s quality of life.
While medical intervention is often necessary, there are also home treatment approaches that individuals may consider to alleviate symptoms and manage the condition. These home treatments typically focus on lifestyle modifications, stress management, and complementary therapies to help reduce pain and improve overall well-being.
Typically, it occurs in brief, erratic bursts that range in duration from a few seconds to around two minutes. The attacks abruptly end when they begin.
Trigeminal neuralgia typically only affects one side of the face, with the lower face experiencing the most discomfort. Rarely, though generally not simultaneously, the pain can radiate to both sides of the face.
Individuals suffering from the ailment could frequently have pain episodes that last for days, weeks, or even months. Attacks can occur hundreds of times a day in extreme circumstances.
The sharp episodes may occasionally be followed by a more persistent aching, throbbing, or burning sensation in certain persons.
Trigeminal neuralgia can make daily living extremely challenging. It can significantly lower someone’s quality of life and lead to issues including sadness, loneliness, and weight loss.
Anatomy of Trigeminal Nerve
One group of cranial nerves in the head is the trigeminal nerve. This nerve is in charge of giving the face its sensibility. The left side of the head is served by one trigeminal nerve and the right by the other. There are three separate branches on each of these nerves. “Trigeminal” originates from the Latin words “tria,” signifying three, and “geminus,” signifying twin. The trigeminal nerve, which controls sensations throughout the face, splits into three smaller branches after leaving the brain and moving through the skull:
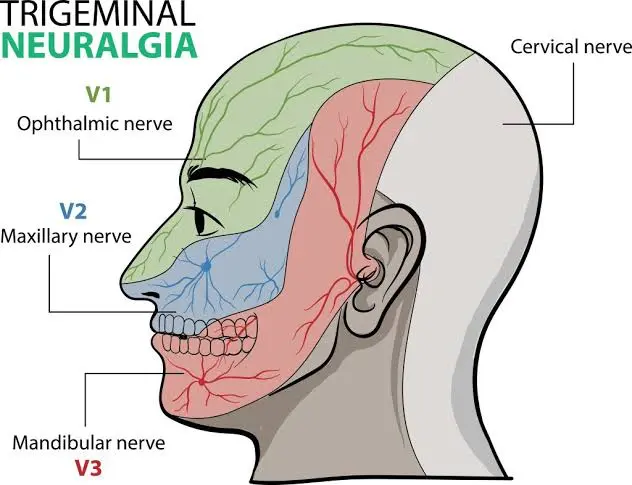
Ophthalmic Nerve (V1): The first branch regulates feeling in the forehead, upper eyelid, and eyes of an individual.
The second branch of the maxillary nerve (V2) regulates feeling in the nose, upper lip, cheek, lower eyelid, and upper side gum.
Mandibular Nerve (V3): The jaw, lower lip, lower gum, and some chewing muscles are all sensed by this third branch of the nerve.
Epidemiology
An estimated 150,000 individuals receive a trigeminal neuralgia (TN) diagnosis each year. Although the illness can strike anyone at any age, those over 50 are most likely to experience it. women experience TN twice as frequently as men do. There is a connection between TN and multiple sclerosis (MS).
Causes of Trigeminal Neuralgia
The trigeminal nerve is not functioning properly in trigeminal neuralgia, commonly known as tic douloureux. Usually, the issue arises from contact between the trigeminal nerve at the base of your brain and a regular blood vessel, in this case, an artery or vein. The nerve is compressed by this contact, which results in nerve dysfunction.
There are numerous other possible causes of trigeminal neuralgia in addition to the more frequent one of compression by a blood vessel. Some might have anything to do with MS or another condition that damages the myelin sheath that covers some nerves. A tumour compressing the trigeminal nerve can potentially result in trigeminal neuralgia.
Trigeminal neuralgia can occur in certain individuals as a result of brain lesions or other anomalies. Trigeminal neuralgia may also result from stroke, face trauma, or surgical damage in other situations.
Pathophysiology
The actual cause of trigeminal neuralgia (TN) is still unknown, hence it could have a central, peripheral, or mixed cause. Due to its primary sensory role, the trigeminal nerve (cranial nerve V) has the potential to generate pain. Although most researchers concur that vascular compression—usually venous or arterial looping at the trigeminal nerve entry into the pons—is essential to the pathophysiology of the idiopathic variation, there is typically no anatomical lesion visible (85% of cases). The cause is classified as classic trigeminal neuralgia after the default classification of idiopathic pain.
