Humerus Fracture
Table of Contents
Introduction
A humerus fracture is a fracture in the humerus bone of the upper arm.
There are two necks on the proximal humerus. The surgical neck is the metaphyseal area below the humeral head, while the anatomic neck is the old epiphyseal plate. The anterior and posterior humeral circumflex arteries supply blood to this region, with the axillary nerve as the major nerve.
The humeral shaft is a cylindrical bone that tapers to a triangular shape distally. This bone originates from the brachialis, triceps, and brachioradialis and serves as an insertion site for the pectoralis major, deltoid, and coracobrachialis.
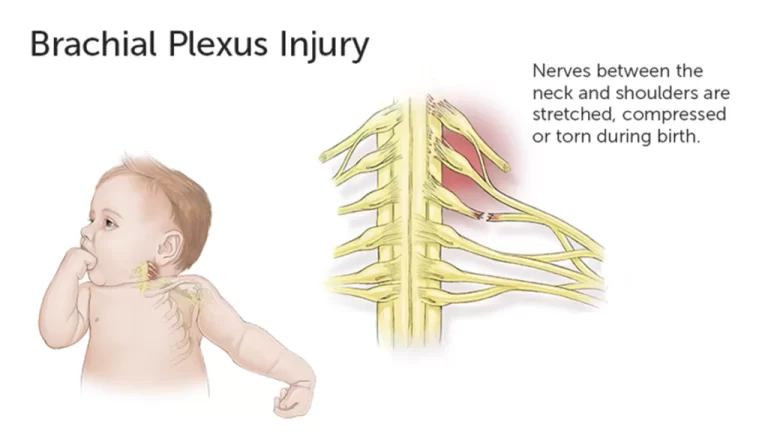
The primary nerve of the humerus shaft is the radial nerve, located approximately 14 cm from the lateral epicondyle and 20 cm from the medial epicondyle. The ulnar and radial nerves are the major nerves of the distal humerus.
Supracondylar fractures, single condyle fractures, bi-column fractures, and coronal shear fractures are all types of distal humerus fractures. Open reduction and internal fixation closed reduction percutaneous pinning, and intramedullary nailing or bracing are all treatment options.
Types of the Humerus Fracture
The shape or pattern of the break line is used to classify some fractures:
- The fracture is transverse.
- The fracture is oblique.
- Spiral fracture is a type of fracture.
- Fracture of a segment.
- A fracture that has been comminuted.
- Fracture caused by an impact.
- Fracture of the buckle.
- A hairline fracture has occurred.
Some fractures are classified based on how they occur:
- Fracture due to stress.
- Fracture of the avulsion.
The supracondylar humerus fracture
If you break your humerus just above your elbow, you may have a supracondylar fracture. This is a type of elbow fracture that almost always occurs in children. Supracondylar humerus fractures are typically caused by a child catching themselves from a fall while holding their arm out in front of them. A supracondylar fracture will be diagnosed and treated similarly to any other broken bone by your provider.
Open fracture or closed fracture
Your fracture will be classified as either open or closed by your doctor. An open fracture takes place if the bone breaks within the skin. Open fractures typically heal more slowly and are more susceptible to infections and other complications. Closed fractures are still dangerous because the bone extends through the skin.
Humerus fractures with displacement
Your fracture will also be described as displaced or non-displaced by your provider. When your bone broke, the pieces of your bone moved so far apart that a gap formed around the fracture. Non-displaced fractures continue to be broken bones, but the pieces were not moved sufficiently during the break to be out of alignment. Displaced fractures are far more likely to necessitate surgical repair.
Anatomy and location of humerus fractures
Your provider may mention the location of the fracture on your humerus. Providers use numerous terms to describe specific bones, but the most common ones are:
Location (proximal and distal): The terms proximal and distal describe where a fracture is located along the length of your bone. The top of your humerus is the proximal end. The bottom is the distal end. With a proximal humerus fracture, your upper arm bone is broken near the top — the end that connects to your shoulder. Similarly, a distal humerus fracture indicates that your bone has been broken at the bottom, closer to your elbow.
Anatomy (parts of your bones): Your bones are made up of many parts that can be damaged during a fracture. Your humerus has a head (the top end near your shoulder), a shaft, and a distal end (the bottom end near your elbow). Other common terms, such as surgical neck and greater tuberosity, refer to specific areas of your bone. These terms, which describe where your bone is damaged, are usually reserved for your healthcare provider.
Causes of the Humerus Fracture
Humerus fractures are most commonly caused by physical trauma, falls, excessive physical stress, or pathological conditions. Falls that result in humerus fractures in the elderly are typically associated with a preexisting risk factor for bone fracture, such as osteoporosis, low bone density, or vitamin B deficiency.
