Popliteal Artery Entrapment Syndrome
Popliteal Artery Entrapment Syndrome (PAES) is a rare vascular condition that involves compression or entrapment of the popliteal artery, which is the major artery located behind the knee.
Table of Contents
Introduction
An unusual disorder that affects the main artery behind the knee. The name of that artery is a popliteal artery. The calf muscle is either enlarged or positioned incorrectly in this disease. The artery is compressed by the muscle. The artery becomes clogged, which impedes blood flow to the foot and lower leg.
The majority of cases of popliteal artery entrapment syndrome occur in athletes.
When the surrounding popliteal fossa myofascial tissues crush the popliteal artery, an unusual condition known as popliteal artery entrapment syndrome (PAES) results. Claudication and chronic leg ischemia are the outcomes of this. Young athletes are more likely than older athletes to experience this ailment.
Elderly people are more likely to be diagnosed with peripheral artery disease and related atherosclerosis when they have comparable symptoms. Patients with PAES typically arrive with intermittent calf and foot pain that is eased by rest and is linked to exercise.
Combining a physical examination, medical history, and advanced imaging techniques like magnetic resonance angiography, computed tomography, or duplex ultrasonography can help identify PAES.
With a usually good prognosis, management options include open surgical decompression or no intervention at all. Untreated PAES can lead to complications such as distal arterial thromboembolism, aneurysm formation, stenotic artery degeneration, and total popliteal artery blockage.
What is Popliteal Artery Entrapment Syndrome (PAES)?
Some adolescent sportsmen suffer from a rare vascular illness called popliteal artery entrapment syndrome (PAES), which affects the legs. The popliteal artery, which is the primary artery that connects your thigh to your calf, is compressed by the muscle behind your knee when you have this syndrome.
The term “popliteal artery entrapment syndrome” describes the symptomatic compression or occlusion of the popliteal artery as a result of the artery’s developmentally abnormal positioning about surrounding structures, such as the popliteus or fibrous bands, or less frequently, the medial head of the gastrocnemius.
Compression is caused by the gastrocnemius muscle’s connection to the thigh bone. Your artery is compressed when your gastrocnemius muscle contracts during plantar flexion, or pushing down on your foot.
Your arteries spasm as a result of recurrent compression during activity. Blood flow is decreased as a result. Your muscles and nerves accumulate lactic acid and carbon dioxide as a result of the decreased blood flow, which causes heaviness, achiness, fatigue, and occasionally numbness in your foot and leg.
Usually, three to five minutes after the exercise is stopped, the symptoms get better. In the absence of therapy, the spasm usually happens more frequently and lasts longer. It takes longer to heal and symptoms appear after a shorter distance.
When you exercise, this restricts the blood supply to your lower leg. Recovery from surgery takes four to six weeks, and success rates are high.
Epidemiology
Up to 3–3.5% of people may have anatomic abnormalities, which are typically bilateral (presenting in about 2/3 of cases). The genuine clinical syndrome is much less prevalent, and the majority of people have no symptoms at all. Well-developed muscles are associated with a higher likelihood of symptoms, which likely explains why young athletes (~60% of those under 30 years old) with a male-to-female ratio of 15:13 are most commonly affected by the syndrome.
Popliteal artery entrapment syndrome (PAES) is thought to affect 0.16% of the general population. This disparity in occurrence might be exaggerated because research generally shows that men engage in greater physical activity than women or because military hospitals, which treat primarily male patients, provide a substantial percentage of the statistics. There is a higher risk for those who run and play soccer, football, basketball, or rugby.
Congenital factors also raise the risk of PAES in newborns and early children. The medial head of the gastrocnemius migrates superiorly and medially throughout embryonic development. In addition to accounting for the infrequent cases of entrapment brought on by the popliteus muscle, this migration may result in anatomical anomalies such as uneven popliteal artery placement. The anatomical anomaly leading to PAES is present in less than 3% of the population at birth, and most of those individuals never experience any symptoms. About 30 percent of patients had a bilateral presentation of PAES.
History
Medical student Anderson Stuart initially reported the illness in a 64-year-old man in 1879. Hamming and Vink initially reported on the treatment of a 12-year-old patient’s PAES in 1959. The patient had a concurrent endarterectomy of the popliteal artery and myotomy of the medial head of the gastrocnemius muscle.
They then published four more cases and stated that 40% of patients with claudication who were under 30 years old had this pathology. The reduced distal pulses seen in patients with this condition, when pushed to dorsiflex or plantar fascicles, were initially noted by Servello.
