Muscle Tone Physiology and Abnormalities
Table of Contents
What is a Muscle Tone?
Due to reciprocal and hierarchical anatomical relationships, muscle tone is a dynamic and complicated condition. Its input and output systems control it and interact crucially with the demands of task performance and power. In simple terms, tone is a motor control concept that maintains power balance inherently.
The brainstem reticular system (a common pathway for ascending and descending tracts), the spinal cord (the main pathway for ascending and descending tracts), the cerebellum (fine-tuning), the cortex (extensive processing capability with highest degree of freedom), and the muscle spindle(last common pathway with least degree of freedom) make up this hierarchy of motor control.
We have covered the discussions around the definition and classification of muscle tone in this review and the methods and processes in charge of maintaining tone.
The two forms of hypertonia, spasticity, and rigidity, have been explained regarding supraspinal pathway malfunction and the connection between the spinal cord and the muscle spindle.
The physiological malfunction of the tone pathways is not directly linked to the other two altered tone diseases, namely dystonia and paratonia.
Because dystonia is a system-level processing issue, spasticity and rigidity are primarily output system issues in the motor control system.
Due to network disruption in the thalamocortical circuits, the basal ganglia, and their connections, dystonia and paratonia have changed tone.
From a movement disorder position, the processes underlying them have been explored later since they have importance from a clinical and pathophysiological point.
Definition of Muscle Tone
“The tension in the relaxed muscle” or “the resistance, observed by the examiner during passive stretching of a joint when the muscles are at rest” are the most common definitions of muscle tone.
There are several issues in this definition of tone, such as the difficulty with the definition surrounding the term “resistance to passive stretch” and the possibility of subjective fluctuation during clinical examination and assessment interrater variability due to the use of the phrase “felt by the examiner”.
Studies that use electromyographic (EMG) measurement frequently compare baseline EMG levels in a relaxed state with muscle tone.
Muscle tone may be understood mathematically as the change in force or resistance per unit change in length.
Bernstein stressed that, contrary to common opinion, muscle tone may indicate a person’s level of readiness for a movement. As a result, it might not be able to determine muscle tone when a person is instructed to remain still and not move.
According to this concept, muscular tone actively influences posture and movement. Similarly, “the constant muscular activity that is necessary as a background to actual movement to maintain the basic attitude of the body, particularly against the force of gravity” is how Carpenter et al. define tone clinically.
The degree of tension, or resistance to movement, in muscles is known as muscle tone. When we sit and stand, our ability to maintain our body’s upright posture is supported by our muscular tone.
We can move because of changes in muscle tone. The capacity to move with control, speed, and volume is also influenced by our muscle tone.
Classification of Muscle Tone
There are two categories of muscle tone: “postural” and “phasic.” Gravity is the primary starting cause for postural tone in axial muscles. It occurs as a prolonged contraction of the muscles and tendons as a result of continual stress.
On the other hand, phasic tone is often evaluated clinically in the extremities as a quick reaction. It happens when a tendon, a muscle that is linked to it, or more specifically, the muscular spindle, stretches quickly. In addition, as was previously said, muscle tone may be divided into its active and passive components.
Muscle Tone Assessment
The assessment of muscle mass, tone, and strength is part of the motor exam. Assessments of body alignment, coordination, and the existence of involuntary movements are also included.
You have two options: either assess each component in turn (e.g., look at all motor activities in the arms, legs, and trunk) or assess them one after the other (e.g., assess strength in every body area, assess tone, etc.).
Evaluation of Muscles
At rest, check the symmetry and mass of your muscles. Look out for the appearance of atrophy in particular. Take note of any uncontrollable movements, such as fasciculations, tics, or tremors. Athetoid, hemiballismus, and choreiform motions are examples of additional involuntary movements. Note the rhythm, amplitude, pace, quality, and any correlation with activity and posture, if any are present.
The resistance of a muscle to passive stretch is used to determine the muscle’s tone. A significant amount of normal variance exists. Flex and extend the patient’s wrists, knee, ankle, and elbow joints to test this.
Shake the hand lightly back and forth while holding the forearm if you notice less resistance. The hand should not be too floppy, but it should be able to move easily back and forth.
Try to get the patient to relax more if they experience increasing resistance. Next, find out if the resistance changes as the limb moves or if it is constant throughout the range of motion and present in both flexion and extension.
The Medical Research Council (MRC) scale is used to evaluate muscle strength, with zero denoting no contraction and five denoting normal strength.
Anatomy Related to Regulation of Muscle Tone
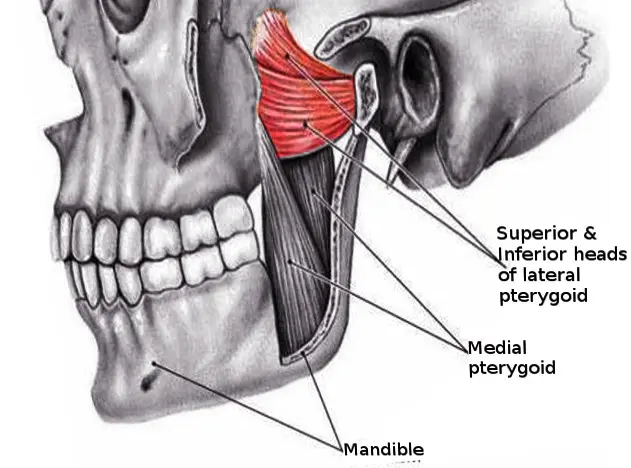
Both spinal and supraspinal processes control muscle tone. While interneurons and the interplay of the spinal cord with the muscle spindle determine spinal control, the cerebellum and facilitatory and inhibitory long tracts control supraspinal control.
