Fibula Fracture
Table of Contents
Introduction
A fibula fracture refers to the breakage or damage to the fibula, which is one of the two long bones located in the lower leg alongside the tibia. It is a common injury accounting for about 10-15% of all adult fractures.
The fibula, also known as the calf bone, is a long thin bone located on the outer side of the lower leg. It runs parallel to the tibia or shin bone, the larger bone in the lower leg. The fibula plays an important role in stabilizing the ankle and knee joints.
Anatomy of the Fibula
The fibula is located on the lateral or outer aspect of the lower leg next to the tibia bone. It is a long, slender bone providing attachment points for various muscles and lending stability to joints above and below.
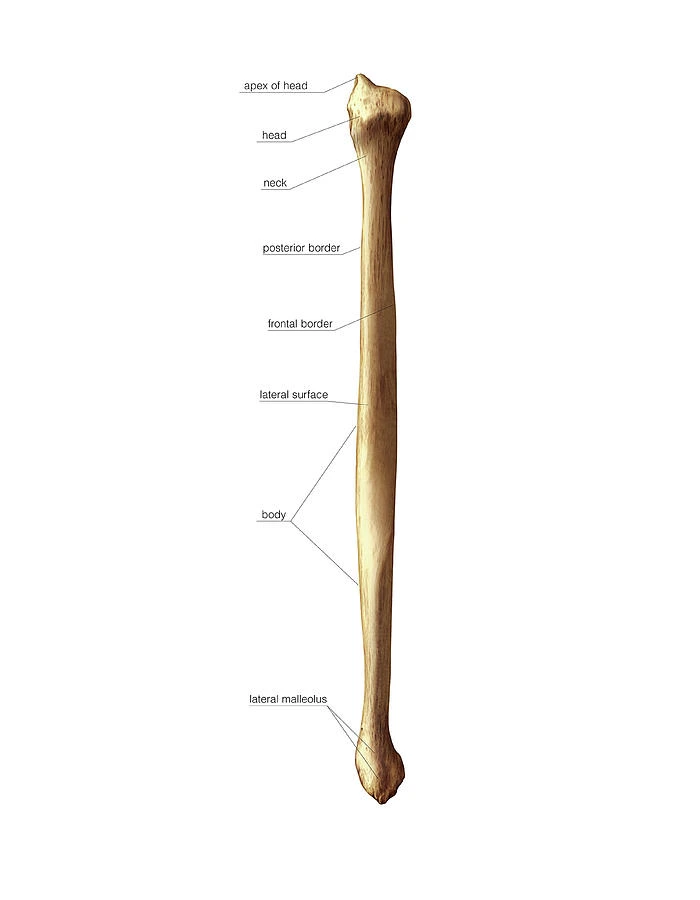
The fibular head comprises the expanded proximal end reaching the tibia at the knee joint. It articulates with the tibia and supports the lateral meniscus.
The fibular shaft is skinny, making up most of the bone’s length. It has a body and three borders – the anterior, interosseous, and posterior borders. Numerous muscle origins attach along the entirety of the shaft including:
- Anteriorly – extensor digitorum longus
- Posteriorly – soleus, flexor hallucis longus
- Laterally – peroneus longus and brevis
The interosseous border forms a ridge for the attachment of the long, powerful interosseous membrane binding the parallel tibia and fibula.
The distal end continues into a wider pyramid-shaped lateral malleolus forming the outer tip of the ankle joint. It projects farther than the medial tibial malleolus on the other side. The inferior transverse ligament crosses under the malleoli making a socket for the talus bone to form the ankle joint.
On the medial malleolus is a smooth facet over which a tendon glides during certain foot movements. Further continuing posteriorly and superiorly are two additional tubercles for ligament attachments. Finally, the roughly triangular subcutaneous surface lacks muscle attachments and is visible externally underneath the skin.
The vascular supply enters proximally, segmentally, and via the distal syndesmotic arteries. These provide circulation to the fibula which lacks a medullary cavity and consists mostly of dense cortical bone.