Among 20,000 Greek soldiers, Bouhoutsos and Daskalakis (1981) identified 45 occurrences of this condition. The rising number of reports of popliteal artery entrapment over the past few decades strongly suggests that the syndrome is becoming more widely recognized.
What leads to popliteal artery entrapment syndrome?
Two primary categories of compression are present:
- Anatomic compression: This kind of compression makes up around 10% of instances and appears to be more prevalent in those who were assigned to the male gender at birth. About 70% of cases only involve one leg.
- Non-anatomic compression, also known as functional or physiologic compression: Individuals allocated to the female gender at birth are more likely to experience this kind of compression. In about 90% of instances, it affects both legs.
Anatomical compression:
This occurs as a result of a gastrocnemius muscle segment passing over or across your artery. Your artery may be harmed by a tendinous band in your muscle. This results in:
- An arterial sore or ulcer.
- Clot formation
- Eventual blockage or closure of your artery or arteries downstream.
- The position of the muscle concerning your artery can be divided into four categories.
Functional, physiologic, or non-anatomic compression:
All of your muscles are where they should be, although they are usually inserted on the inside notch of your thigh bone at the knee or higher up your thigh bone. As a result, your muscle is pulled within, compressing your artery with plantar flexion.
Another area of compression is the popliteus muscle, which is a muscle that lies beneath your artery. Researchers have not found any link between physiologic compression and arterial damage
Who is affected by popliteal artery entrapment syndrome?
Athletes between the ages of 15 and 25 are most likely to get PAES, especially those who participate in running-related activities and sports. Among them are:
- Track.
- Cross country.
- Soccer.
- Lacrosse.
- Field hockey.
Less than 1% of people are thought to have PAES. The exact number of people who suffer from this illness is hard to determine.
Pathology
Localized premature arteriosclerosis, thrombus development, and persistent vascular microtrauma are all possible outcomes of arterial compression. This may cause ischemia distal to the area. Aneurysm development, or post-stenotic ectasia, can result from stenosis and turbulent flow.
Usually, five anatomical entrapment types are explained:
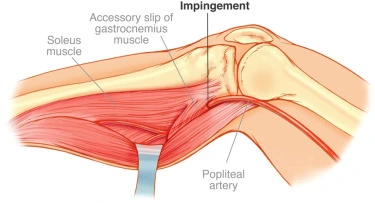
- Type I: The popliteal artery circumnavigates the medial head of the gastrocnemius with an abnormal medial route.
- Type II: The artery is not displaced. The artery penetrates medially and beneath the muscle, but the medial head of the gastrocnemius inserts more laterally than typical.
- Type III: The artery is encircled by an auxiliary slip of the gastrocnemius medial head.
- Type IV: Artery blocked by popliteus or fibrous band deep into popliteal fossa
- Type V: Popliteal artery and vein entrapment
The Heidelburg classification system is an additional classification technique.
- Type I: The path of the popliteal artery is unusual.
- Type II: There is an abnormal muscle insertion
- Type III: Both conditions are present.
Causes
An uneven muscle in the calf, most commonly the gastrocnemius muscle, is the cause of popliteal artery entrapment syndrome (PAES).
The disease may manifest from birth or emerge at a later age. During pregnancy, the calf muscle or surrounding artery starts in the incorrect location and remains after birth. Calves born to individuals with the condition later in life are larger than average.
The changes in the calf muscle press on the main artery located behind the knee. As a result, the blood flow to the lower leg is reduced. A decrease in blood flow is the reason for pain and cramping in the back of the lower leg during times of exertion.
Symptoms
The primary symptom of popliteal artery entrapment syndrome, or PAES, is lower leg pain or back cramps. The back part of the lower leg is referred to as the “calf.”Exercise is the source of the pain, which goes away when you rest. Additional signs and symptoms could include:
- Chills following physical activity.
- Sensation in the vicinity of the calf.
- A deep vein thrombosis is a blood clot that occurs in the lower leg.
- Adults under the age of 40 are typically impacted.
- Aching pain.
- Tiredness.
- Heaviness.
- Cramping.
- Numbness.
- Burning or tingling
- During intense exercise, one or both calves may have claudication, which is an excruciating ache that usually goes away after five to ten minutes of rest.
- Swelling around the calf
- Skin tone variations near the calf muscle
- Foot numbness, tingling, and discoloration
- Discomfort during repose in the lower limbs and feet (in individuals with advanced PAES)
Most symptoms fade away after three to five minutes of rest. In the absence of treatment, the symptoms typically worsen with time and become more confined.
Risk factors
The disorder known as popliteal artery entrapment syndrome, or PAES, is rare. The risk associated with the condition is increased by the following factors:
- Younger age: The disease more frequently affects people in their late teens or early 20s. For people over 40, diagnoses are rare.