Spinal Control
Interaction between Muscle Spindle and Spinal Cord
Muscle tone control requires muscle sensations regarding length and tension, which are transmitted to the spinal cord. The Golgi tendon organs supply information about tendon tension and the rate at which it changes.
In contrast, intrafusal fibers transmit information about muscle length and the rate at which it changes. During a stretch, type Ia afferents measure the speed at which muscle length changes (dynamic response).
On the other hand, the steady-state length of the muscle is detected by the tonic activity of type Ia and II afferents (static response). Information is sent from the Golgi tendon organs by type Ib afferents.
Tone is produced by the muscle spindle by triggering the stretch reflex. Both extramural and intrafusal fibers will contract as a result of alpha–gamma co-activation, which occurs when a motor command is transmitted to the gamma motor fibers that supply intrafusal fibers.
There are two different kinds of stretch reflexes: dynamic and static. When a muscle is suddenly stretched rapidly, nuclear bag fibers are activated. These fibers react to the rate or velocity of the strain, and Ia afferents, or annulospiral endings, transmit the dynamic signal to the spinal cord.
Muscle contraction occurs abruptly as a result of the efferent signal from the cord (alpha motor neuron) traveling via alpha efferents to intrafusal fibers (dynamic stretch reflex). The clinical elicitation of the deep tendon reflexes depends on this.
Interneurons
An essential component of the stretch reflex arc, interneurons are crucial for preserving muscle tone. Many descending fiber networks either stimulate or inhibit them.
There are other interneuronal routes; we will discuss how they relate to spasticity later.
The most important factors for maintaining muscular tone are presynaptic inhibition, non-reciprocal Ib inhibition by the Posterior tendon organ, reciprocal Ia inhibition from antagonist muscle, and recurrent inhibition by the Renshaw cell.
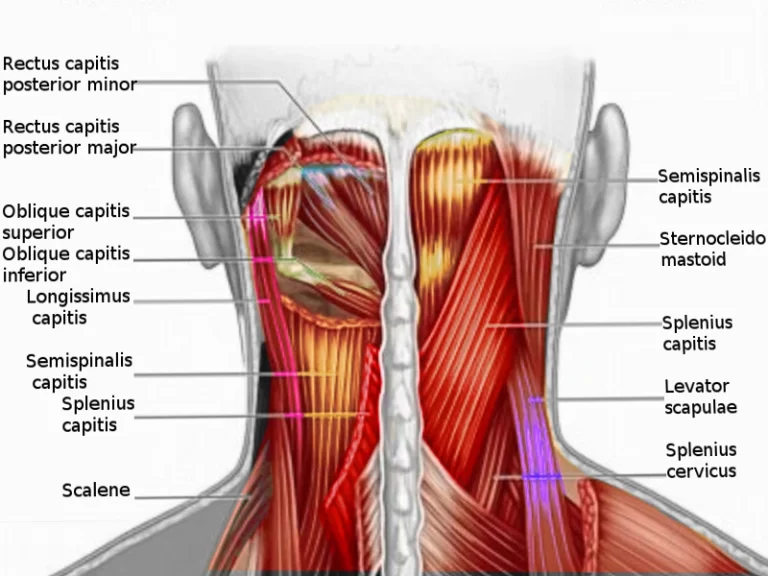
Supraspinal Control via Descending Long Tracts
In humans, two inhibitory and two facilitatory descending pathways interact to primarily control the supraspinal effect on muscle tone and stretch reflexes.
Inhibitory Tracts
Corticospinal tract/CST
Corticoreticular (from premotor cortex) and dorsal reticulospinal tract/ dorsal RST (from medullary reticular formation)
Facilitatory Tracts
Vestibulospinal tract/VST
Medial reticulospinal tract/medial RST
The facilitatory medial RST and inhibitory dorsal RST are the two primary tracts that control muscle tone.
Role of Cerebellum
The dorsal reticular formation, which gives birth to dorsal RST, is activated by the medial part of the anterior lobe of the cerebellum.
As a result, the cerebellum indirectly reduces muscle tone by blocking gamma motor neurons via dorsal RST.
However, the pontine reticular development is activated by the lateral region of the anterior lobe. Thus, activating gamma motor neurons via medial RST indirectly promotes muscle tone.
In humans, cerebellar lesions frequently result in hypotonia because the lateral section of the anterior cerebellum is more developed.
However, the vestibular nucleus, which is linked to the vestibulocerebellum, is what activates the alpha motor neurons. Consequently, the cerebellum is a crucial location for “alpha-gamma linkage” regulation.
Spasticity
As a part of the upper motor neuron syndrome, spasticity is defined as “a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflex.”
