Shoulder Dislocation
Table of Contents
What is a Shoulder Dislocation?
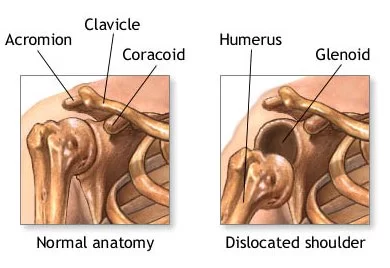
Shoulder dislocation is a common orthopedic injury characterized by the displacement of the humeral head from the glenoid fossa of the scapula. It often occurs due to trauma, such as falls, sports injuries, or accidents, leading to instability and pain in the shoulder joint.
The shoulder joint‘s unique anatomy, providing a wide range of motion but also vulnerability to dislocation, makes it particularly prone to this injury.
Shoulder dislocations can be total or partial, and they typically happen following an injury like a fall or car crash.
The humerus separates from the scapula’s glenoid at the glenohumeral joint in shoulder dislocation, which is more accurately called a glenohumeral joint dislocation. Because only a small portion of the humeral head articulates with the shallow glenoid, the shoulder joint is inherently unstable.
Being the most frequently dislocated joint in the body, this kind of dislocation accounts for 50% of all major joint dislocations.
In 95% of cases, the shoulder can dislocate anteriorly. It can also dislocate posteriorly, inferiorly, and totally or partially.
A dislocation is made more difficult by the frequently stretched or torn fibrous tissue connecting the bones.
The joint surfaces are separated during a complete dislocation.
A partial dislocation only results in a partial separation of the joint surfaces. Another name for a partial dislocation is a subluxation.
Other possible reasons for a dislocated shoulder are seizures and electrocution. The shoulder often dislocates backward after an outbreak.
Anatomy of Shoulder Joint
The three bones that make up the shoulder joint are a ball and a socket:
- The shoulder and the body are joined by the collarbone, or clavicle.
- The rounded socket in the shoulder blade (scapula) accommodates the head, or ball, of the upper arm bone (humerus). This socket is known as the glenoid. Because of the unique shapes of the glenoid and humerus, the shoulder can move in all directions.
- The shoulder is stabilized by some key structures in addition to the bones.
- The labrum encircles the shoulder socket’s perimeter. This serves as a bumper to support and maintain the correct alignment of the bones.
- Ligaments attached to the skeleton also aid in preventing shoulder dislocation.
- The ball of the shoulder is surrounded by four muscles. The rotator cuff is the collective name for these muscles. To keep the humerus in the socket, they move the arm and compress it against the glenoid.
Epidemiology
Out of all the major joint dislocations, shoulder joint dislocations occur most frequently. Anterior-superior, posterior, anterior, or inferior dislocations are possible. Both anterior and posterior shoulder dislocations are possible. The most frequent kind, though, are anterior dislocations. It stands for 95% of dislocated shoulders.
Mechanism of Injury
Excessive rotation or strong forces may cause the humeral head to separate from the glenoid labrum. Accidents involving falls, motor trauma, and contact sports injuries are common causes of dislocated shoulders.
The following reduction, the Hill-Sachs and Bankart lesions, Shoulder Anterior Dislocation,
The most common kind of dislocation is an anterior one, which is caused by the arm being held in an excessive amount of external rotation and abduction. The main barrier preventing anterior glenohumeral translation in this position is the inferior glenohumeral complex. The glenohumeral joint is particularly prone to dislocation in the 90° abduction and 90° external rotation due to a lack of ligamentous support and dynamic stabilization.
Among the complications and related injuries are:
- Immobility of the shoulder as a result of inferior glenohumeral ligament damage.
- The Hill-Sachs flaw
- Additional anterior glenolabral lesions, like a bankart lesion
- Damaged brachial plexus or axillary artery
- Dislocation of the posterior shoulder (PSD)
With only 3% of shoulder dislocations being posterior, it is a less common dislocation. Usually, the arm is abducted and the humeral head is forced posteriorly in internal rotation. Road trauma, electrocution, and epileptic disorders (the most prevalent cause in adults, often bilateral) are some of the causes. affecting more than 20% of the articular surface
Cause of Shoulder Dislocation
More often than any other joint in the body, the shoulder joint dislocates. The strained or pull apart fibrous tissue that connects the bones can exacerbate a dislocation. Only an intense force, like a blow to the shoulder, can force the bones out of their proper alignment.