- Male: Although everyone can be impacted by PAES, young males are much more prone to do so.
- Physically rigorous sports activities. Runners, bikers, and athletes who try to build quickly with weight training or severe circuit training are the most vulnerable.
Complications
Prolonged pressure can cause the popliteal artery to constrict. Arterial stenosis is the term for it. One of the tiniest tasks that might cause pain and cramps is walking.
Leg muscles and nerves might suffer injury in extreme circumstances or if treatment is not received. There can be blood clots in the lower leg. It is important to look into arterial ballooning or bulging when older athletes have the symptoms of popliteal artery entrapment syndrome. This is known as a popliteal aneurysm. It’s what senior guys do.
Diagnosis
In order to determine the diagnosis of popliteal artery entrapment syndrome (PAES), the medical team will examine you and inquire about your medical history and symptoms. But diagnosing PAES might be difficult at times because most of the individuals with the disorder are young and generally healthy. A physical examination usually yields no remarkable results.
Tests for diagnosis quantify the blood flow in your foot, leg, and knee. Visualization can demonstrate:
- Typical artery.
- Your artery is being ulcerated.
- Blood clots.
- An arterial aneurysm is a dilatation of the blood vessel that is greater than 50% of its usual size.
- Arterial compression is caused by muscle.
Tests are performed to rule out the possibility of stress fractures, muscle strains, and peripheral artery disease, which is the consequence of clogged arteries, as additional causes of leg pain.
Tests could consist of the following:
- Ankle-brachial index (ABI) with exercise: The initial test used to diagnose PAES is typically the ankle-brachial index measurement. Blood pressure readings are obtained in the arms and legs both during and after walking on a treadmill. Ankle pressure is divided by arm pressure to get the ABI. It is expected that the blood pressure in the legs will be higher than in the arms. Leg blood pressure after exercise decreases to less than 90% of the arm blood pressure when jogging creates an artery spasm. However, when you exercise and have PAES, your ankle pressure decreases.
- Popliteal artery duplex ultrasonography with plantar flexion: High-frequency sound waves are used in duplex ultrasonography of the calf to visualize the speed at which blood flows through the leg arteries. You can take this test either before or after working out. Your calf muscles will be used if you are requested to flex your foot up and down.
- MRA, or magnetic resonance imaging, determines whether the artery is being trapped by the calf muscle. Additionally, it can determine the extent of popliteal artery narrowing. During this exam, you can be asked to press or flex your foot against a board. This makes your lower leg’s blood flow more visible.
- CT angiography: The leg muscle causing the arterial entrapment is clearly seen on CT angiography. This kind of CT scan looks at the arteries in your legs when they are at rest and in plantar flexion. It does this by using dye to detect compression of the muscles. Similar to MRA, there’s a chance this test will require you to move your foot.
- Catheter-based angiography: Real-time visualization of the blood flow to and from the lower leg is possible with catheter-based angiography. It is carried out if additional, less invasive imaging tests fail to provide a clear diagnosis.
- Ultrasound: May demonstrate artery compression brought on by dorsiflexion and plantar flexion. Doppler could show a rise in peak velocity.
- Angiography (DSA): Ankle plantarflexion during lower limb angiography typically shows medial deviation/compression of the popliteal artery. The acute presentation shows occlusion of the arteries by thrombus. Collateral vessels are typically found. A vessel’s even the slightest abnormality can reveal a degree of entrapment.
Healthcare professionals who specialize in vascular problems are the most qualified to diagnose PAES. They will perform a physical examination, which will involve monitoring your popliteal artery and your foot pulse. When you push your foot up and down against resistance, they might also check for variations in your pulse.
Your healthcare provider, if you have popliteal artery entrapment syndrome:
- May be able to sense your heartbeat when you’re sleeping.
- May find it more difficult to feel your pulses when you flex or extend your foot or when you exercise.
Treatment
Your gastrocnemius and popliteus muscles may be surgically removed in little pieces by your healthcare provider. By doing this, the compression on your artery is removed, and your leg’s blood flow returns to normal.
Popliteal artery entrapment syndrome is best treated surgically because most patients have satisfactory outcomes. Following the procedure, over 90% of patients reported significant symptom relief.
Surgery could be recommended if popliteal artery entrapment syndrome (PAES) symptoms substantially interfere with daily or athletic activities. The only method to repair the calf muscle and release the trapped artery is surgery.
Under general anaesthesia, surgery is performed in a hospital or medical facility. The inner calf is incised by the surgeon either in the rear of the knee or directly below it during the procedure. To allow the artery greater space, this relaxes the calf muscle. The artery is no longer compressed by the calf muscle.