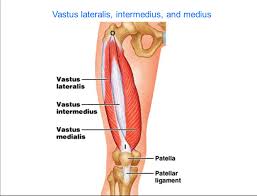
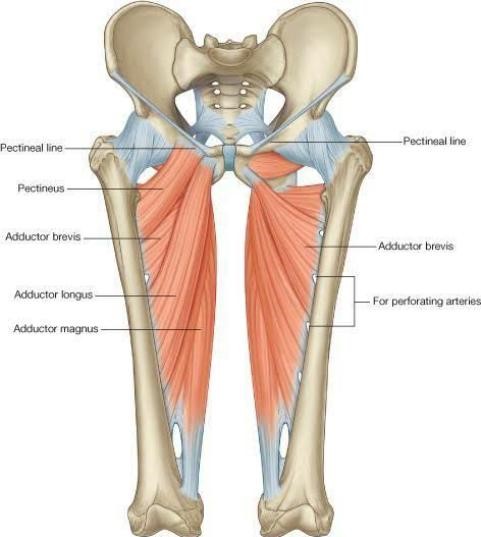
However, muscle length also affects spasticity in addition to velocity. In the knee extensor (quadriceps), spasticity increases with muscle length; whereas, in the upper limb flexors (biceps, for example) and ankle extensors (gastrocnemius, soleus), spasticity increases with muscle length. Additionally, Lance’s definition disregards how sensory input (covered later) contributes to spasticity.
The Support Programme for Assembly of a Database for Spasticity Measurement (SPASM) defines spasticity as disrupted sensory-motor control arising from an upper motor neuron injury, manifesting as intermittent or prolonged involuntary activation of muscles.
The definition included the part that impaired sensory input—rather than just motor—plays in spasticity. The IAB-Interdisciplinary Working Group for Movement Disorders provided a more comprehensive definition of spasticity in 2018, stating that it is “involuntary muscle hyperactivity in the presence of central paresis.”
The term “involuntary muscle hyperactivity” has been defined in this definition as a spectrum that includes the following: (i) “spasms” triggered by sensory or auditory stimuli; (ii) “rigidity” triggered by slow passive joint movements; (iii) “dystonia” when the involuntary muscle hyperactivity is spontaneous; and (iv) “spasticity sensu strictu” triggered by rapid passive joint movements.
Additionally, the group has suggested an axis-based approach to spasticity, which includes four components: extra central nervous system impairments (axis 4), localization (axis 3), etiology (axis 2), and clinical description (axis 1).
The Frequency of Spasms Score, Tardieu Scale, and Modified Ashworth Scale can all be used to gauge the severity of muscular hyperactivity.
Based on the relative participation of the phasic (dynamic) or tonic (static) components of muscular stretch reflexes, spasticity can be categorized as either “tonic” or “phasic.”
Patients who are mobile after a spinal injury have “phasic” spasticity with rapid stretch responses and clonus.
However, passive ankle stretching and vibratory tonic reflex tests reveal the development of “tonic” spasticity in non-ambulatory individuals.
The pathophysiology of the clasp-knife phenomena and clonus will be covered in the next part, after which we will address spinal and supraspinal components that contribute to spasticity, including the importance of sensory input as demonstrated by recent research.
Factors Contributing to Spasticity
Spinal Influence
The pathophysiology of the clasp-knife phenomena and clonus will be covered in the next part, after which we will address spinal and supraspinal components that contribute to spasticity, including the importance of sensory input as demonstrated by recent research.
The descending serotonergic and noradrenergic drive can influence the prolonged depolarization (plateau potential) caused by voltage-dependent persistent inward current (PIC), which is mediated by Na+ and Ca2+ channels.
Normally, descending monoaminergic drive stimulates alpha motor neurons at the ventral horn through 5HT2 and NEa1 receptors, whereas it decreases alpha motor neurons at the dorsal horn through 5HT1b/d and NEa2 receptors.
Due to the lack of this descending monoaminergic effect, motor neuron hyperexcitability develops at the ventral horn in the acute period following an injury to the spine, but sensory input is disinhibited and stimulated at the dorsal horn.
However, until motor neurons repair their excitability, interneuronal excitability does not cause acute spasticity to occur. Spasticity develops in the chronic stage due to denervation hypersensitivity of ventral horn motor neurons to the residual monoaminergic input and PIC activation.
Recent research has shown that altered spinal inhibitory circuitry plays an important part in spasticity, in addition to excitatory reasons.
Reduced presynaptic inhibition of Ia afferents, decreased disynaptic reciprocal Ia afferent inhibition from the antagonist muscle group, decreased Ib afferent mediated inhibition by the Golgi tendon organ, and altered recurrent inhibition by Renshaw cells (dubious role) may all contribute to disinhibition of the alpha motor neuron in spasticity.
Supraspinal Influence
In a typical situation, the facilitatory drive (on extensor tone) provided by medial RST and, to a lesser extent, VST, and the inhibitory drive of CST and dorsal RST balance human muscle tone seriously.
Among them, flexor reflex afferents (FRA) are inhibited by dorsal RST. The corticospinal tract (CST) and dorsal RST are located in the lateral funiculus of the spinal cord, while the medial RST and VST are found in the anterior funiculus.
This makes the following summary of how spinal and cortical injuries affect muscle tone possible.
Cortical Lesions
It takes more than just one CST interaction to cause spasticity. Due to the involvement of corticoreticular fibers, which connect the premotor cortex to the medullary reticular formation, the source of dorsal RST, cortical lesions cause spasticity.
Without the inhibitory impact of dorsal RST, the unopposed facilie.tatory activity of medial RST results in hemiplegia with stiffness and antigravity posture.
Spinal Cord Lesions
Incomplete/partial myelopathy involving lateral funiculus
If the CST is the only organ involved, weakness, hypotonia, and loss of superficial reflexes will follow. Due to unopposed medial RST activity, spasticity and hyperreflexia will occur if dorsal RST involvement is increased.
Antigravity muscles will have a higher incidence of spasticity, which can lead to paraplegia in terms of extension and extensor spasms.