The key indicator of damage to the tiny unmyelinated and sparsely myelinated primary afferent fibres that provide nociception is neuropathic pain. Changes are made to the pain mechanisms themselves. The nerve’s root entry zone (REZ) is frequently the site of micro anatomic small and big fibre damage, or demyelination, which causes ephaptic transmission—a phenomenon in which action potentials hop from one fibre to another. One factor is the absence of inhibitory inputs from big myelinated nerve fibres. A re-entry process also results in an increase in sensory inputs. For example, the possibility that an attack could be triggered by vibration is a clinical correlate. Features, like as the refractory period and the latency between stimulation and pain, also point to the possibility of another central mechanism.
Triggers
Factors that trigger neuralgia include:
- Cutting
- Putting my hand on your face
- Meals and Drinks
- Using a toothbrush
- Speaking
- Applying cosmetics
- Airflow blowing gently across your face
- Grinning
- Cleansing your visage
- Headache conditions include cluster and migraine headaches
- Toothache
- Abnormalities of the temporomandibular joint
- Other nerve pains
- Renal Sinusitis
Risk Factors
The following have been found to be significant risk factors for TN,
- Growing older Stroke
- Blood pressure in females
- The disease Charcot-Marie-Tooth
- Tumours close to the trigeminal nerve
Types of Trigeminal Neuralgia
Two primary categories of TN exist:
Type 1
This is the standard or “classic” manifestation of the illness. Extreme, sporadic, abrupt burning or shock-like facial discomfort is the result. Each bout of discomfort can last anywhere from a few seconds to two minutes. These episodes may happen in bursts of up to two hours, often rather close together.
Pain flare-ups that are severe can be brought on by vibration or touch with the cheek (during face cleaning, shaving, or applying cosmetics), brushing your teeth, eating, drinking, talking, or being in the wind. Your face may only be slightly affected by the pain, or it may spread. Rarely do painful episodes happen while you’re asleep. Because of how bad the agony was, several people may shy away from social interactions or everyday activities out of concern for a potential attack.
Type 2
This “atypical” form of the illness is typified by a persistent scorching, stabbing, or agonizing pain. Usually, this discomfort is not as bad as Type 1.
You may occasionally have both types of trigeminal neuralgia simultaneously. The severity of pain can have disastrous effects on one’s body and mind. TN attacks usually pause for a while before resuming. The illness may be progressive in certain instances, which means that the attacks may worsen with time and that there may be fewer and shorter intervals without pain before they return.
The pain-free intervals gradually vanish with progressive TN, and the effectiveness of painkillers diminishes.
Symptom of Trigeminal Neuralgia
Symptoms of trigeminal neuralgia can include one or more of the following patterns:
periods of intense, stabbing, or shooting pain that could be compared to an electric shock
episodes of discomfort that happen on their own or that are brought on by actions like stroking the face, chewing, speaking, or brushing teeth
Pain episodes that range in duration from a few seconds to many minutes
Pain that results from spasms in the face
Attacks that endure for days, weeks, months, or longer in succession; some people go for extended periods of time without experiencing any discomfort.
Trigeminal nerve-supplied regions of pain, such as the cheek, jaw, teeth, gums, lips, and, less frequently, the eye and forehead
One side of the face experiencing pain at a time
Pain that is localized or distributed within a larger area
Rarely, pain happening while you’re sleeping at night
Attacks that increase in frequency and severity with time
Trigeminal neuralgia shares similarities with a number of other pain conditions. Trigeminal neuropathic pain is the most prevalent mimic of TN (TNP). Trigeminal nerve damage or injury is the cause of TNP. Most people who have TNP pain report it as dull, searing, and continuous. Sharp pain episodes are also possible; these are typically occur by touch.
Other mimics consist of:
Ernest syndrome (temporal tendinitis) stylomandibular ligament injury
The occipital nerve
Migraines and cluster headaches
Massive cell arthritis
Toothache
Herpes-related neuralgia
Neuralgia of the gloss pharynx
Infection of the sinus
Infected ears
Syndrome of the temporomandibular joint (TMJ)
Complications
The main issue with trigeminal neuralgia is the toxicity and side effects that come with using anticonvulsants over an extended period of time. Another issue is that these medications’ ability to manage neuralgia is diminishing over a period of years, making the addition of a second anticonvulsant necessary and perhaps increasing the risk of drug-related side effects.
Common mistakes to avoid are misdiagnosing bone marrow aplasia as an idiosyncratic side effect of carbamazepine and failing to detect a brainstem tumour.