The humeral head may separate from the glenoid labrum as a result of extreme rotation. Accidents involving falls, motor trauma, and contact sports injuries are common causes of dislocated shoulders. Shoulder dislocation can result from trauma suffered in falls and auto accidents.
Dislocations of the shoulder occur often. They usually arise from traumatic injuries, like those suffered in falls or car crashes. Other possible causes of a dislocated shoulder include electrocution and epileptic attacks.
The most frequent way for the shoulder to dislocate is by sliding anteriorly, or forward, out of the socket. This happens when the arm is raised away from the body and the shoulder dislocates.
Another way to dislocate the shoulder is to slide posteriorly, or backward. This might happen if the arm is raised in front of the body and the shoulder dislocates. The shoulder often dislocates backward after a seizure.
Clinical Symptoms of Shoulder Dislocation
Anterior Dislocation: the humeral head shifts to lie anteriorly, medially, and slightly inferiorly relative to the glenoid fossa and its normal position.
After an acute dislocation of the anterior glenohumeral:
- Arm raised to the ER position and held abducted
- Loss of the acromion’s and deltoid’s typical contour is noticeable laterally and posteriorly
- Anteriorly palpable humeral head
- Every motion is painful and restricted.
- perceptible fullness beneath the coracoid process and towards the axilla
- Possible damage to the bone and muscles of the rotator cuff.
- Traction of the axillary blood vessels can cause vascular injuries, which may appear as a drop in pulse rate or a temporary feeling of coldness in the hands.
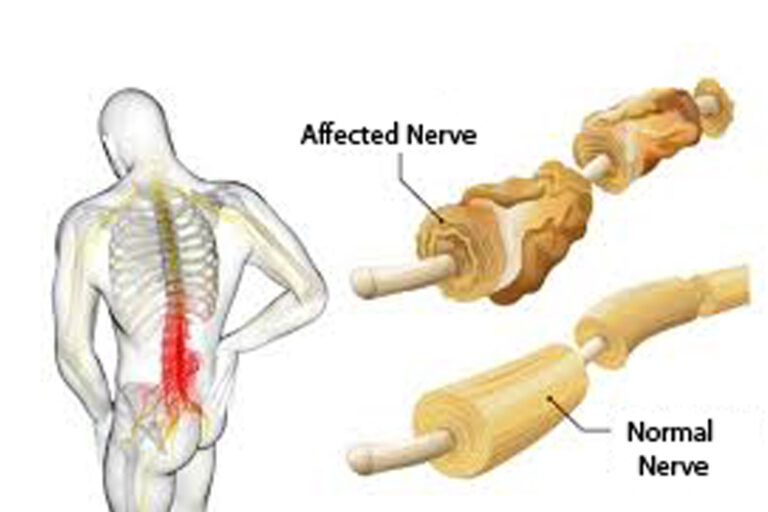
- Traction of the brachial plexus often results in injuries to the peripheral nerves.
Posterior Dislocation
Having an acute dislocation of the posterior glenohumeral:
- The arm is taken off, and the IR
- Possible loss of deltoid outline
- possibly observe posterior prominence humerus’s head
- weakness or inability to internally rotate due to a rupture in the subscapularis muscle
- Posterior shoulder instability may result from associated glenolabral and capsular injuries, even though neurovascular damage is rare.
Due to the difficulty of reducing posterior dislocations, closed reduction procedures must be carried out in consultation with the treating orthopedic surgeon. Closed reduction is not recommended if the shoulder dislocation occurred more than three weeks ago (which is common in elderly patients who lack physical strength) or if there is a reverse Hill-Sachs defect
Examination
Medical history
Medical history review and physical examination, Your physician must be aware of the cause of the dislocation as well as previous shoulder dislocations.