If pressure sores trigger FRA, flexor spasms may result. However, there won’t be significant weakening if dorsal RST involvement is limited to sparing CST, leading to spasticity.
Complete myelopathy with involvement of all four tracts
Because medial RST and VST do not provide any facilitatory input, there will be less spasticity in this situation. When FRA is disinhibited, flexion and flexor spasm paraplegia occur.
Role of Sensory Feedback
According to recent research, hyperexcitable reflexes are either insignificant or nonexistent in stabilizing the joint and posture in the context of diminished muscular strength, while co-activation of antagonist muscles, rigid posture, and stiff gait of spasticity may be adaptations. When motions are not adequately anticipated for their sensory effects, spastic movement problems can occur.
The patient with a UMN lesion will have trouble optimizing the movement since there is no solid prediction of somatosensory feedback from the moving limb.
Hence, co-contraction of the surrounding muscles may be a tactic to reduce erratic movement and, to the greatest extent feasible, stabilize the movement. Therefore, an attempt to compensate for the weakness.
The idea may be used for simple hereditary spastic paraplegia (HSP), a condition in which there is involvement of the corticospinal tract (CST) and large fiber proprioceptive sensory loss.
As was previously mentioned, a selective loss of CST is insufficient to cause noticeable spasticity beyond weakening.
Therefore, the clinical presentation of significant spasticity out of proportion to weakness in HSP may potentially be related to impaired sensory input.
DeLuca et al. noted that whereas small diameter fibers are mainly impacted in multiple sclerosis (MS), both big (>3 µm2) and small (<3 µm2) diameter nerve fibers of motor (CST) and sensory (posterior column) routes experience axonal loss in HSP.
Therefore, in contrast to MS, where weakness predominates, the affection of large-diameter nerve fibers may be the cause of the prevalence of spasticity observed in HSP.
Non-Neural Factors
As was previously mentioned, variations in non-neural variables such as tissue viscoelastic characteristics (e.g., elastic stiffness, viscous damping) can also elicit spasticity.
Pathophysiology of Clasp-Knife Phenomenon
“Regular, repetitive, rhythmic contractions of a muscle subjected to sudden, maintained stretch” is the definition of clonus.
A clonus that lasts five beats or more is regarded as clinically aberrant. Several explanations for the pathological foundation have been offered in the literature: Stretch reflex-inverse stretch reflex sequence;(2) disruption of the antagonist’s inhibition by Renshaw cells and type Ia inhibitory interneuron mediated contraction;(3) hyperactivity of the muscle spindles resulting in activation of all motor neurons from the burst of impulses coming from the spindle; consequent muscle contraction stops spindle discharge; during maintenance of the sustained stretch, the muscle is again stretched as soon as the muscle relaxes resulting in spindles being stimulated again.
Rigidity
In contrast to spasticity, rigidity is independent of movement speed. The “lead pipe” effect, which causes consistent resistance to passive stretching in all directions, is caused by it equally affecting flexors and extensors.
The “cogwheel phenomenon” of hypertonicity in Parkinson’s disease (PD) was also seen to occur regularly at a frequency of 6–9 Hz, which is greater than the frequency of rest tremor (4–5 Hz) and postural tremor (5–6 Hz).
According to a new agreement, superimposed tremor, often known as “an underlying, not yet visible, tremor,” causes “cogwheel” stiffness in Parkinson’s disease (PD) and causes an occasional increase in tone during passive joint movement.
Therefore, even in the absence of overt tremor, cog-wheeling may occur. One of Parkinson’s’ hallmarks is rigidity. It is seen in both the “akinetic-rigid” and “tremor dominant” PD phenotypes, albeit it is more pronounced in the former.
In idiopathic Parkinson’s disease (IPD), appendicular stiffness often outweighs axial rigidity; however, significant axial rigidity is indicative of atypical parkinsonism, such as progressive supranuclear palsy (PSP).
Factors Contributing to Rigidity
Exaggeration of Long-Latency Stretch Reflexes (LLSR)
The finding that Parkinsonian stiffness improved after dorsal cord excision supported the first investigations’ hypothesis that the stiffness was probably a spinal reaction.
The primary reason was believed to be an enhanced response of the muscle receptors to passive strain.
Nevertheless, further research using microneurographic recordings discovered that stiffness was not caused by the increased muscle afferent discharge from the larger fusimotor drive.
In the research using electrophysiological analysis, there was no significant difference in the monosynaptic segmental stretch reflexes between PD patients and healthy volunteers.
Instead, it was shown that most of the Ia afferent mediated spinal reflexes in PD patients, including tendon jerks, H-reflex, and tonic vibration reflex, were normal.
Thus, the focus increasingly turned from spinally mediated reflexes to the increased long-loop or long-latency stretch reflex (suspensional effect) on Parkinsonian stiffness.
Berardelli et al. observed a correlation between stiffness and an increase in LLSR and hypothesized that group II afferents may play a role in this.
Despite observing increased LLSR in Parkinson’s disease, Rothwell et al. were unable to establish a quantifiable link between this and stiffness.
They proposed that augmented late polysynaptic reflexes mediated by cutaneous afferents may potentially play a significant role in Parkinsonian rigidity and that LLSR is not the only cause of it.
Enhanced Shortening Reaction (SR) and Stretch-Induced Inhibition (SII)
Overstated LLSR can account for hypertonia in Parkinson’s disease (PD), but what about the resistance to passive stretch that is constant over the range of motion? Westphal first observed an abnormal reaction in the shortening muscle, and Sherrington later dubbed this phenomenon the “shortening reaction” (SR).