Invasive procedures require standard care because they are the most likely to result in claims. Long-term problems are possible with percutaneous neurosurgery operations and microvascular decompression treatments. There are perioperative dangers as well. Consult Surgery for Trigeminal Neuralgia. Furthermore, some patients experience relief for only a year or two following the procedure, at which point they must consider having another operation. Others may have to wait weeks or months for relief.
Some individuals experience irreversible loss of feeling in parts of their mouths or faces. Patients may experience corneal anaesthesia and/or jaw weakness occasionally. Nerve differentiation can produce trophic disruptions, which can lead to corneal ulcers.
Reactivation of a herpes simplex infection is common following any invasive treatment.
Anaesthesia dolorosa, a persistent facial dysesthesia, is the worst complication and maybe even more incapacitating than the initial trigeminal neuralgia. Occasionally, surgery and other treatments can be the cause of this dysesthesia.
Diagnosis
Since there are no particular diagnostic tests for TN and its symptoms are quite similar to those of other conditions causing face pain, TN can be exceedingly challenging to diagnose. Consequently, if you have unexpected, acute pain in the area of your eyes, lips, nose, jaw, forehead, or scalp, you should get medical attention right away, especially if you haven’t had any recent dental or face surgery. The first step for the patient should be to discuss the issue with their primary care physician. Later on, they might recommend the patient to a specialist.
If MS or a tumour is damaging the trigeminal nerve, it can be determined with magnetic resonance imaging (MRI). A high-resolution, thin-slice, or three-dimensional magnetic resonance imaging (MRI) can detect blood vessel compression. More advanced scanning methods can indicate whether or not a vascular lesion is pressing on the nerve, as well as how much is compressed. On these scans, vein compression is more difficult to detect. Tests are useful in eliminating potential causes of facial abnormalities.
The patient’s statement of their symptoms, a thorough patient history, and a clinical evaluation are typically used to diagnose TN. Physicians must primarily rely on patient history and symptoms as there are no particular diagnostic tests for TN. Doctors diagnose patients based on the type of pain (abrupt, sudden, and shock-like), the source of the pain, and the objects that cause it. In order to determine the exact location of the pain, the doctor may also perform physical and neurological examinations during which they will touch and examine various portions of your face.
International Headache Society guidelines
A – Paroxysmal episodes of pain that impact one or more trigeminal nerve divisions and meet certain criteria, lasting anywhere from a fraction of a second to two minutes C and B
B-At least one of the following traits describes pain: (1) strong, piercing, superficial, or stabbing; or (2) brought on by trigger circumstances or trigger regions
C – Targets the specific patient with stereotypes
D – No neurologic impairment that is clinically apparent
E: Not connected to any other illness
Physicians may ask you to try a brief course of antiseizure medication if they suspect you have TN1. If the drug is effective, it supports the TN1 diagnosis.
Although the diagnosis of TN2 is more complicated and challenging, physicians may advise you to try taking tricyclic antidepressants, such as amitriptyline and nortriptyline, at lower doses to see if it helps. If this is the case, TN2 diagnosis is supported by a favorable response to treatment.
Treatment of Trigeminal Neuralgia
Patient`s Educations
A description of the disorder’s natural history is beneficial to patients, as it helps them to understand that long-term anticonvulsant treatment may not be necessary until the syndrome spontaneously remits for months or even years. Because of this, some people may decide to reduce their medicine after the initial episode passes; as a result, it is important to inform them of the significance of following their prescribed course of action.
Additionally, especially in older patients, individuals need to be informed about the possible side effects of anticonvulsant drugs, such as drowsiness and ataxia, which can make operating machinery or driving dangerous. These medications may also be harmful to the hematopoietic system and liver. Record the conversation regarding these possible dangers that you had with the patient.
There isn’t a particular preventative treatment. Since patients may experience premonitory atypical pain for months, early and more effective treatment may result from proper identification of this pre-trigeminal neuralgia syndrome.
Maneuvers that cause pain should be avoided by patients. After the diagnosis is made, tell them that even if the discomfort travels to the gums, tooth extractions do not provide relief.
Patients who want to have a procedure should report any changed facial sensation, especially following one, and be informed of any possible side effects. They ought to be made aware of the possibility of dolorosa anaesthesia.
Nonsurgical Interventions
Pain can be effectively managed in a number of ways, including with a range of drugs. Typically, low doses of medications are started and then progressively increased based on how the patient responds to the medication.
