Muscles of mastication
Table of Contents
Introduction
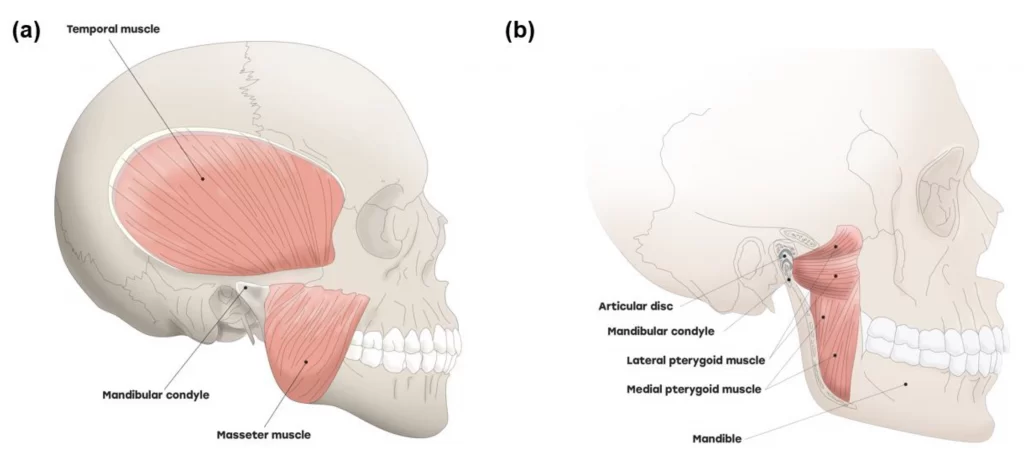
The muscles of mastication move your mandible during mastication and speech. The muscles of mastication are the Masseter, the Temporalis, The Lateral pterygoid, and the medial pterygoid. They develop from the mesoderm of the first branchial arch and are supplied by the mandibular nerve which is the nerve of the branchial arch. The muscles are described below.
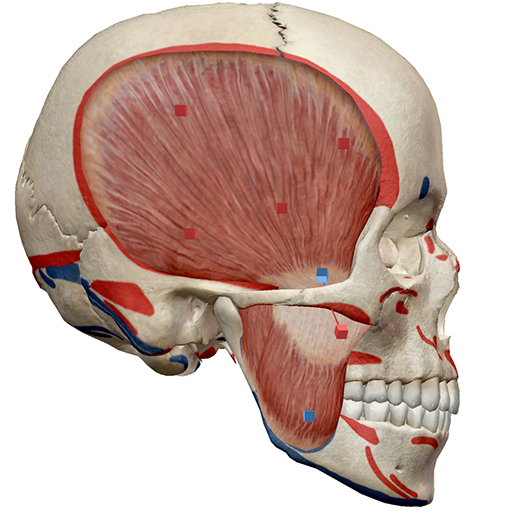
The Masseter
The masseter is a quadrilateral muscle which covers the lateral surface of the ramus of the mandible. The masseter muscle fibres are arranged in three layers.
Origin
Superficial layer from the anterior 2/3 of the lower border of the zygomatic arch and from the process of zygomatic of the maxilla
Middle layer from the anterior 2/3 of the deep surface and posterior 1/3 of the lower border of the zygomatic arch.
Deep layer from the deep/inferior surface of the zygomatic arch (posterior 1/3)
Insertion
The superficial fibres pass downwards and backwards at an angle of 45 degrees. superficial fibres are inserted into the lower part of the lateral surface of the ramus of the mandible.
The middle and deep fibres pass vertically downwards. the middle fibres are inserted into the middle part of the ramus, and the deep fibres into the upper part of the ramus and into the coronoid process.
Nerve supply
The nerve supply of the masseter muscles is the Masseteric nerve, a branch of the anterior division of the mandibular nerve (CN V3)
Blood supply
The blood supply of the masseter muscle is the Masseteric artery
Action
The masseter muscle Elevates the mandible and clenches the teeth
The temporalis
This muscle fills the temporal fossa.
Origin
Temporal fossa, excluding the zygomatic bone,
Temporal fascia
Insertion
The fibres of the temporalis muscle converge and pass through the gap deep to the zygomatic arch. They are inserted into The margins and deep surface of the coronoid process; and the anterior border of the ramus of the mandible.
Nerve supply
The nerve supply of the temporalis muscles is the Deep temporal branches from the anterior division of the mandibular nerve (CN V3)
Blood supply
The blood supply of the temporalis muscle is the Deep temporal branches of the maxillary artery, middle temporal branches from the superficial temporal artery
Action
Anterior fibres: Elevates mandible
Posterior fibres: Retracts mandible
The lateral pterygoid
The lateral pterygoid muscle has the upper head and lower head.
Origin
Both heads of the lateral pterygoid muscles arise from the sphenoid bone.