Mechanism of Injury
Depending on the energy involved, the mechanisms of injury for tibia-fibula fractures vary greatly and fall into two primary categories:
Low-energy: these include falls from a height and sports-related injuries. Under these conditions, the fibula is frequently affected by strain or overuse, especially in activities involving repetitive motion or abrupt spikes in activity. Stress fractures or small fibula breaks are common in runners and athletes.
High energy: These are linked to more serious trauma such as car crashes, vehicle strikes on pedestrians, or gunshot wounds. In these situations, the fibula is subjected to abrupt, powerful impacts that may result in more serious fractures. These fractures are frequently complicated, and they could also involve other soft tissue and bone damage.”
Patients with tibia fractures may complain of discomfort, swelling, and difficulty walking. They may also describe a history of direct trauma (such as axial loading from a motor vehicle accident) or indirect trauma (such as twisting).
Causes and Risk Factors
A fibula fracture often occurs due to a direct blow or twisting injury to the lower leg. Common causes include:
- Falls – landing abruptly on the foot with the ankle bent inwards
- Sports injuries – tackles or collisions in soccer, rugby, hockey
- Motor vehicle accidents
- Twisting the ankle when stepping on an uneven surface
- Repetitive stress on the bone from overuse
- Certain factors can increase one’s risk of getting a broken fibula:
- Osteoporosis – weakened bones that break easily
- Previous injuries such as an ankle sprain
- High-intensity sports
- Poor physical conditioning, muscle weakness
- Improper footwear like high heels or slippery shoes
- Some medical conditions like bone cysts or tumors can also weaken the fibula and make it more prone to fractures.
Statistics and Incidence
It is estimated that about 10-15% of all adult fractures are fibula fractures. The annual incidence rate is 9.7 per 10,000 person-years. Men under the age of 45 are at a slightly higher risk due to participation in contact sports and high-risk activities.
After the age of 50, women are more commonly affected due to postmenopausal osteoporosis. Lateral malleolus fractures comprising the distal end account for over 60% of all fibula breaks.
Types of Fibula Fracture
There are five main types of fibula fracture depending on the location and pattern of break:
Fibular Head Fracture
The fibular head fracture occurs at the proximal end of the fibula where it articulates with the tibia at the knee joint. This type comprises 1-2% of all lower limb fractures. It commonly results from a fall directly onto the bent knee or a blow to the knee, transmitting excessive force up the leg.
Signs and Symptoms:
- Pain, swelling, and bruising over the upper outer calf
- Tenderness at the fibular head
- Difficulty bearing weight on the limb
Treatment:
- Casting or bracing to immobilize the fracture
- Surgical fixation using screws and plates
- Partial removal of the fibular head if severe comminution
Fibular Shaft Fracture
The diaphyseal shaft refers to the long, narrow body of the fibula. About 4-5% of fractures occur along this portion, usually due to sudden rotational movements or a direct blow. Transverse, oblique, or spiral fractures may result.
Signs and Symptoms:
- Pain over the lower outer leg
- Inability to bear weight
- Visible swelling
Treatment:
- Cast immobilization for 4-8 weeks
- Surgical fixation for displaced fractures to realign the limb
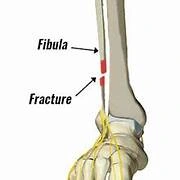
Lateral Malleolus Fracture
This is the most common type, accounting for over 60% of all fibula fractures. It occurs at the outer projection of the ankle joint. Twisting injuries like an ankle sprain or losing one’s balance can cause avulsion of this distal portion.
Signs and Symptoms:
- Ankle pain, swelling, bruising
- Tenderness over lateral malleolus
- Inability to bear weight
Treatment:
- Below-knee cast for 6 weeks in simple fractures
- Open reduction and internal fixation surgery for displaced joints
Avulsion Fracture
Forceful contraction of attached muscles or ligaments pulls off a fragment of bone at their insertion site. The peroneus longus tendon commonly avulses parts of the distal fibula to which it adheres.