The phenomena of SR may be caused by changes in the pathways for short-latency autogenic inhibition, which are mediated by increased excitability of Ia and Ib spinal interneurons.
However, when a muscle is constantly stretched or lengthened past a crucial joint angle, there is a significant drop in resistance.
Stretch-induced inhibition (SII) or a “lengthening reaction” is the term used to describe the phenomena. When assessing limb tone in Parkinson’s disease, the combined effects of SR and SII produce a “lead pipe” effect.
Role of Brainstem
Recent research has brought more attention to the non-dopaminergic system’s involvement in Parkinson’s disease. Recently, Linn-Evans et al. observed that PD patients with REM sleep without atonia (PD-RSWA+) had greater symmetric stiffness in their upper limbs while awake than did controls and patients with atonia (PD-RSWA-).
The brainstem circuit sustaining motor neuron excitability and postural control throughout waking and REM sleep have similarities in terms of tone. Alpha-synuclein accumulation has been seen in the nuclei of both circuits in Parkinson’s disease (PD), including the caudal raphe, locus coeruleus, nucleus reticularis gigantocellularis (NRGC), sublaterodorsal nucleus (which regulates tone during REM sleep), and pedunculopontine nucleus (PPN).
The globus pallidus interna (GPi) provides inhibitory input to PPN. Degeneration of PPN and NRGC in Parkinson’s disease (PD) reduces the excitation of Ib spinal interneurons, which disinhibits alpha motor neurons and may result in stiffness.
Similarly, increased inhibitory tone in PD might result from GPi to PPN. Additionally, Heckman et al. have demonstrated how persistent inward current (PIC) firing, which is promoted by the locus coeruleus and caudal raphe, respectively, has a noradrenergic and serotonergic effect on motor neuron excitability.
In Parkinson’s disease (PD), affection of these pathways may result in a change in the motor neuron’s firing pattern in response to external stimuli, which can cause stiffness.
Non-Neural Factors
As was previously mentioned, parkinsonian stiffness may also be influenced by the elastic characteristics of surrounding connective tissues and muscle fibers.
According to Watts et al., upper limb stiffness was higher in PD patients even with minor motor symptoms compared to controls in a relaxed state, but without any EMG activity.
The study emphasized how stiffness is influenced by passive mechanical characteristics. Additionally, Xia and others have observed that while neural input dominates, non-neural variables also contribute to Parkinsonian stiffness.
Network Hypothesis of Parkinsonian Rigidity
Baradaran and company investigated the relationship between Parkinsonian stiffness and changes in functional connectivity in brain networks. As the stiffness increased, they saw an increasing abnormality in the premotor.
pre-cuneus link (a change attributable to the illness), whereas the cerebellar? the premotor connection became closer to normal (a compensatory mechanism).
The akinetic-rigid subtype of Parkinson’s disease (PD) is thought to have a more aggressive course of functional decline than the tremor-dominant subtype due to significant loss of brain function and abnormal functional connectivity in fronto-parietal networks, which are critical for motor planning and execution.
Pathophysiological Basis of Activation Maneuver
The increase in stiffness in the contralateral limb during isometric or rhythmic muscular contraction is an intriguing phenomenon associated with Parkinson’s disease (PD) that is yet poorly understood.
Several possible explanations have been proposed in the literature for this phenomenon, such as(1) enhanced LLSR via the transcortical pathway;(2) altered spinal motoneuron excitability mediated by the crossed sensory afferent feedback via lb afferent input, which results in diminished SR and increased sensitivity to passive stretch; (3) facilitation of bilateral descending reticulospinal projection; and (4) an analog of the “Jendrassik maneuver,” in which contraction of a different body part facilitates the H-reflex and improves the stretch reflex response.
Dystonia
Pathophysiology and Mechanisms
Dystonia is defined as persistent or intermittent muscular contractions that produce abnormal, frequently repeated, postures, motions, or both. Usually patterned, these motions might be twisted or tremulous, and they can be made worse by deliberate action.
There are several types of dystonia, including focal, segmental, hemi dystonia, and generalized.
The diverse range of aetiologies and variable presentation of dystonia, from hereditary origins to neurodegenerative illnesses, suggests many processes involved in the pathophysiology of dystonia.
When analyzing the processes behind dystonia, the basal ganglia-thalamo-cortical circuitry has been the focal point of most of the conjecture.
However, newer imaging modalities and electrophysiological studies have expanded the range of neuroanatomic correlates involved in dystonia. Anomalies in sensory processing and sensorimotor integration are indicated by the phenomena of mirror movements and sensory tricks observed in dystonia.
Anatomical Correlates of Dystonia
The most significant structure linked to dystonia has been suggested to be the basal ganglia and their aberrant connections. For an extended period, a clear illustration of this correlation is secondary dystonias brought on by basal ganglionic injuries.
Additional evidence supporting the key involvement of the basal ganglia in the genesis of dystonia comes from the improvement of some cases of dystonia by deep brain stimulation of the internal segment of the globus pallidus or the improvement of dopa-responsive dystonias (DRD) by levodopa.
In spinocerebellar ataxias (SCA), dystonia is not always present, although on occasion it does when cerebellar atrophy predominates and the basal ganglia are spared.
SCA-6 often manifests as a pure cerebellar ataxia phenotype and has a pure cerebellar pathophysiology. Nonetheless, these individuals have dystonia, which cannot be accounted for by malfunctioning of the basal ganglia.