Upon examining your shoulder, the physician will:
- Examine for deformity, swelling, and discomfort.
- Examine the skin and circulation in the arm, taking note of the wrist pulses. Should an artery sustain damage during the dislocation, the hand will feel cool to the touch and could appear white or purple. The hand’s inability to receive warm blood is the cause of this.
- Verify the arm’s and shoulder’s nerve supply. If the dislocation caused damage to nerves, part or all of the shoulder and arm may become numb and immobile.
Imaging Examinations
To determine whether there is a bone injury, an X-ray is required. X-rays can also be used to help determine the dislocation’s direction.
- The best method to verify that the shoulder is dislocated is through X-rays.
- When identifying bone detail on an X-ray proves to be challenging, the physician might prescribe a computed tomography (CT) scan.
- Frequently, it’s important to assess the ligaments, and an MRI scan can be useful in this regard. When the dislocation occurs, an MRI is not usually necessary.
Upon confirmation of the dislocation by X-ray, the physician will set (reduce) the shoulder. If an MRI or CT scan is required, it may not be requested until after the dislocated shoulder has been realigned. Usually, these tests are carried out following that.
Physical examination
Observation:
First, a physician will look at the patient’s general posture and the way the damaged arm is positioned. The most common kind of dislocation, an anterior one, usually requires holding the arm slightly abducted and externally rotated. This indicates that the hand is turned outward and the arm is away from the body.
The arm will be maintained internally rotated and adducted in the less typical condition of a posterior dislocation. This indicates that the hand is turned inward and the arm is near to the body
Palpation:
- To feel pain, edema, and deformity in the shoulder, the medical practitioner will lightly touch it. One may feel a depression on the back of the shoulder and a lump on the front in the event of an anterior dislocation.
- Additionally, the medical expert will feel for particular bony landmarks, such as the coracoid process, a little hook-shaped bone near the front of the shoulder blade, and the acromion process, The point of bone in the upper part of the shoulder blade.
Testing the range of motion
- The medical practitioner will carefully move the arm through its range of motion to check for pain and movement restrictions. The range of motion will be painfully limited in the event of a dislocation.
Examination of the nervous system
To check for any injury to the nerves or blood vessels, a healthcare professional will feel and move the arm and hand. This is crucial because a dislocated shoulder may sometimes damage the blood vessels or nerves that are close to the joint.
Differential Diagnosis
- Fracture of the humeral head, proximal humerus, glenoid, clavicle, and greater tuberosity
- Rheumatoid Arthritis Joint
- Injury to the Rotator Cuff
- Dislocation of the Acromioclavicular Joint
- Pathology of Labral Organs
- Subluxation of the Shoulders
- Palsies of the Axillary and suprascapular nerves
Treatment of Shoulder Dislocation
A dislocated shoulder needs to be treated as an emergency. The objective of promptly managing a dislocated shoulder is to reposition the shoulder to its typical position. Restoring the arm’s function is the ultimate objective.
Non-Surgical Care
Closed-off decrease. In a hospital emergency room (ER), the shoulder can usually be realigned to its normal position. The patient will typically receive sedatives and painkillers before this procedure. A closed reduction is the process of realigning the shoulder. It is carried out slowly and gently. When a shoulder dislocation happens during a sporting event, medical professionals might be able to realign the shoulder at the scene.
Closed Reduction: A medical professional in the ER will try to reposition the moved bone. To reduce pain and discomfort, this closed reduction procedure is frequently carried out under local anesthesia or sedation.
Immobilization. A sling is used to keep the shoulder motionless once it has been reduced to its proper position. By doing this, the shoulder is protected from additional harm. You should wear the splint until you see a doctor again. To allow the tissues to heal and stabilize the joint, the doctor will probably immobilize your arm with a brace or sling for a few weeks following a successful reduction.
Your doctor will examine your shoulder at your follow-up appointment and decide if further information is required. If so, they might now request an MRI or CT scan.
Surgery may not be necessary to treat a shoulder dislocation if the shoulder is not severely damaged.