Proximal
Proximal humerus fractures are most common in elderly people who have osteoporosis and fall on an outstretched arm. Proximal fractures are caused less frequently by car accidents, gunshots, and violent muscle contractions caused by an electric shock or seizure. Other risk factors for proximal fractures include low bone mineral density, poor vision and balance, and tobacco use. After an excessive amount of throwing, such as pitching in baseball, a stress fracture of the proximal and shaft regions can occur.
Middle
Physical trauma or falls are the most common causes of middle fractures. Physical trauma to the humerus shaft causes transverse fractures, whereas falls cause spiral fractures. Metastatic breast cancer can also cause humerus shaft fractures. Long spiral fractures of the shaft in children could indicate physical abuse.
Distal
Physical trauma to the elbow region is the most common cause of distal humerus fractures. If the elbow is bent during the trauma, the olecranon is driven upward, resulting in a T- or Y-shaped fracture or the displacement of one of the condyles.
Symptoms of the Humerus Fracture
The following symptoms may occur depending on the type of fracture:
- Pain
- Swollen and bruised skin
- immobility of the shoulder
- A grinding sensation when moving the shoulder
- “It does not look right.”
- Occasionally, there is bleeding (open fracture).
- Normal arm use is lost if a nerve injury occurs.
Diagnosis of the Humerus Fracture
A physical exam and imaging tests will be used by your healthcare provider to diagnose a humerus fracture. If you’re admitted to the hospital after a trauma, this may be done in the emergency room.
If you are taken to the emergency room, a team of providers will stabilize you and treat your injuries in order of severity, especially if they are life-threatening. After you’ve been stabilized, imaging tests will be required to confirm your fracture.
To photograph your fracture, you’ll need at least one of the following imaging tests:
X-rays: An X-ray will confirm any fractures and show how badly your bones have been damaged.
Magnetic Resonance Imaging (MRI): Your provider may use an MRI to obtain a comprehensive picture of the damage to your bones and the surrounding area. This will also show them the tissue surrounding your bones.
CT scan: Unlike an X-ray, a CT scan provides your provider or surgeon with a more detailed picture of your bones and surrounding tissue.
Treatment of the Humerus Fracture
The treatment of a humerus fracture is dependent on several factors, including the type of fracture and the presence of loose bone fragments. Your doctor will begin by taking an X-ray of your arm to determine the best treatment. They may also ask you to perform some arm movements. This will assist them in determining the type of fracture you have and if you have any other injuries.
Proximal and mid-shaft humerus fractures rarely require surgery because the broken ends are usually close together. This facilitates the natural healing of your humerus. You will, however, need to wear a sling, brace, or splint to keep your arm from moving and to stabilize your shoulder, if necessary. Occasionally, surgery with plates, screws, rods, or replacement of your shoulder joint with a prosthesis is required.
Non-surgical treatment
Immobilization
If your fracture is minor and your bones did not move far out of place (non-displaced), you may only require a splint or cast. Splinting is typically worn for three to five weeks. If you require a cast, it will most likely be for a longer period, usually six to eight weeks. In both cases, you’ll most likely require follow-up X-rays to ensure that your bones are healing properly.
A sling may be required to keep your shoulder and arm in place, particularly if your humerus is fractured at the proximal end near your shoulder.
Closed reduction
Closed reductions are required for more severe breaks to set (realign) your bones. During this nonsurgical procedure, your provider will physically push and pull on the outside of your body to align the broken bones within you. To keep you comfortable during the procedure, you will be given one of the following medications:
- A local anaesthetic will be used to numb the area around your fracture.
- Sedatives are medications that are used to relax the entire body.
- General anaesthesia is used to put you to sleep during the procedure.
- Your provider will place you in a splint or cast after the closed reduction.
Surgical treatment
Some humeral fractures necessitate surgery. There are a few techniques your surgeon may use depending on the type of fracture you have and how badly your bones are damaged.
Internal fixation
Before securing your bones, the surgeon will realign (set) them to their ideal position so they can heal and grow back together. Internal fixation is a surgical procedure that involves inserting metal pieces into your bone to maintain it in place while it heals. You’ll need to limit how much you use your arm to allow your bone to heal completely.
Internal fixation techniques include the following:
- Rods: A rod that runs from top to bottom through the centre of your bone.
- Plates and screws: These are metal plates that are screwed into your bone to hold the pieces together.
- Pins and wires: Pins and wires are used to secure bone fragments that are too small for other fasteners. They are typically used in conjunction with rods or plates.
Some people live their entire lives with these pieces implanted in them. You may require additional surgeries to remove them.
Arthroplasty
If you break your elbow or shoulder, you may require an arthroplasty (joint replacement). Your surgeon will use an artificial joint to replace the damaged joint. Metal, ceramic, or heavy-duty plastic can be used to make the artificial joint (prosthesis). The new joint will look and move similarly to your natural joint.