The voxel-based morphometry studies revealed a substantial increase in the grey matter volume in the hand representation region of patients with focal hand dystonia.
The dorsolateral prefrontal cortex, inferior parietal regions, and cerebellum also showed this peri-rolandic rise, while the lentiform nucleus did not.
Similar anatomical anomalies in the primary sensorimotor cortex, cerebellum, and pulvinar nuclei of the thalamus have been seen in the writer’s cramp.
Mechanisms of Dystonia
With the development of transcranial magnetic stimulation (TMS) and repeated transcranial magnetic stimulation (rTMS), the pathophysiological pathways generating dystonia were revealed in the absence of animal models.
The TMS protocols that were created as a research tool have brought attention to the physiological dysfunctions described below in dystonia patients.
Loss of Inhibition
The physiological loss of inhibition is the cause of a lack of surround inhibition, co-contraction of antagonistic muscles, and overflow of activity into the muscles not intended for the action.
To prevent overflow contraction, the muscles surrounding an active contracting muscle actively block it.
This phenomenon is known as surround inhibition, and it is caused by corticism. Using a single TMS pulse, Sohn et al. reported this occurrence in healthy individuals.
The motor evoked potential (MEP) recorded on TMS from the ulnar innervated abductor digiti minimi (ADM) decreased upon voluntarily flexing the index finger, which is innervated by the median nerve.
The same author group showed that during index finger flexion, the MEP amplitudes of ADM were elevated by up to 270% in seven patients with focal hand dystonia when compared to controls, demonstrating a lack of surround inhibition.
Similarly, Ikoma et al. observed increased cortical excitability on TMS administered at varying stimulus intensities and with varying degrees of muscle facilitation in 11 patients with task-specific dystonia, indicating a greater quantity of activated motor units.
When observing the cortical reserved period (CSP), which is the cessation of voluntary electromyographic muscle activity after a suprathreshold TMS pulse, intracortical inhibition is evaluated electrophysiological.
In 10 dystonia patients, Rona et al. discovered that the CSP was shorter in task-specific dystonia than in generalized dystonia.
The previously mentioned monosynaptic and long-latency stretch reflexes are prolonged with slower stretch in dystonia and frequently elicit reflex activation in distant muscles, suggesting overflow.
The typical dystonia-related co-contraction of opposing muscles is caused by a breakdown in reciprocal inhibition. Dysfunctional descending inputs from higher centers are thought to be the cause of the abnormalities in spinal reflexes observed in dystonia.
Abnormal Sensory Function
A well-known dystonia symptom, ain has been observed in almost 70% of instances with cervical dystonia.
These individuals experience sensory symptoms such as photosensitivity in blepharospasm or neck discomfort before cervical dystonia, even in the lack of overt sensory abnormalities on clinical examination.
The “geste antagonist,” often known as the sensory trick, is the most remarkable dystonia phenomenon. The patient is making this choice to lessen the intensity of their dystonia.
The dystonia was relieved by a sensory trick, which led to the incorrect diagnosis of psychogenic dystonia.
However, it was later demonstrated that a significant physiological change observed in dystonia involves aberrant sensory function and disrupted sensorimotor integration.
Consequently, the tonic vibration reflex (TVR), a polysynaptic spinal cord reaction involving gamma motor neurons and muscle spindle afferents, is elicited by transcutaneous vibration applied to the muscle at a frequency of 50–120 Hz.
According to one theory, the way the sensory trick functions is by lowering the gamma drive to the spindles in comparison to the activity of the alpha motor neurons.
The ability for spatial discrimination is measured using the grating orientation task (GOT). It finds the minimum grating ridge width at which the orientation can be reliably identified, and it is applied to both hands’ fingers.
GOT anomalies with elevated spatial discrimination threshold have been seen in individuals with focal hand dystonia, blepharospasm, and cervical dystonia in several investigations.
The shortest duration needed for two tactile stimuli applied to the same body area to be temporally distinguished from one another is known as the somatosensory temporal discrimination threshold (STDT), which gauges how quickly sensory information is processed.
To evaluate putaminal volumes in relatives with aberrant and normal TDTs, Bradley et al. looked at the STDT in 35 adult-onset primary and 42 unaffected first-degree relatives using voxel-based morphometry (VBM). STDT was abnormal in thirty-two patients and twenty-two relatives who were not affected.
Grey matter volume in the putamen of thirteen unaffected members with aberrant STDTs and twenty unaffected members with normal STDTs was bilaterally enhanced, as demonstrated by VBM.
Accordingly, peripheral sensory abnormalities as seen in GOT and TVR tests as well as somatosensory processing are involved in sensory dysfunction in dystonia.
Dysfunctional connection between the main somatosensory region (S1) and subcortical structures (thalamus, basal ganglia, and superior colliculus) results from abnormalities in the processing of sensory information.
The basal ganglia act as a gatekeeper for sensory inputs, while the thalamus is crucial in integrating sensory inputs with the basal ganglia and cerebellar outputs.
Therefore, abnormal sensorimotor integration is central to the pathophysiology of dystonia.
Abnormal Synaptic Plasticity
Both short- and long-term alterations in the cortical-subcortical circuits are brought about by the aberrant sensory feedback and the lack of inhibition.
To emphasize the neuroplasticity/learning nature of dystonia, Byl et al. conducted tests on monkeys to assess the function of repetitive strain injuries generating focal dystonia.
They proposed that neuronal plasticity caused the sensory feedback in repeated strain injuries to deteriorate, which had a significant impact on the major motor region responsible for dystonia.