The anticonvulsant medication and other
Carbamazepine is the most often prescribed by physicians to treat TN. Most people’s pain is controlled by carbamazepine during the early stages of the condition. If this drug is not helping the patient, the doctor may question if TN is actually present. Nonetheless, carbamazepine’s efficacy diminishes with time. Nausea, sleepiness, double vision, and dizziness are possible adverse effects.
TN can be treated with the anticonvulsant medication gabapentin, which is primarily used to treat migraines and epilepsy. This medication has very mild side effects, such as sleepiness and/or dizziness, which go away on their own.
More recently, the first line of treatment has included the use of a more contemporary medicine called oxycarbazepine. It shares a structural similarity with carbamazepine and might be chosen due to its generally lower occurrence of side effects. Double vision and vertigo are possible adverse effects.
Clonazepam, sodium valporate, lamotrigine, phenytoin, valproic acid, baclofen, amitriptyline, , pregabalin, and opioids are among the other drugs.
Beyond side effects, these drugs have disadvantages. Higher doses can have more noticeable adverse effects, and some people may require rather high doses to relieve their pain. Over time, anticonvulsant medications may become less effective. Adverse medication reactions may occur if a patient requires a second anticonvulsant or a larger dose to relieve their discomfort. For some patients, especially those with a history of bone marrow suppression and kidney and liver toxicity, several of these medications can have hazardous side effects. To make sure these patients are safe, their blood pressure has to be checked.
Operative procedure
In cases where medicine has not been successful in managing TN, a number of surgical techniques may assist in managing pain.
There are 2 types of surgical treatment:
Either open brain surgery or Lesioning techniques. When it is determined through brain imaging, such as a specialized MRI, that a patient has pressure on the trigeminal nerve due to a neighboring blood artery, open surgery is typically carried out. It is believed that this operation will remove the underlying issue that is producing the TN. On the other hand, lesioning techniques include intentional damage to the trigeminal nerve with the goal of stopping the nerve from causing facial pain. Lesioning may have more transient symptoms, including facial numbness in certain cases.
1. Open Procedure
The trigeminal nerve root is microsurgically exposed during microvascular decompression, and a blood artery may be gently moving the blood artery away from the site of compression and squeezing the nerve. By allowing the trigeminal nerve to heal and revert to a more typical, pain-free state, decompression may lessen sensitivity. Due to the need for a craniotomy to open the skull, this procedure is usually the most invasive even if it is also the most effective. There is a slight chance of double vision, stroke, facial paralysis, diminished hearing, and even death.
2. Lesioning Methodologies
TN is treated with percutaneous radiofrequency rhizotomy by electrocoagulation (heat). Eliminating the portion of the nerve responsible for the pain and blocking the brain’s pain signal, can reduce nerve discomfort. A hollow needle is inserted by the surgeon into the trigeminal nerve through the cheek. A current that heats up and travels through an electrode kills some of the nerve fibres.
Percutaneous balloon compression
In order to apply percutaneous balloon compression, a needle is inserted into the cheek and into the trigeminal nerve. Using a catheter, the neurosurgeon inserts a balloon into the trigeminal nerve. The balloon is inflated at the site of pain-producing fibres. After damaging the pain-producing fibres by compressing the nerve, the balloon is removed.
Percutaneous glycerol rhizotomy
Glycerol is injected with a needle into the location where the nerve splits into its three main branches in order to perform a percutaneous glycerol rhizotomy. The idea is to specifically harm the nerve to obstruct the brain’s ability to receive pain messages.
Through techniques like Cyberknife, Gamma Knife, and Linear Accelerator (LINAC), stereotactic radiosurgery provides a single, highly concentrated dose of tiny, exact targets located at the root of the trigeminal nerve. Numerous dangers and consequences associated with open surgery and other therapies are circumvented by this non-invasive approach. The gradual creation of a lesion in the nerve due to radiation exposure over time prevents pain signals from reaching the brain.
In general, one should always carefully consider the hazards associated with surgery or Lesioning techniques in relation to their advantages. While many TN patients report significant pain alleviation following operations, not everyone will benefit from them.
Brain-Stimulation
In order to provide electrical stimulation to the area of the brain responsible for facial sensation, patients with TNP may benefit from another surgical procedure in which one or more electrodes are positioned in the soft tissue close to the nerves, beneath the skull on the surface of the brain, and occasionally deeper into the brain. The leads for peripheral nerve stimulation are positioned beneath the skin on trigeminal nerve branches. The region that innervates the face is stimulated using motor cortex stimulation (MCS). Deep brain stimulation (DBS) may activate brain areas that influence facial sensory pathways.