Ice. To reduce pain and swelling, the affected area can be iced three or four times a day. Avoid putting ice right on your skin. Towel-wrap the ice or use an ice pack.
Drugs for pain. Pain and swelling can be lessened with the use of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen.
Rehabilitation. Physical therapy can be beneficial while you’re recovering. Strengthening the muscles and restoring the shoulder’s range of motion are two benefits of physical therapy. Additionally, rehabilitation may help avoid future shoulder dislocations.
The first exercise in the rehabilitation process will be mild muscle toning. Weight training can be added later.
Following a shoulder dislocation, some people can resume their full range of activities. Even after receiving physical therapy, some people still experience a sensation that their shoulder is sliding out of place. For specific activities, these patients may wear a brace to help protect their shoulders.
Physical Therapy treatment
Physical therapy is a must for shoulder dislocation recovery. It helps to:
- Minimize pain and inflammation: During the early phases of healing, pain and inflammation can be managed with the use of techniques like electrical stimulation, heat therapy, and ice therapy.
- Restore range of motion: To help you regain your shoulder joint’s full range of motion, gradually introduce gentle stretching exercises.
- Improve stability and strength: Exercises aimed at strengthening the muscles surrounding the shoulder joint are important for stabilizing the joint and preventing further dislocations.
- Boost your body’s awareness of its physical position, or proprioception. Your sense of joint position and movement can be improved with proprioceptive exercises, which are helpful for coordinated movement and injury prevention.
- Reduce a dislocated shoulder as soon as possible. In the Emergency Department, this is typically done after sedation and suitable analgesia. There are several methods for lessening the shoulder.
Anterior Dislocation
To allow for proper capsular healing, ASDs are typically treated with closed reduction and a period of immobilization (e.g., six weeks). A structured physical therapy program is necessary to minimize muscle atrophy and preserve mobility to promote healing and eventually return to normal function. Isometric shoulder muscle exercises are essential during immobilization. For dislocation treatment complications and related injuries, surgery might be necessary.
There is a lot of variation in the length of the post-operative immobilization period and the introduction of each type of exercise after traumatic ASD. There is an absence of evidence to direct post-operative rehabilitation as well as research comparing the effectiveness of various rehabilitation programs. This variability is partially due to diverse populations presenting with ASD and recent advancements in surgical procedures. Wang and associates proposed a three-step procedure:
Phase 1 (up to 6 weeks) Immobilization. Preserving anterior-inferior stability is the aim.
Although it has historically been believed to be immobilized with internal rotation, Miller maintains that because there is greater contact force between the glenoid and the labrum in external rotation, immobilization has been advantageous.
- Immobilization at 10 degrees of external rotation appears to have a lower recurrence rate than internal immobilization at 10 degrees, according to researchers.
- As of right now, there is no agreement on how long being immobilized in a sling should last.
- The average length of time spent in a sling is 1-2 weeks for those over 40 and 3-6 weeks for those under 40.
- AROM of the elbow, wrist, and hand as well as pain management are the main goals during the immobilization phase. It is possible to include isometric exercises for the rotator cuff and biceps muscles. For example, the Codman Exercises and AAROM for forward elevation (0-90º) and external rotation (0-30º)
The main goals are to control pain, lower inflammation, and stop additional injuries.
Interventions:
- Rest and immobilization: To help the joint heal, your arm may be immobilized in a sling for a short duration of time.
- Ice therapy, also known as cryotherapy, is useful in lowering pain and inflammation.
- Electrotherapy: Methods such as electrical stimulation or ultrasound can help relieve pain while helping with healing.
- Mild isometric exercises help maintain muscle strength without putting excessive pressure on the healing tissues. They include contracting muscles without moving the joint.
Phase 2 (6–12 weeks): Restoring appropriate motion, particularly in external rotation, is the aim.
Focus: Expanding the shoulder joint’s range of motion gradually.
Interventions:
- Exercises for passive range of motion: To help increase flexibility, a physiotherapist will slowly move your arm through its range of motion.
- Active-assisted range-of-motion exercises: Your physiotherapist will progressively assist you in performing these exercises.