This phenomenon—excessive amplitude of plasticity responses and unspecific topography of the spread, or abnormal spread—has also been shown in research involving humans and is a key component of the dystonia underlying mechanism.
Long-term depression (LTD) and long-term potentiation (LTP) are known to affect receptive sensory fields and motor representations in the brain, and they are important for cortical plasticity.
TMS studies that employ paired associative stimulation (PAS), which pairs TMS with low-frequency median nerve stimulation, examine synaptic alterations in the motor cortex.
In a case-control study including patients with writer’s cramp, TMS was administered to the contralateral brain 21.5 ms or 10 ms following peripheral nerve stimulation (PAS) on the dominant hemisphere using electrical stimulation of the ulnar or median nerve.
The adductor digiti minimi (ADM) and abductor pollicis brevis (APB) muscles were used to test the motor response.
In the case of homologous peripheral regions for the afferent PAS component, the amplitude of the motor potentials measured after 21.5 ms rose in the control subjects.
However, in writers’ cramp patients, the amplitudes of the APB and ADM motor unit potentials were raised by either the median or ulnar PAS at 21.5 ms.
There was a greater number of instances, they began sooner, and they persisted longer. The patients’ aberrant dynamic responses to PAS protocols, the scientists concluded, suggested neural plasticity of various polarity, consistent with LTD and LTP.
According to this, Quartarone et al.’s PAS tests demonstrated that individuals with dystonia had a lack of topographical specificity of PAS with facilitation in both the median and ulnar innervated muscles, as well as a greater and longer-lasting facilitatory rise in corticospinal excitability.
This experiment serves as more evidence that anomalies in the spatial features of associative plasticity might be linked to co-contraction or overflow events. Therefore, an abnormally strong link between sensory inputs and motor outputs may be the origin of dystonia.
But unlike primary dystonia, a new study has shown that lower somatosensory inhibition and increased cortical plasticity might not be necessary for secondary dystonia to manifest clinically.
Mirror Movements in Dystonia
In people with dystonia, mirror motions are an indication of motor overflow.
It is described as the onset of aberrant posture in the afflicted limb brought on by the contralateral, undamaged limb performing a particular function.
This makes it easier to distinguish between compensatory motions made unintentionally to lessen a handicap and actual dystonic movements.
Functional neuroimaging and electrophysiological investigations have shown interhemispheric inhibition, and mirror movement loss has been linked to its loss. Merello and associates.
Applying function MRI, Merello et al. showed that when a patient with writer’s cramp and mirror motions wrote with the afflicted hand, the posterior parietal cortex, putamen, and inferior frontal gyrus were activated both ipsilaterally and contralaterally.
Nevertheless, increased activity was observed ipsilaterally when writing with the unaffected hand, indicating attenuation of the inhibitory intracortical circuits and transcallosal inhibition.
Using TMS, Beck et al. demonstrated that individuals lacking mirror motions did not exhibit interhemispheric inhibition of the dystonic motor cortex during the premotor phase.
Dystonia as a Network Disorder
The earlier stated idea that dystonia is solely a basal ganglia condition is contradicted by the anatomical correlations and the processes outlined above.
The role of the pallidothalamocortical and cerebellothalamocortical cortical-subcortical circuits in the pathogenesis of dystonia is becoming more well-acknowledged.
The localized onset and slow segmental or generalized spread of the anomaly is also explained by the network idea.
Previous descriptions of the basal ganglia and their thalamocortical connections via the hyper-direct route and direct and indirect pathways from the cortex to the subthalamic nucleus are well known.
Movement is facilitated by the direct pathway and hindered by the indirect pathway. By demonstrating the activation of the direct route in focal dystonias, Simonyan et al.
The aberrant striato-thalamo-cortical excitability in dystonia is further supported by the considerably higher availability of D1 receptors in the putamen of individuals with writer’s cramps and laryngeal dystonia.
The beneficial effects of deep brain stimulation (DBS) of the internal portion of the globus pallidus in dystonia provide another evidence pointing to the network mechanism.
Improvements in sensorimotor processing and symptom relief are the outcome of the abnormal bursts and oscillations in the network being inhibited by the DBS-induced alterations in neural patterns.
Argyelan et al. used probabilistic tractography and magnetic diffusion tensor imaging to examine the cerebellar connections in dystonia in carriers of the DYT1 and DYT 6 mutations.
They demonstrated compromised cerebellothalamocortical fiber tract integrity in carriers of both manifesting and non-manifesting mutations, with the former group exhibiting more abnormalities.
The deficiency of cortical inhibition in dystonia may be caused by anomalies in the cerebellar outflow, according to the authors’ conclusion.
Both the cerebellum and the basal ganglia project to the SMA and pre-SMA, although the basal ganglia pallidal neurons contribute more.
This was demonstrated by Akkal et al. in monkeys via retrograde transneuronal transfer of the neurotropic virus. According to the network, dystonia is thus not only caused by physical malfunction in the thalamus or basal ganglia but also by a functional disruption of the pathways that were previously mentioned and are crucial in the pathophysiology of dystonia.
As a result, new experimental data has changed our understanding of dystonia from a psychiatric diagnostic to an illness marked by changes at several brain nodes.
Although the pathophysiology of dystonia is largely influenced by various areas of the motor circuit, it is primarily caused by the basal ganglia.
Improper sensory input influences the anomalies in the networks including the basal ganglia, cerebellum, thalamus, and cortex.