Supplementary therapies
Certain individuals treat their trigeminal neuralgia with complementary therapies, typically in addition to medication. The efficacy of these therapies varies. Treatments for TN that are complementary include:
- Low-stress workouts
- Yoga poses
- Imaginative visuals
- Use of aromas
- Introspection Acupuncture
- Therapy with chiropractic adjustments for the upper cervical spine
- Feedback from within
- Vitamin supplementation
- Nutritional treatment
- Botulinum toxin injections to stop sensory nerve activity
Physiotherapy management
Through the application of various approaches, physiotherapy improves, maintains, and restores an individual’s physical, psychological, and social welfare. The patient’s needs and goals are the main emphasis of TN’s physiotherapy treatment.
Your symptoms’ course of treatment will change according to the neuralgia’s cause, location, and severity. For instance, tight blood sugar management will assist in reducing symptoms if you are diagnosed with diabetes. You could require surgery to remove a tumour if it is pressing on your nerves. In order to alleviate the symptoms of neuralgia, you will require medicine to treat the infection if you have shingles.
Relieving pain is the main goal of the treatment. Originally developed to treat epilepsy, anticonvulsant medications lessen nerve discomfort and excitability in the nervous system. The symptoms of can also be relieved by nerve blocks, surgical treatments, or injections of painkillers.
Goal
The goals of physiotherapy treatment for neuralgia are to lessen symptoms while enhancing the general quality of life and muscle strength. Following a thorough evaluation by a neurological physiotherapy specialist, your care could consist of:
- mobilisation of muscles
- Stretches for soft tissues
- Exercises to strengthen muscles
- Proprioceptive and sensory stimulation
- Pain control
- facilitation of daily living activities.
Benefits
Neuralgia sufferers greatly benefit from the care provided by a neurological physiotherapist. The benefits consist of:
- increased muscular strength
- Resuming regular daily activities
- reduces in pain
- Keep your muscles long.
- Preserve your joints’ range of motion.
- Reduced alterations in perception
- Discover how to control your pain.
- Acquire particular exercises to perform at work or home.
Management
TENS, or electrical stimulation
It is the more popular and successful method.
For four weeks, five days a week, patients received continuous transcutaneous electrical nerve stimulation (TENS) at 250 Hz with a 120 u pulse across the afflicted nerve for 20 minutes. One electrode was positioned directly in front of the ear, and the other at the end of the corresponding nerve. When necessary, however, the location was adjusted based on effectiveness and pain referral.
Therapy that Interferential (IFT)
Ultrasound ( US )
Additionally, the management of ultrasound physiotherapy will use the following techniques to lessen discomfort and enhance the ability to do activities of daily living
Hot pack and workouts for the isometric neck
In order to lessen muscle spasms, the trapezius and neck muscles were treated to a heated, wet pack for ten minutes. Additionally, each side received isometric neck exercises and five repetitions of pain-free neck range-of-motion exercises (neck flexion, extension, and side flexion).
Deep breathing exercises and other relaxation techniques
For ten minutes, which included deep breathing exercises. Techniques for distraction are also included. Instead of sitting and thinking about their discomfort situations, patients were advised to participate in the activities that they enjoy. It was requested that they practice these exercises at home.
Cardiovascular workouts
It is used to enhance fitness and well-being
Practical Activities for issues related to ADLs
Tips to reduce hypersensitivity
Patients were instructed to cover the afflicted side of their face with a cotton pad or a soft cloth for 15 minutes each day in order to lessen their hypersensitivity. This may have the effect of reducing the nervous system’s exposure to continual afferent input.
Tips on how to avoid washing and drinking with cold water and chew on the non-disease side.
In addition, physiotherapy can educate, counsel, and inspire patients in many ways that are relevant to the management of TN. Even though physiotherapy is a successful treatment for TN, the general public needs to be made aware of its importance.
Acupuncture and Additional Therapies in Integrative Medicine
In order to relieve pain, acupuncture inserts tiny needles along the “trigger points.” Acupuncture has been reported by some trigeminal neuralgia sufferers to lessen the severity and/or frequency of flare-ups.
For those seeking additional treatment following surgery or more natural approaches to treating trigeminal neuralgia, there are alternative options such as meditation, wellness centers, and lifestyle modification programmes.
Prevention
Trigeminal neuralgia cannot be prevented, regrettably. However, by avoiding specific behaviors that result in extreme, excruciating pain, you can prevent uncomfortable episodes. Furthermore, there is no evidence to support the theory that stress causes trigeminal neuralgia.