- Maintaining mild isometric training
- When stretching is allowed, use joint mobilizations or self-stretching to passively stretch the posterior joint capsule to reach its full range of motion (AAROM).
- Waiting to begin strengthening or repetitive exercises until a full range of motion is achieved is advised
Phase 3 (12–24 weeks): Achieving a successful comeback to daily physical activities or sports
Goals: Increasing proprioception and strengthening the muscles surrounding the shoulder joint.
Interventions:
- Exercises for progressive strengthening: To strengthen and stabilize your shoulder muscles, you will progressively move on to harder workouts.
- Exercises that help you regain your sense of joint position and movement are called proprioceptive exercises.
- Functional exercises: You’ll start to practice using your shoulder in everyday activities.
- Start doing strengthening exercises; these should be specific to the individual’s impairment.
- Start your strengthening exercises with stability exercises in a pain-free motion.
- The rotator cuff muscles and scapular stabilizers, such as the trapezius, serratus, levator scapulae, and rhomboids, could be the first areas of focus for a potential progression. Next, move on to the larger muscles, including the pectorals, latissimus dorsi, and deltoids.
- Start concentrating on functional exercises, such as proprioceptive training, and modify them to promote the patient’s engagement in social activities.
- Also, see Going Back to Play in Sports
Posterior Dislocation
With the following exceptions, the anterior protocol’s progression for managing posterior dislocation is as follows:
- Posterior glide is not recommended.
- Avoid flexion when internal rotating and adduction.
- If you are younger than 40, you will be immobilized for 3-6 weeks. If you are older than 40, you will be immobilized for 2-3 weeks.
- The posterior musculature, including the teres minor, posterior deltoid, and infraspinatus, will be the main focus of your strengthening exercises.
- Also, see Going Back to Play in Sports
Surgical Treatment of Shoulder Dislocation
Surgery might be necessary if the shoulder joint cannot be rearranged or has dislocated more than once. Surgery is frequently required for a dislocated shoulder if there are injuries to the shoulder’s musculature or bones.
Based on the extent of the injury, surgical procedures could involve:
- Ligament tightening or repair
- Repairing labrum damage
- Filling gaps in bone
- Bone regrowth
- Certain surgical procedures are better suited for specific individuals.
Following a first dislocation, some patients, especially young athletes, may require surgery to help prevent further dislocations (chronic shoulder instability). Your surgeon will go over your risk factors for recurrent shoulder dislocations with you and weigh the advantages and disadvantages of surgery versus nonsurgical treatment.
Following surgery, a degree of shoulder stiffness is possible.
Following surgery, physical therapy is important for assisting in the restoration of range of motion.
Maintaining proper muscle strength and control in your shoulder and shoulder blade muscles is important, regardless of whether you receive nonsurgical treatment or surgery. This can lessen your chance of experiencing another shoulder dislocation in the future (chronic shoulder instability) and help you heal more quickly from a dislocation.
Re-dislocation risk factors:
- Previous dislocation accompanied by lax soft tissue or poor tissue healing
- Because they are more active, younger patients experience re-dislocation much more frequently.
- Re-dislocation is more common in patients with glenoid fractures or torn rotator cuffs.
Some other risk factors:
- Previous Dislocation: The single largest risk factor for re-dislocation of the shoulder is having previously experienced a dislocation. During the first dislocation, the tissues and ligaments holding the shoulder joint in place are stretched or torn, which weakens them and increases their susceptibility to further injuries, particularly in younger people.
- Age: Compared to older persons, younger people (between the ages of 15 and 30) have a larger chance of experiencing re-dislocation. Younger people’s ligaments are more flexible than those of older people, which makes them more prone to tearing and stretching.
- Participation in Contact Sports: Because contact sports involve high-impact movements, athletes who play football, rugby, or hockey are more likely to suffer a dislocated shoulder. Another factor raising the risk is repetitive strain on the shoulder joint from throwing or overhead motions in sports like basketball, tennis, and baseball.
- Loose Ligaments (Ligamentous Laxity): People who have loose ligaments in other parts of their bodies—not only the shoulder—are more likely to experience dislocations and instability in their joints.