The upper head is small. its origin is from the infratemporal surface and crest of the greater wing of the sphenoid bone.
The lower head is large. its origin is from the lateral pterygoid plate.
Insertion
The lateral pterygoid muscle fibres run backwards and laterally and converge to be inserted into the pterygoid fovea on the anterior surface of the neck of the mandible and the anterior margin of the articular disc and temporomandibular joint capsule.
Nerve supply
The nerve supply of The lateral pterygoid muscle is the branches from the anterior division of the mandibular nerve (CN V3)
Blood supply
The blood supply of the lateral pterygoid is from the pterygoid branches of the maxillary artery and the ascending palatine branch of the facial artery.
Action
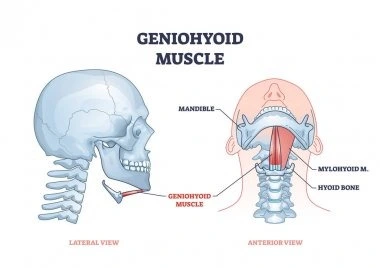
Depression of the mandible to open the mouth,(with suprahyoid muscle)
The lateral and medial pterygoid muscles of both sides act together to protrude the mandible.
The medial pterygoid muscle and lateral pterygoid muscles of both sides contract alternately to produce side-to-side movements of the mandible(as in chewing).
The medial pterygoid
The medial pterygoid is a quadrilateral muscle and it has a small superficial head and a large deep head which forms the major part of the muscle.
Origin
The superficial head(small slip) of the medial pterygoid muscle originates from the tuberosity of the maxilla and adjoining bone.
The deep head of the medial pterygoid muscle originates from the medial surface of the lateral pterygoid plate and adjoining part of the palatine bone.
Insertion
The medial pterygoid muscle fibres run downwards, backward, and laterally to be inserted into the roughened area on the medial surface of the angle and the adjoining part of the ramus of the mandible, below and behind the mandibular foramen and the mylohyoid groove.
Nerve supply
The nerve supply of the medial pterygoid muscle is the Branch of the main trunk of the mandibular nerve.
Blood supply
The blood supply of the medial pterygoid muscles is the pterygoid and buccal branches of the maxillary artery. To a lesser extent, ascending palatine artery and muscular branches of the facial artery also contribute to the blood supply of the medial pterygoid muscle.
Action
Elevates the mandible
Helps to protrude the mandible
See “c” under lateral pterygoid
Clinical significance
Temporomandibular joint dysfunction
Temporomandibular dysfunction can be caused by the imbalance of forces within the muscles of mastication. Grinding of teeth at night (bruxism) is a common cause of Temporomandibular dysfunction secondary to a resultant imbalance in the muscle of mastication forces from excessive grinding of the teeth.
Myofibrotic contracture
Myofibrotic contracture involves a painless shortening of muscle as a result of fibrosis in and around the remaining contractile muscle tissue. There are limited mouth opening and unyielding resistance to passive jaw muscle stretching.
Myositis
Myositis is inflammation of the muscles caused by acute trauma or infection. It is characterized by swelling, redness overlying skin, and increases in the temperature over the affected part. It can cause jaw dysfunction and a limited range of movement(ROM).
Physiotherapy treatment for the muscles of mastication
Control of Jaw Muscles
to Control Jaw Muscles First, teach recognition of the resting position of the jaw. The lips are closed, teeth apart slightly, and the tongue resting lightly on the hard palate behind the front teeth. The patient should breathe in and breathe out slowly through the nose, using diaphragmatic breathing.
Teach control while opening and closing the jaw through the first half of the Range Of Motion. With the tongue on the roof of the mouth, the patient opens the mouth while trying to keep the chin in the midline. You can use a mirror for visual reinforcement. The patient is also taught to lightly palpate the lateral pole of each condyle of the mandible bilaterally and to attempt to maintain symmetry between the movement of the two sides while opening and closing the mouth.
If the jaw deviates while opening or closing the mouth, have the patient practice lateral deviation to the opposite side. The lateral motion should not be excessive or should not cause pain. You can Progress by applying gentle resistance with the thumb against the chin. Do not overpower the muscles.
Stretching Techniques
If there is restricted jaw opening, determine if it is from hypomobile tissues or from the dislocated meniscus. Passive stretching and mobilization of the joint are used to stretch the tight tissues. Joint distraction can be used to reposition a meniscus that is blocking the opening of the jaw.
Passive Stretching
Stretching to increase jaw opening if indicated. It Begins by placing layered tongue depressors between the central incisors.
The patient can gradually work to increase the number of tongue depressors used until he or she can open approximately far enough to insert the index and middle fingers’ knuckles.
Self-stretching
Self-stretching can be performed by placing each thumb under the upper teeth and the index or middle fingers over the lower teeth and pushing the teeth open.