Signs and Symptoms:
- Ankle pain when pushing off with the toes
- Foot and ankle swelling
- Difficulty bearing weight through the heel
Treatment:
- Immobilization for bone fragment reattachment
- Screw fixation of larger detached pieces
Stress Fracture
Repetitive overloading causes tiny cracks along areas of muscle attachment, commonly the distal fibula or tibiofibular joints. Gradual ankle soreness presents in athletes, runners, and military recruits undergoing intensive training.
Signs and Symptoms:
- Diffuse ankle ache worsening with activity
- Relieved by rest
- Potential swelling
Treatment:
- Relative limb rest with a walking boot for 4-8 weeks
- Muscle relaxants and anti-inflammatory medication
Diagnosis and Testing
An orthopedic doctor elicits a history of the injury pattern and completes a physical examination of the entire lower limb joint to diagnose a fibula fracture. Diagnostic tests that aid confirmation include:
- Radiographs: X-rays taken from at least two angles detect over 95% of fractures. It helps classify the break pattern – transverse, oblique, spiral, or comminuted.
- CT scan: Provides excellent detail of the bone anatomy and fracture configuration. Useful for complex breaks and preoperative planning.
- MRI scan: Identifies bone bruises, ligament, and tendon injuries associated with the fracture. Also, diagnoses of subtle stress fractures are not seen on regular X-rays.
- Bone scan: Radioactive tracer injected intravenously gets absorbed at the fracture site indicating increased bone turnover during the early healing phase.
The results of medical imaging indicate whether the fracture is displaced or non-displaced, closed or open, along with the precise size and orientation of the break. This determines the ideal treatment plan for proper healing.
Differential Diagnosis
It is important to distinguish a fibular fracture from other disorders that may present with similar symptoms to get an accurate diagnosis.
A critical stage in this procedure is the differential diagnosis, which assists in ruling out further possible explanations for the patient’s symptoms:
- Acute Compartment Syndrome
- Knee Fracture
- Soft Tissue Knee Injury
- Ankle Fracture
- Ankle Injury
- Child Abuse
- Tibia Fracture
- Peripheral Vascular Injuries
- Pediatric Limp
Treatment
The main aims during the management of a fibula fracture are:
- Restore normal limb alignment and anatomy
- Immobilize and stabilize the fracture fragments
- Ensure adequate bone healing in a good position
- Prevent complications like non-union, delayed union, or malunion
- Restore pain-free weight-bearing and joint movements
The kind, location, and severity of the fracture all influence the course of treatment. Fractures are commonly classified as closed (skin intact) or open (skin fractured).
A physical therapist can teach you how to walk without bearing weight on the fractured leg. After your doctor aligns your bones, they will place your leg in a cast or splint, either closed or open, to restrict movement and allow the fracture to heal. You may also be given crutches.
Closed (simple) fracture treatment
A splint or cast that restricts movement is usually all that is required for closed fractures unless other parts of the leg are also affected. If extra treatment is necessary to realign your bones, your doctor may suggest the following:
- Closed reduction: A broken bone is realigned by your doctor without requiring skin incisions.
- Open reduction: When a bone breaks more than twice, your doctor will perform invasive surgery known as an open reduction.
- Nonunion: When the ends of a fractured bone do not heal together, nonunion can be surgical or noninvasive. Your doctor will typically utilize electrical and magnetic stimulation devices in addition to bone grafting when surgery is not necessary.
Open (compound) fracture treatment
If you have an open fracture, get emergency medical assistance. Rest, ice, compression, and elevation (RICE) should be followed while you wait for aid. Open fractures require surgery since there may be other problems, such as skin loss and artery damage.
Your doctor will concentrate on the following:
- Having imaging tests to determine what kind of surgery is necessary
- Cleaning the wound to prevent contamination and infection
- Before surgery, the wound must be stabilized to maintain the bones in place
- Assessing whether antibiotics are necessary to prevent infection
Your doctor may use either internal or external methods to fix your fracture during surgery. This is usually done until your condition is ready for internal fixations. Internal fixations involve placing metal implants inside the fractured bone to hold it together while it heals. External fixations, on the other hand, involve placing metal screws or pins outside the skin to hold the bones in place. Your doctor may use either internal or external methods to fix your fracture during surgery. This is usually done until your condition is ready for internal fixations.