Bone Grafting
If your humerus fracture is severely displaced or your bone isn’t healing as well as it should, you may require bone grafting. To repair your fractured bone, your surgeon will insert additional bone tissue. Following that, they’ll usually perform an internal fixation to hold the pieces of your bone together while it regrows.
Bone grafts are available from many different kinds of sources, including:
Internally from a different part of your body, often the upper hip bone.
An artificial beings replacement piece.
Your arm will be immobilized following surgery. Before you can use it as you did before the fracture, you’ll need to wear a splint, cast, or sling.
Complications of the Humerus Fracture
- Acute compartment syndrome (ACS) occurs when pressure builds up in your muscles, preventing blood from reaching tissue and causing permanent muscle and nerve damage.
- Malunion occurs when your broken bones do not align correctly while healing.
- Nonunion: the bones may not heal properly or at all.
- Osteomyelitis (bone infection): If you have an open fracture (the bone breaks through your skin), you are more likely to get a bacterial infection.
- Other internal damage: Fractures can harm the muscles, nerves, blood vessels, tendons, and ligaments in the area around the injury.
Prevention
To reduce your risk of injury, follow these general safety guidelines:
- Wear your seatbelt at all times.
- For all activities and sports, wear the appropriate safety equipment.
- Maintain a clutter-free home and workspace to avoid tripping yourself or others.
- To reach things around the house, always use the proper tools or equipment. Place your feet on chairs, tables, or countertops at all times.
- Maintain good bone health according to a diet and exercise routine.
- Talk to your doctor about getting a bone density test if you’re over 50 or have a family history of osteoporosis.
- If you have trouble walking or are at risk of falling, use a cane or walker.
Summary
The humerus is a bone that connects the proximal and distal hemispheres. It is a complex structure with two necks, the surgical and anatomic necks, and the axillary nerve as the major nerve. The humeral shaft is a cylindrical bone that serves as an insertion site for the pectoralis major, deltoid, and coracobrachialis.
The radial nerve is the major nerve of the humerus shaft. Distal humerus fractures can be classified based on the break line, type, and location. They are most commonly caused by physical trauma, falls, excessive stress, or pathological conditions.
Symptoms of a humerus fracture include pain, swelling, bruised skin, shoulder immobility, grinding sensations, and nerve damage.
Diagnosis involves a physical exam and imaging tests, which may include X-rays, MRIs, and CT scans. Treatment options include open reduction, internal fixation, closed reduction, percutaneous pinning, and intramedullary nailing or bracing.
The treatment of a humerus fracture depends on the type of fracture and loose bone fragments. An X-ray and arm movements are used to determine the best treatment. Proximal and mid-shaft fractures rarely require surgery, but slings, braces, or splints may be needed. Closed reductions are used for more severe fractures to realign bones. Surgical treatments include internal fixation, arthroplasty, and bone grafting.
Complications include acute compartment syndrome (ACS), malunion, nonunion, osteomyelitis, and other internal damage. To reduce injury risk, follow safety guidelines such as wearing seatbelts, using appropriate safety equipment, maintaining good bone health, and discussing bone density tests with a doctor. If you have difficulty walking or are at risk of falling, use a cane or walker.
FAQs
The surgical neck, which is a constriction distal to the tuberosities, is the most commonly fractured site of the humerus, especially in the elderly. PHF-relevant deforming forces include Pectoralis major: anterior/medial displacement of the humeral shaft.
Abstract. Nerve lesions are a relatively common complication following humeral shaft fractures, with the radial nerve being the most commonly affected.
This type of fracture is frequently caused by trauma from a fall or accident. Treatment varies according to the type and severity of the break but may include a sling, brace, splint, or cast, as well as surgery.
Proximal. A proximal humerus fracture is a break in your humerus near your shoulder.
Mid-shaft. A mid-shaft humerus fracture is a break in the humerus in the middle.
Distal. Distal humerus fractures happen near the elbow.
The anatomical neck is the region just below the head. The surgical neck (so named because it is the location of many fractures that require surgery) is where the neck continues along the humerus body.
References:
- Professional, C. C. M. (n.d.). Humerus Fracture. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22990-humerus-fracture
- Humerus Fracture (Upper Arm Fracture). (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/humerus-fracture-upper-arm-fracture
- Attum, B. (2023, July 4). Humerus Fractures Overview. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482281/
- Humerus fracture. (2023, May 20). Wikipedia. https://en.wikipedia.org/wiki/Humerus_fracture
- Roland, J. (2018, May 24). Humerus Fracture: How Long Will It Take to Heal? Healthline. https://www.healthline.com/health/humerus-fracture
- Proximal Humerus Fracture (Broken Shoulder). (n.d.). Orthopaedic Trauma Association (OTA). https://ota.org/for-patients/find-info-body-part/3831#/+/0/score,date_na_dt/desc/