Differential diagnosis
- headache conditions include cluster and migraine headaches
- toothache
- abnormalities of the temporomandibular joint
- Other nerve pains
- Sinusitis infection
How to care for loved ones with trigeminal neuralgia
The pain and anxiety associated with trigeminal neuralgia, while not life-threatening, can significantly impair the quality of life for both the affected individual and those in their vicinity. The first steps to providing care for a loved one with trigeminal neuralgia are to acknowledge the extent of the pain the individual is experiencing and to be understanding. Other actions could be:
Assisting your loved one in taking their prescriptions as prescribed and keeping you informed about the treatment’s progress.
Promoting medical appointments and looking at alternate forms of care when prescription drugs run out.
Assisting in locating and scheduling visits with physicians who are able to provide evaluations and second opinions.
Working together with knowledgeable and caring healthcare professionals who can assist in determining the most effective therapeutic approach for every person.
Prognosis
Some people with this illness mistakenly believe that their pain is just a common dental issue because it may initially only be felt in the jaw region. However, as time passes, the illness may worsen to the point where the intervals of time without pain are shorter and sometimes even disappear.
Furthermore, your pain may worsen to the point where it becomes difficult for you to perform daily duties and you may have to cut them out of your schedule out of dread of another attack. Over time, pain management may also become less effective.
Follow up
Regular follow-up with primary care physicians and specialists is necessary for patients to continue receiving treatment. Patients undergoing neuromodulator surgery are usually requested to visit the clinic a few months after the procedure. They may change the stimulation levels and evaluate the patient’s post-operative recovery during these appointments.
Checking in with a doctor on a regular basis guarantees that the treatment is accurate and efficient. Following any type of neurostimulation surgery, patients will also have follow-up visits with a device representative who will work with their doctors to modify the device’s parameters and settings as necessary.
Summary
On one side of the face, trigeminal neuralgia is a painful condition that feels like an electric shock. The trigeminal nerve, which transmits sensation from your face to your brain, is impacted by this chronic pain disorder. Even modest facial stimulation, like brushing your teeth or applying makeup, can cause a sharp, excruciating pain spike if you have trigeminal neuralgia.
At first, you might have brief, minor episodes. However, when trigeminal neuralgia worsens, episodes of excruciating pain may become longer and more frequent. Women are more likely than men to get trigeminal neuralgia, and those over 50 are more likely to experience it.
Trigeminal neuralgia does not always indicate that a person will always be in pain because there are numerous treatment options accessible. Trigeminal neuralgia is typically well managed by doctors with medication, injections, or surgery.
FAQs
The pain may then totally go away and not come back for a few months or years (a phase of time referred to as “remission”). In severe situations, however, there would not be any intervals of remission and attacks might happen hundreds of times a day.
It has been demonstrated that vitamin B12 acupoint injections work better for treating trigeminal neuralgia pain than carbamazepine does.
Asparagus, sweet potatoes, zucchini, quinoa, and avocado.
Carbamazepine is typically prescribed by doctors (Tegretol, Carbatrol, etc)
References
- Trigeminal neuralgia. (2023, February 14). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/trigeminal-neuralgia
- Trigeminal neuralgia – causes, symptoms, and treatments. (n.d.-b). https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Trigeminal-Neuralgia
- Singh, M. K., MD. (n.d.). Trigeminal neuralgia: practice essentials, background, anatomy. https://emedicine.medscape.com/article/1145144-overview?form=fpf#a1
- Trigeminal neuralgia – Symptoms and causes – Mayo Clinic. (2022, January 26). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/trigeminal-neuralgia/symptoms-causes/syc-20353344
- Trigeminal neuralgia. (n.d.-b). Physiopedia. https://www.physio-pedia.com/Trigeminal_Neuralgia
- Website, N. (2023b, February 10). Trigeminal neuralgia. nhs.uk. https://www.nhs.uk/conditions/trigeminal-neuralgia/
- Trigeminal neuralgia. (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/trigeminal-neuralgia
- Professional, C. C. M. (n.d.-h). Trigeminal neuralgia (TN). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/15671-trigeminal-neuralgia-tn#management-and-treatment
- Karegeannes, M. (2019, January 25). Trigeminal Neuralgia Physical therapy Treatment approach. Treating TMJ. https://www.treatingtmj.com/treatment/trigeminal-neuralgia-physical-therapy-treatment-approach/