These abnormalities are crucial in improper sensorimotor integration that results in dystonia.
Paratonia
The abnormal motor activities that precede voluntary movement execution are known as higher-order motor disorders. These include disinhibition diseases, motor intention disorders, syndromes of the alien limb, and mirror motions.
Mirror motions in the context of movement disorders have been covered under the section on dystonia. Although well-documented cortical phenomena in parkinsonism, alien limb phenomena, and motor intention problems are outside the purview of this discussion on disorders of tone.
But since botulinum toxin is known to alleviate the involuntary resistance associated with paratonia, we would want to quickly address this disinhibition condition here: paratonia. Paratonia was initially defined as elevated muscle tone in reaction to passive movement, proportionate to the strength of the applied stimulus.
This was first reported by Friedlander in 1828 and then by Dupre in 1910. The movement’s speed determines the resistance level. In the early stages, it may be facilitatory, with the patient voluntarily supporting passive motions; as the disease advances, it may become oppositional, as resistance rises with more movements.
Paratonia differs from spasticity in that it is not velocity dependent, unlike rigidity, and it may be triggered in any direction of movement. It also lacks a catch.
Pathophysiology of Paratonia
Beversdorf et al. showed that facilitatory paratonia was an echopraxia-like condition in which the participants imitated the motions of the examiner.
They concluded that frontal lobe impairment is the cause of this type of faulty response inhibition.
Defective response inhibition has been associated with orbitofrontal injury and frontal-subcortical dysfunction.
Two circuits that converge on the primary motor cortex mediate goal-directed movement: the parietal-premotor-primary motor area circuit and the pre-supplementary motor area (Pre-SMA)–primary motor circuit.
The former regulates internally generated voluntary motor actions by receiving signals from the basal ganglia and prefrontal cortex.
The latter circuit is engaged in activities that are focused on objects, such as gripping or paying attention to spoken or visual stimuli. Because the two circuits are generally balanced, goal-directed tasks may be completed with ease.
The parieto-premotor circuit is ordinarily inhibited by the pre-SMA, and frontal lobe dysfunction results in a disruption of this circuit.
As a result, the person exhibits a disinhibited behavior and becomes dependent on tactile and visual stimuli to propel their motor motions with impaired inhibition, which exacerbates facilitatory paratonia.
There is also a theory that suggests a peripheral mechanism plays a role in the development of paratonia.
Growing older affects the reciprocal inhibition at the spinal level, which results in the co-contraction of agonist and antagonist and is interpreted as a rise in resistance to movement.
However, co-contraction of the opposing set of muscles in paratonia was not seen in the electromyographic examination of paratonia patients.
Another peripheral metabolic alteration that may heighten tissue resistance in individuals suffering from dementia and paratonia was suggested by Drenth et al.
Patients with paratonia showed considerably higher levels of advanced glycation end products (AGEs), which were directly correlated with the degree of paratonia as determined by skin autofluorescence measurement.
AGEs degrade skeletal muscle function, increase tissue stiffness by creating cross-links in muscle collagen, and may contribute to the pathophysiology of paratonia.
Conclusions
Complex interactions between supraspinal and spinal processes regulate tone; disturbances cause stiffness and spasticity.
However, dystonia and paratonia, conditions brought on by aberrant sensorimotor integration, disinhibition in the brain and spinal cord, and network failure, can exhibit altered tone.
It is critical from a pathophysiological and treatment standpoint to distinguish between these four illnesses in a hypertonia clinical setting.
FAQ
Abnormally high muscle tone state. The following conditions result in aberrant muscular function: dystonia, myotonia, atonia, hypotonia, and hypertonia. Every one of these ailments has unique traits and signs. There are typically treatments available.
A child’s hypertonia is marked by an unusual increase in muscular tone. While the body may move freely and defy gravity, normal muscle tones allow for this. A person with well-defined muscles may stand, sit, and move about with better posture and efficiency.
If a person has a low tone or too little tone, their muscle tone is abnormal. “Floppier” than normal muscular tone is low tone. If a person’s muscles are too toned, they are also considered abnormally toned. Another name for a condition, when there is excessive muscular tone, is high tone or spasticity.
Maintaining muscle tone, or the partial contraction of a muscle, is crucial for producing reflexes, preserving balance and posture, and regulating the appropriate operation of other organ systems. The sensory muscle spindle, which gauges muscle strain, regulates tone.
Casting or bracing: lessens muscular tightness and stops uncontrollably occurring spasms. Oral drugs: oral drugs, such as physical or occupational therapy, are used in conjunction with other therapies or medications. Oral drugs are only taken when symptoms make it difficult to go to sleep or function daily.
A prolonged muscular contraction that results in abnormal muscle stiffness is called spasticity. It is a sign of harm to the brain, spinal cord, or motor nerves and is seen in people with neurological diseases like cerebral palsy (CP) and Multiple sclerosis.
When we sit and stand, our ability to maintain our body’s upright posture is aided by our muscular tone. Our ability to move with control, speed, and volume is also influenced by our muscle tone.
A toned physique will give you more energy, stamina, and flexibility. It will also lower your chance of contracting certain illnesses, like diabetes and heart disease.
In people with neurological problems, muscle vibration has been utilized as a treatment to lessen stiffness and muscular tone. It is believed that muscular vibrations in the antagonistic muscle enhance both inhibitory neural activity and corticospinal excitability.
muscular injuries or overuse, such as sprains or strains, cramps, or tendinitis, are among the causes of muscular diseases. an inherited illness like muscular dystrophy.