The exact treatment is tailored to factors like fracture location, pattern of break, displacement amount, associated soft tissue injury, patient health status, and demands. The main modalities include:
Casting and Splinting
The application of a plaster cast or splint provides rigid support to immobilize the fracture for natural healing. The leg may be wrapped in a soft roll bandage followed by a molded plaster or fiberglass cast enclosing the foot, ankle, and lower calf up to the knee.
The cast holds the limb in the correct anatomical position preventing movement at the fracture site during the initial weeks after injury. Once adequate callus forms between bone ends by 6-8 weeks, the cast can be removed and gradual rehabilitation started.
Surgical Fixation
Surgery is required for widely displaced bone fragments over a 2 mm gap or more. The orthopedist repositions and stabilizes the broken ends with fixators like plates, screws, and wires. Screw fixation across a fibular shaft fracture provides superior torsional stiffness and rotational control compared to conservative treatment in a cast.
Open reduction internal fixation surgery has the advantage of early mobilization and weight-bearing once the wound heals and fixators stabilize the fracture site. However, it does carry risks such as infection, bleeding, nerve injury, and anesthesia reactions. The hardware removal may be needed after complete healing as well.
External Fixation
This technique uses a scaffold-like frame with pins that go directly into the bone above and below the fracture site. Bars and rods connect the pins to create rigidity and compression at the fracture fragments for union. It helps realign severe lower leg deformities from high-impact trauma. Soft tissue coverage, bone grafting, or flap surgery may also be combined with external fixation. Hardware removal after treatment completes rehabilitation. External fixation carries an increased infection risk.
Physiotherapy Management
Physiotherapy and rehabilitation play a key role in regaining strength, mobility, and function of the ankle and lower limb after fibula fracture management. The exercises progress gradually under a physical therapist’s supervision based on the stage of bone healing, the type of treatment received, and the presence of any complications.
Initial Phase:
After splinting or casting, R.I.C.E. protocol is recommended – Rest, Ice compression, and elevation to reduce pain and swelling. Gentle range-of-motion exercises of the knee and hip help prevent joint stiffness. The therapist may also give crutches or walker assistance for safe mobility. Once the cast is removed after 6-8 weeks, physiotherapy intensifies to:
- Reduce swelling and improve blood flow: Light massage, contrast baths, pumping exercises
- Prevent muscle atrophy and weakness: Isometric contractions of the quadriceps, hamstrings and calf muscles
- Regain flexibility: Gentle stretching of the calf, hamstrings, and iliotibial band using straps or supports
- Improve proprioception: Balance and gait training on even surfaces
- Manage residual ache: TENS, ultrasound, or heat therapy
Rehabilitation Phase:
Once the fracture site has consolidated and any internal or external fixators have been removed, usually by 12 weeks, more intensive physiotherapy is initiated:
- Progressive weight bearing: Initially toe-touch, then partial weight bearing with supports, and finally full weight bearing. Each stage stretches for a few weeks based on patient tolerance.
- Active range-of-motion exercises – Close and open chain kinetic movements of the knee, ankle, and subtalar joints.
- Stretching exercises to improve flexibility
- Strengthening exercises for all lower limb muscles
- Gait training on uneven terrain
- Balance and proprioception exercises such as wobble board
- Functional skills training for stairs, squatting, and jogging
- Hydrotherapy once the wound has adequately healed
Physiotherapy continues for 3-6 months guided by periodic radiographs to monitor bone healing until pre-injury mobility and strength levels are achieved. The therapist may fabricate shoe inserts or orthoses to stabilize the realigned ankle joint as well. Home exercise programs and activity modification help prevent complications or recurrence in the long run.
Long-term recovery
The likelihood that a patient will regain full strength and motion is increased by proper treatment and rehabilitation under medical supervision. Individuals who play high-risk sports should wear the necessary safety equipment to avoid fibula fractures in the future.