The procedure for popliteal artery entrapment syndrome takes approximately sixty minutes. You will usually need to spend one day in the hospital.
You may require an arterial bypass surgery if the artery constriction is severe and you’ve had the issue for a long time.
The function of the leg is typically unaffected by surgery performed to release the calf muscle and artery. Early diagnosis and treatment should result in a full recovery and the disappearance of symptoms.
Botulinum toxin Injections are the only non-surgical treatment available for the functional kind of PAES. Your healthcare professional injects Dysport or Botox into the compressing muscle under the supervision of a CT scan or ultrasound. In an attempt to get the symptomatic muscle to shrink permanently, this momentarily paralyzes it.
But this is merely a three- to six-month-long effect. The symptoms will recur if the muscle doesn’t shrink. Less than 60% of patients report success with this one-year treatment.
Prevention for Popliteal Artery Entrapment Syndrome (PAES):
- Avoid repetitive motions, heavy lifting, extended sitting or standing, and intense exercise that could strain the popliteal artery.
- If you must sit for extended periods, make sure you get up often to walk about and extend your legs.
- If you are overweight, try to reduce your weight with exercise and a healthy diet.
- Wear loose-fitting garments and footwear to prevent your legs’ blood vessels from being constricted.
- If you feel any pain or discomfort in your legs, particularly during or after activity, get medical help immediately.
- Make an appointment for routine check-ups with your physician, particularly if PAES or other vascular diseases run in your family.
Differential Diagnosis
- Chronic exertional compartment syndrome: Prolonged discomfort and oedema in the impacted muscle due to an increase in intramuscular pressure during physical activity.
- Unresolved muscle strain: A tear or impairment to the muscle or the tendons that adhere to it.
- Medial tibial stress syndrome: Running or other sports-related activities can cause pain over the tibia, or shin bone.
- Fibular and tibial stress fracture: Many athletes, particularly runners, as well as non-athletes who abruptly increase their level of exercise, can sustain a non-displaced microscopic fracture of the fibular and tibia.
- Fascial defects: pain and oedema are caused when a muscle protrudes through the surrounding fascia.
- Sciatic nerve entrapment syndrome: entrapment of the sciatic nerve by muscles or other tissues.
- Vascular claudication (secondary to atherosclerosis): Secondary to atherosclerosis, vascular claudication is characterized by a restriction of arterial flow that results in muscle ischemia and buttock and calf pain. more prevalent in older people who have cardiovascular risk factors.
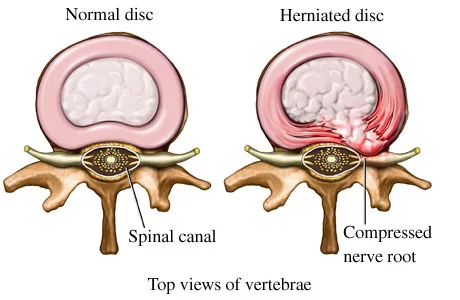
- Lumbar disc herniation: a bulging or herniated disc in the lower back that can cause discomfort to radiate from the buttock into the leg and occasionally the foot.
Conclusion
When making a differential diagnosis for exertional lower leg pain in athletes and other physically active people, popliteal artery entrapment should be taken into account. Physical examination results might be normal; however, areas of functional or anatomic compression might be defined, and clinical findings can be correlated with the proper interpretation of imaging investigations.
Bilateral testing is advised, and noninvasive initial testing is preferred. In circumstances where surgery is indicated, it is crucial to act before artery wall damage or other vascular problems arise. Fortunately, case studies and series in the athletic community to date show excellent results, including a return to activities and the absence of notable vascular sequelae.
Further long-term outcome research in the symptomatic athlete population with popliteal artery entrapment will help to further improve evidence-based recommendations.
FAQs
The first line of treatment should be nonsurgical, consisting of physical therapy and stretching of the gastrocnemius complex.
During intense exercise, one or both calves may have claudication, which is an excruciating ache that usually goes away after five to ten minutes of rest. swelling around the calf. skin tone variations near the calf muscle. Foot numbness, tingling, and discolouration.
When an artery is occluded, tests using magnetic resonance angiography (MRA) or computed tomography (CT) angiography can confirm the diagnosis, but they do not permit provocative testing.
Back and outer knee discomfort is common in people with popliteal problems. When bending the knee against resistance or fully straightening it, discomfort is frequently experienced. Running, climbing stairs, and walking downhill all typically cause more pain.
The majority of these wounds recover without any problems or complications. After completing a functional assessment, the patient can resume full physical activity without limitation. The recovery period may take anywhere from three to sixteen weeks.