- Weakness in the Rotator Cuff: The rotator cuff muscles aid in stabilizing the shoulder joint. These muscles’ weakness may aggravate shoulder instability and raise the possibility of re-dislocation.
- Bone Impingement: A slight depression or impaction on the bone may occasionally result from a fracture in the humeral head bone, or upper arm bone, caused by the initial dislocation. This may press against the socket, raising the possibility of further dislocations.
- Insufficient therapy: To strengthen the muscles and ligaments surrounding the shoulder joint and increase joint stability, it is important to receive proper care following an initial dislocation. Re-dislocation risk may increase if rehabilitation exercises are skipped or performed insufficiently.
Prevention
Maintaining Strength and Flexibility:
- Regular Exercise: Strengthening and stabilizing the shoulder joint can be achieved by regular exercise regimens that focus on the rotator cuff, surrounding upper back, and chest muscles.
- Stretching: Performing regular stretches helps to increase the flexibility of the muscles surrounding the shoulder joint, which lowers strain and the risk of tearing them during motions.
Taking Part in Activities in a Secure Way:
- Proper Technique: To reduce stress on the shoulder joint, make sure you employ the correct technique if you play sports or engage in other activities that require strong arm motions. If necessary, seek professional advice.
- protection Gear: As advised by a healthcare provider, wear the proper protection gear, such as shoulder pads or braces, when participating in high-risk activities like contact sports or activities that could result in falls.
- Return to Activities Gradually: To promote healing and avoid reinjury, increase activity levels and intensity gradually following a shoulder injury.
Taking Care of the Underlying Conditions
- Ligament Laxity: See a medical expert about bracing or exercises that might help support joint stability if you have naturally loose ligaments.
- Seeking Treatment for Rotator Cuff Weakness: Improving shoulder stability and lowering the risk of dislocation can be achieved by treating rotator cuff weakness with physical therapy or targeted exercises.
Complication
- Soft tissue damage: The muscles, tendons, and ligaments that surround the joint may be broken stretched, or otherwise harmed by the force of the dislocation. Shoulder pain, weakness, and instability may result from this.
- Nerve damage: In serious cases, a dislocation may cause harm to the nerves supplying the arm’s movement and sensation. This may result in hand and arm weakness, tingling, and numbness.
- Damage to blood vessels: Although it is uncommon, a dislocation can harm the blood vessels supplying the arm with blood. Negative effects like gangrene and tissue death may result from this.
- Recurrent dislocations: You run a higher risk of further shoulder dislocations after you’ve already experienced one. This is due to the possibility of stretched or stretched ligaments and other supporting structures, which would reduce the stability of the joint.
- Post-traumatic arthritis: This type of arthritis can develop over time as a result of repeated dislocations or cartilage damage to the joints. This is a painful disease that can result in shoulder pain, stiffness, and restricted range of motion.
Prognosis
When given the right care and rehabilitation, the majority of people with a shoulder dislocation have a good prognosis and recover fully. However, some variables, such as the following, might affect the healing process and long-term results:
- The severity of the dislocation: Recovery time and possible problems may be affected by the degree of ligament and tissue injury, as well as any accompanying bone fractures.
- Age: Because of increased ligament laxity, younger people (under 30) usually have a higher risk of re-dislocation than older adults.
- Past dislocations: The likelihood of future re-dislocations is much increased in those with a history of shoulder dislocations.
- Treatment observation: For the best possible outcome and to avoid difficulties down the road, you must follow the prescribed treatment plan, which includes physical therapy exercises.
the normal period for recovering from a dislocated shoulder:
- Emergency medical care: This includes X-rays to confirm the dislocation, pain management, and joint repositioning by a medical specialist.
- Immobilization: Putting on a brace or sling for a few weeks, usually one to four, to give the joint time to mend and stabilize.
- Physical therapy: Performing rehabilitation activities to restore shoulder joint strength, range of motion, and flexibility. This usually takes a few weeks to months, depending on how well each person is progressing.