Individuals can lower their risk of fracture by:
- Wearing appropriate footwear
- Maintaining a diet high in calcium-rich foods like milk
- Yogurt, and cheese
- Engaging in weight-bearing workouts
Possible complications
While most fractured fibulas heal without any further issues, the following complications can occur:
- Prolonged discomfort
- Irreversible damage to the nerves and blood vessels around the ankle joint;
- Abnormal pressure accumulation in the muscles surrounding the ankle;
- Degenerative or traumatic arthritis
- Abnormal deformity or permanent impairment of the ankle
- Chronic swelling of the extremities
Prevention of Fibula Fracture
Certain preventative measures can help reduce the risk of sustaining a broken fibula bone:
- Build bone density with weight-bearing and resistance training, adequate calcium and Vitamin D intake.
- Wear protective gear during sports – shin guards, ankle braces, sturdy shoes with cushion and arch support.
- Include balance and agility drills in fitness routines.
- Take breaks between strenuous activities to rest fatigued muscles and tendons.
- Ensure fields and walking surfaces are even and obstacle-free.
- Manage chronic medical conditions affecting bone health, such as osteoporosis, thyroid problems, or steroid use.
- Eat a nutritious diet rich in bone-healthy nutrients like protein, Vitamin C, iron, and magnesium.
- Maintain an active lifestyle with regular exercise.
- Avoid substance abuse and smoking which compromises bone structure.
- Learn proper landing techniques when jumping.
Following injury-preventive protocols decreases the likelihood of accidents causing broken lower limb bones. But prompt medical care in case an unlikely fracture occurs, helps avoid complications and supports optimal recovery.
Summary
The fibula or calf bone in the lower leg provides stability around the ankle joint and extensive muscle attachments. A fibula fracture refers to a partial or complete break across this long thin bone, typically due to excessive twisting or direct impact trauma.
It is a relatively common injury with five main fracture types based on anatomical location – the fibula head, shaft, lateral malleolus, avulsion, and stress fractures. Diagnosis involves a combination of physical exam and imaging studies like x-rays, CT, or MRI scans to locate the fracture site and guide management. Treatment modalities range from conservative casting and splinting to surgical screw fixation or external scaffolds based on fracture severity.
Physiotherapy prescribed over three progressive phases helps rehabilitate flexibility, proprioception, muscle strength, and limb function. Preventive strategies also play a role in reducing injury risk during sports and high-intensity training. While fibula fractures can certainly be painful and debilitating, timely personalized treatment aids optimal recovery and return to premorbid status.
FAQs
The fibula, a bone in the lower leg that extends from the knee to the ankle and is visible from the outside, can break as a consequence of a strong impact that causes injury. It can also break as a result of excessive strain or stress on the bone.
Whether you can recover fully at home or require surgery, physical therapy, stretching, and consistent exercises to strengthen the affected area are recommended in most cases of fibular fractures. Crutches, a walking boot, or a brace may be necessary to immobilize your lower leg.
The diagnosis of tibia and fibula fractures is made by physical examination and X-rays; depending on the kind and extent of the injury, treatment options include casting and surgery.
If a broken bone does not heal, it is referred to as a “nonunion.” Nonunions occur when the bone is not receiving enough blood flow or stability. Determining the cause of a nonunion is essential to deciding on the best course of treatment.
Complications from weight bearing and early mobility at the fracture site can occur. Fibula bone fractures heal more quickly than weight-bearing bones, including the tibia.
After a fibula fracture or any other broken ankle bone, patients should expect specific physical therapy activities such as walking instruction. Physical therapists can assist patients in starting to put weight on the afflicted leg and progressively progressing to full weight.
References
Duggal, N. (2018, December 7). Fibula Fracture: Symptoms, Treatment, and More. Healthline. https://www.healthline.com/health/fibular-fractures
Fibular Fracture. (n.d.). Physiopedia. https://www.physio-pedia.com/Fibular_Fracture
Higuera, V. (2023, July 28). What to know about fibula fractures. https://www.medicalnewstoday.com/articles/315565
Cluett, J. (2023, May 8). What to Know About Fibula Fractures. Verywell Health. https://www.verywellhealth.com/fibula-fractures-2549440
What to Know About Fibular Fractures. (2017, May 28). WebMD. https://www.webmd.com/a-to-z-guides/what-to-know-about-fibular-fractures