- Return to normal activities: With appropriate supervision and approval from a healthcare provider, a patient can gradually resume everyday activities and sports engagement, usually within three to six months.
positive results
- complete regaining of range of motion and shoulder function
- Capacity to resume most or all activities, sports included
- Minimal to no long-term complications
Conclusion
A common injury is a shoulder dislocation, which occurs when the upper arm bone’s ball, or humeral head, pops out of the glenoid, the shoulder joint’s socket. Even though it’s usually manageable, getting the right medical care is still necessary because it might hurt.
When acceptable rehabilitation and immediate medical attention are received, the prognosis for a dislocated shoulder is generally positive. The majority of patients who dislocate their shoulder recover completely and can use their shoulder normally.
The outlook has been broken down as follows:
- Recovering from a shoulder dislocation usually takes 6 to 12 weeks, but it can take longer based on some factors, including the severity of the injury.
- Complete recovery: With the right therapy, the majority of patients regain their full range of motion and shoulder strength.
- Recurrence risk: Younger people and athletes who participate in contact sports are more susceptible to re-dislocation.
- Problems: Although rare, complications such as blood vessel damage, nerve damage, and post-traumatic arthritis can arise from improper treatment of the dislocation or repeated dislocations.
FAQs
Grip your damaged arm by the wrist whether you’re seated or standing. Straighten and extend your arm in front of you. The purpose of this is to reposition the ball of your arm bone into the shoulder socket. Put your arm in the sling once the shoulder has realigned.
The most common dislocation in the body occurs in the shoulder, which can dislocate anteriorly, posteriorly, inferiorly, or anteriorly-superiorly. The majority of places are anterior. Redislocation is more common in patients with a history of shoulder dislocation.
Five main causes can result in a dislocated shoulder: sports injuries, falls, impact injuries, repetitive stress injuries (RSIs), and “loose ligaments.” Sports and athletic activities are the most common causes of shoulder dislocations, especially those that call for frequent, powerful shoulder use.
The following are potential effects of a dislocated shoulder: tearing of the shoulder joint’s supporting tendons, ligaments, and muscles. injury to the blood vessels or nerves in or near the shoulder joint. increasing the likelihood of recurring dislocations, particularly in cases of severe damage
After a few days, you can take off the sling, but a dislocated shoulder takes 12 to 16 weeks to fully heal. In two weeks, you should be able to resume most activities. For a period of six weeks to three months, you should stay away from doing strenuous lifting or taking part in shoulder-intensive sports.
Immobilization and Icing Pain and inflammation can be reduced and eased by resting the shoulder and applying an ice pack. To let the muscles and other soft tissues to rest and recover, doctors advise immobilizing the affected arm and shoulder for four to six weeks with a sling or brace.
You’ve likely stretched or ripped a few of the shoulder joint’s ligaments, tendons, or muscles. Ligaments are the structures that bind bone to bone. Your arm is kept in place by all of these tissues. A dislocated shoulder causes severe pain. It is quite difficult to move your arm.
Grade 1: This type of injury involves spraining or stretching the capsule that covers the joint, but there is no harm to the ligaments that attach the clavicle to the shoulder blade (scapula). Although the bump is temporary, there can be edema around the joint. The pain typically goes away after two to four weeks, although it might break up again quickly.
Teenage boys and young men in their 20s are more likely to have shoulder dislocations because they participate in strenuous activities that increase the risk of injury, such as playing contact sports like football or hockey.
Usually, a dislocation can be repaired by popping it back into position without the need for surgery. On the other hand, those who experience frequent dislocations and chronic instability might require surgery to address the problem.
An MRI termed an MR arthrogram should be done if the dislocated shoulder is chronic or has happened more than once. Based on the findings of the scans, an orthopedic physician will design the best course of action and decide if surgery is necessary.
fitness regimens that are difficult or painful.
exercises that place all of your body weight on your shoulders, such as raises, rows, and pull-ups. heavy object lifting
References
- Shoulder Dislocation – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/dislocated-shoulder/
- Shoulder Dislocation. (n.d.). Physiopedia. https://www.physio-pedia.com/Shoulder_Dislocation